Navicular Fracture
Introduction
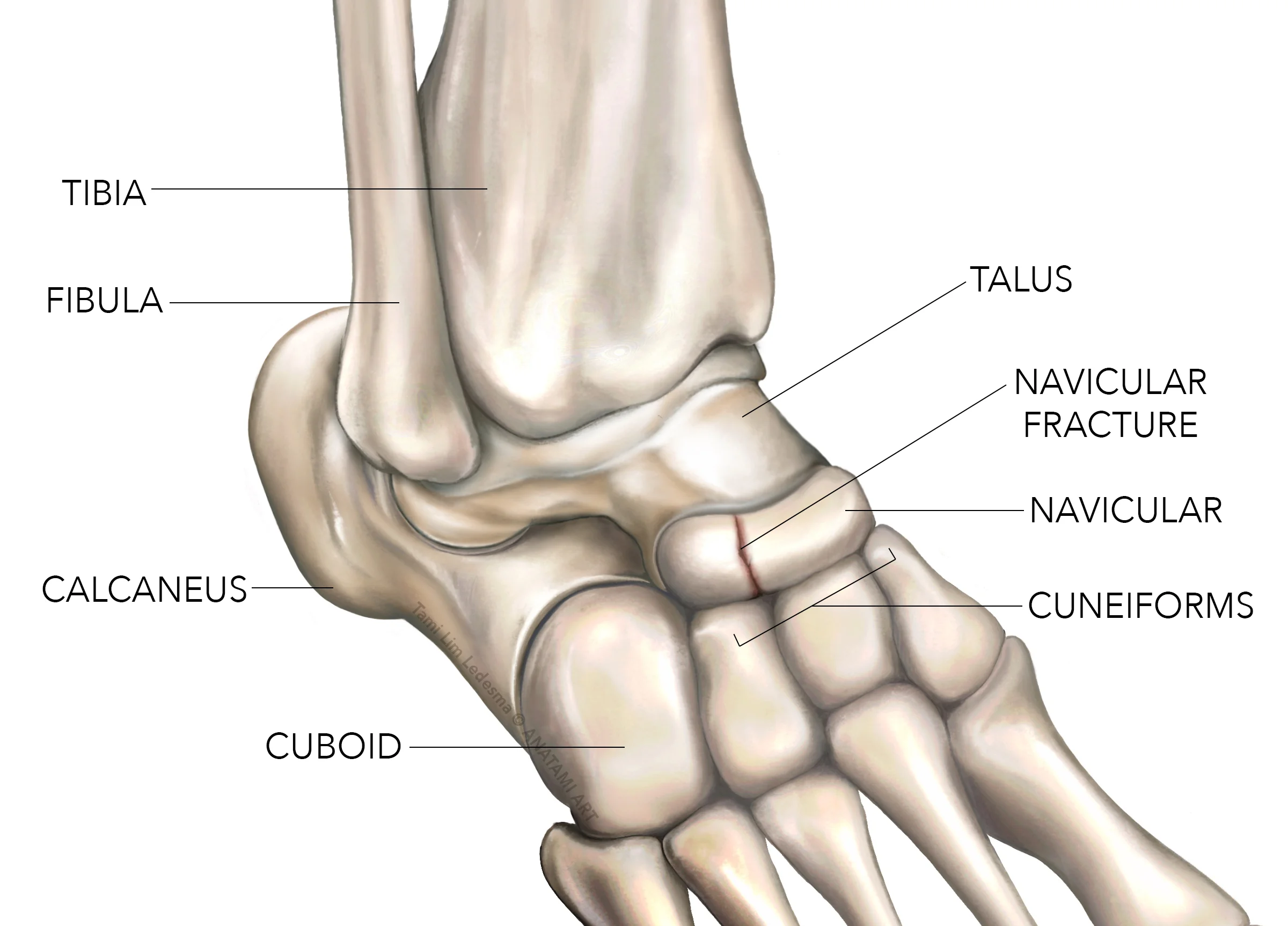
A navicular fracture is a partial or complete crack in the navicular bone, one of the tarsal bones in the midfoot. Navicular stress fractures are caused by repetitive overloading of the bone, which overcomes its structural integrity.
If not properly treated, navicular stress fractures can disrupt blood supply and lead to nonunion, delayed union, or avascular necrosis (AVN). These complications make navicular fractures one of the most difficult foot injuries.
Anatomy & Biomechanics
The navicular bone is centrally located in the midfoot medial to the cuneiform bones. It articulates proximally with the talus, forming the talonavicular joint, and distally with the three cuneiform bones. The navicular serves as a keystone that transmits forces from the talus to the lateral, medial, and intermediate cuneiform bones during gait.
The blood supply to the navicular enters via the dorsal tarsal artery proximally and the plantar artery distally. This leaves the central two-thirds of the bone with relatively poor perfusion, making it vulnerable to disruptions in blood flow after injury.
During the stance phase of gait, body weight is transmitted along the medial longitudinal arch, placing the navicular under significant compressive loads. As the arch lowers and the midfoot pronates, the navicular also descends and rotates. This motion “locks” the midfoot to create a rigid lever for efficient push-off.
The biomechanics of the navicular bone are complex. Repetitive loading during activities like running and jumping can generate forces up to 2-3 times body weight on the navicular.
Over time, these cumulative loads can overwhelm the structural integrity of the bone, resulting in a stress fracture. This typically starts as a partial crack in the central waist of the navicular before progressing to a completed fracture.
Navicular Fracture Classification
Several classification systems have been developed to categorize navicular fractures based on fracture pattern, location, and degree of displacement. These help guide treatment options and predict prognosis.
Gehr’s Classification divides navicular fractures into three main types:
1. Type I – Undisplaced fracture of the middle third of the navicular body
2. Type II – Fracture extending through the proximal articular surface involving the talonavicular joint
3. Type III – Comminuted fracture of the entire navicular bone
Torg’s Classification categorizes navicular stress fractures more specifically based on location:
1. Type I – Fracture of the dorsal cortex distal to the talonavicular joint
2. Type II – Fracture extending proximally from the central third into the talonavicular joint surface
Sangeorzan’s Classification grades the degree of navicular fracture displacement:
1. Grade 1 – Nondisplaced or minimally displaced (<2 mm)
2. Grade 2 – Displaced fracture with less than 50% contact between fragments
3. Grade 3 – Displaced fracture with no contact between fragments
Types of Navicular Fractures
There are several common types and patterns of navicular fractures:
- Transverse mid-body fractures are the most common, caused by tension on the plantar ligament
- Oblique or spiral fractures can occur through the waist or from proximal medial to distal lateral
- Comminuted fractures involve multiple bone fragments, often from compression
- Avulsion fractures can occur from ligamentous attachments to the navicular tuberosity
- Stress fractures start as tiny partial cracks from chronic overuse that then progressively worsen
The classification and pattern of navicular fracture impact healing potential as well as guide appropriate treatment to try and preserve navicular function. However, navicular fractures have high risks for delayed union, malunion, and avascular necrosis even with proper management.
Signs & Symptoms
- Pain – The most common symptom is progressive midfoot pain aggravated by weight-bearing activities. The pain is well localized over the navicular bone. It often starts as mild discomfort that increasingly worsens over time.
- Swelling – Diffuse swelling occurs over the medial midfoot area overlying the navicular. Swelling is often more prominent after activity.
- Tenderness – Exquisite point tenderness can be elicited with palpation directly over the navicular tuberosity.
- Antalgic Gait – Patients often limp or walk on the lateral foot edge to avoid pressure under the navicular.
- Load Test Pain – Having the patient stand on their toes often produces intense focal pain.
- First Step Pain – Pain with the first step of walking after a period of rest is also characteristic.
Diagnosis
Due to vague symptoms and initially normal radiographs, the diagnosis of navicular fractures is often significantly delayed. MRI and bone scan are the most sensitive tools for confirming a suspected navicular stress fracture.
- Radiographs – X-rays often appear normal initially. Findings like bone resorption, haziness, cystic changes, or an obvious fracture line indicate late changes.
- MRI – MRI has over 95% sensitivity for identifying bone marrow edema associated with navicular stress fractures within the first week of symptom onset. This allows early diagnosis.
- CT Scan – CT provides greater bony detail compared to plain films to assess fracture displacement and comminution.
- Bone Scan – Though less sensitive early on, bone scans have nearly 100% specificity. Increased uptake on delayed images is diagnostic.
Once the fracture is diagnosed, further imaging helps classify location and severity to guide appropriate treatment. Given the risks of complications like nonunion and AVN, early diagnosis is vital to prevent disease progression and chronic impairment.
Treatment of navicular fractures:
The goals of treating navicular fractures are to promote bone healing while preventing complications like nonunion, malunion, and avascular necrosis. This requires protecting the fracture to allow for appropriate revascularization and ossification. Treatment principles include immobilization, non-weight bearing, and potentially surgery.
Immobilization
- Casting – Initial treatment typically involves a below-knee cast or walking boot immobilizing the ankle in a neutral position to offload the navicular fracture. This needs to be worn for 6-8 weeks until evidence of fracture healing.
- Non-Weightbearing – Strict non-weight bearing is essential during immobilization to facilitate healing. Up to 3 months of protected weight-bearing is recommended following immobilization based on serial imaging.
- Bone Stimulators – Electrical or ultrasound bone stimulators may be used as adjuncts during immobilization to accelerate bone healing. However, efficacy remains uncertain.
Surgery
Surgical fixation is considered for displaced or unstable fracture patterns, especially those with >50% joint surface involvement or >2 mm displacement. Open reduction and internal fixation help restore anatomic alignment while providing compression across the fracture fragments to stimulate healing. Screw fixation helps maintain reduction during the healing process.
Post-Operative Protocol
If surgery is performed, the patient is typically immobilized for 6 weeks followed by progressive protected weight-bearing over 3 months postoperatively. Serial CT scans help assess fracture alignment and healing.
Complications and Salvage Procedures
For cases progressing to nonunion or osteonecrosis, salvage procedures may be considered. Bone grafting adds osteogenic cells and scaffolds to stimulate healing. Osteotomies and joint fusion procedures may also be required for severe cases refractory to other measures. Despite treatment, outcomes following navicular fractures have up to a 30% risk of poor long-term function.
In summary, a period of non-weight bearing in a cast or brace is the standard initial treatment for all navicular fractures to promote healing. Surgical fixation, bone grafting, joint salvage, and osteotomies may be utilized for complex cases or treatment failures. Rehabilitation requires at least 6 months with a gradual return to weight-bearing activities.
Complications
Navicular fractures have a high rate of complications even with appropriate management. These include:
- Delayed Union or Nonunion: Up to 24% of navicular fractures may progress to nonunion due to the tenuous blood supply. Nonunions occur when the fracture fails to heal properly over an extended timeframe.
- Avascular Necrosis (AVN): Disruption of the blood flow to the navicular can lead to death of the bone tissue, termed avascular necrosis. The rate of AVN is up to 73% following navicular fractures.
- Post-traumatic Arthritis: Fractures into the talonavicular or other navicular joint surfaces frequently cause arthritis long-term due to cartilage injury and joint surface incongruity from malunion.
- Chronic Pain: Persistent pain during activity and weight-bearing is common after the fracture heals due to residual stiffness, arthritis, AVN bone collapse, and discomfort at the fracture site.
Outcomes & Prognosis
The prognosis following navicular fractures largely depends on the development of complications:
- If the fracture heals without complication, patients can generally expect to regain normal or near-normal function without long-term impairment. However, post-traumatic arthritis can still occur.
- With complications like AVN or nonunion, outcomes are significantly worse with high risks of chronic pain and impaired foot mechanics. Additional procedures are often necessary to try to address complications.
- One systematic review found that as many as 33% of competitive athletes sustaining navicular fractures have persistent symptoms prohibiting return to sports even after the fracture has radiographically healed.
- Another study indicated that 45% of patients have persistent pain during activities at a 2-year follow-up, suggesting relatively frequent long-term morbidity.
Overall, outcomes are better if the navicular fracture heals without complication within the first 3 months after injury. However, patients should be counseled that navicular fractures have relatively high risks of delayed healing, AVN, and post-traumatic arthritis, which can result in chronic pain and functional limitations. Close follow-up is necessary to monitor for early complications.
Rehabilitation
The goals of rehabilitation after a navicular fracture are to reduce swelling and pain, prevent complications, regain mobility/strength, and promote a safe return to activities. Rehab principles include:
- Early Phase (0-6 weeks): Fracture protection and pain/swelling management. Use a boot/cast and abide by weight-bearing restrictions. Gentle range of motion exercises can reduce stiffness. contrast baths, massage, and elevation help control swelling.
- Intermediate Phase (6-12 weeks): Gradually increase weight bearing and initiate strength training. Wean into a stiff-soled shoe and progress weight bearing using a directed program over 6-12 weeks. Begin intrinsic foot muscle exercises. Use anti-inflammatories to control residual pain. Consider ultrasound bone stimulation.
- Late Phase (3-6 months): Advance strength and balance exercises. Perform single-leg balance activities. Use resistance bands to strengthen foot intrinsics and gastroc/soleus complexes. Tilt boards can improve proprioception. Stretching and joint mobilization reduces stiffness.
- Return to Play Phase: Sport-specific drills and a gradual return to activities once fully healed. Time frames for returning range from 6 months for walking/hiking up to a year for high-impact sports depending on the sport and player/fracture characteristics.
Prevention
Navicular stress fractures most commonly occur from overuse. Prevention strategies focus on load management and include:
- Allowing adequate rest between workouts
- Cross-training to vary repetitive impact
- Monitoring sudden changes in activity levels
- Optimizing biomechanics and foot architecture
- Wearing appropriate shock-absorbing shoes
- Considering custom orthotics to reduce load
- Strengthening the intrinsic muscles of the foot
Adherence to load management programs helps mitigate overuse injury risk. However, navicular fractures can still occur in a traumatic fashion from an acute overload event. Unfortunately, these cannot be prevented through training programs and reliance is on appropriate diagnosis and management after the injury event.
Summary
- Navicular fractures involve a partial or complete crack in the navicular tarsal bone located on the medial midfoot
- They account for up to 35% of midfoot fractures and are caused by repetitive overloading, leading to structural failure
- The navicular plays an integral role in midfoot function, transmitting forces from the ankle to the medial longitudinal arch
- Its blood supply comes from the tarsal sinus proximally and plantar artery distally, making the central navicular vulnerable to interruptions in circulation after fracture
- Displaced, comminuted fractures have a higher risk of delayed union, nonunion, and avascular necrosis (AVN) which can lead to post-traumatic arthritis
- Patients typically present with progressive midfoot swelling and pain, especially with weight-bearing activities
- Plain films may appear normal initially. MRI and bone scan offer the best sensitivity for early diagnosis
- Most navicular fractures are treated non-operatively with a period of non-weight-bearing cast immobilization
- Surgical fixation is considered for fractures that are significantly displaced or involve the joint surface
- Rehabilitation focuses on managing swelling and pain in the early phases, followed by a gradual return to weight-bearing and strength training
- Complications like nonunion, AVN, and arthritis are not uncommon even with appropriate treatment
- Recovery takes over 6 months on average and up to 33% of athletes may not return to sports due to persistent symptoms
FAQS
How are navicular fractures caused?
Navicular fractures occur from repetitive overloading, typically in the setting of increased activity levels. Stress reactions weaken the bone over time before progressing to partial and complete fractures.
How is a navicular fracture diagnosed?
X-rays may appear normal initially. MRI and bone scan offer the greatest sensitivity and can help diagnose navicular fractures within 1-2 weeks of symptom onset.
How are navicular fractures treated?
Most navicular fractures are treated non-operatively with a below-knee cast or boot for 6-8 weeks and strict non-weight bearing. Surgical fixation is considered for significantly displaced or intra-articular fractures.
What is the prognosis following a navicular fracture?
If the fracture heals without complication within 12 weeks, patients often regain full function. However, complications like AVN and nonunion seen in up to 45% of cases can result in long-term morbidity with pain and arthritis.
What is the prognosis following a navicular fracture?
Preventative strategies focus on load management, including allowing adequate rest between workouts, cross-training, monitoring changes in activity levels, optimizing biomechanics, and wearing appropriate shock-absorbing footwear.
REFERENCES
- Ameres, M. J. (n.d.). Navicular Fracture: Practice Essentials, Epidemiology, Functional Anatomy. https://emedicine.medscape.com/article/85973-overview?form=fpf
- Gheewala, R. (2023, July 10). Tarsal Navicular Fractures. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK542221/
- Clinical Practice Guidelines : Navicular Fractures – Emergency Department. (n.d.). https://www.rch.org.au/clinicalguide/guideline_index/fractures/Navicular_Fractures_-_Emergency_Department/