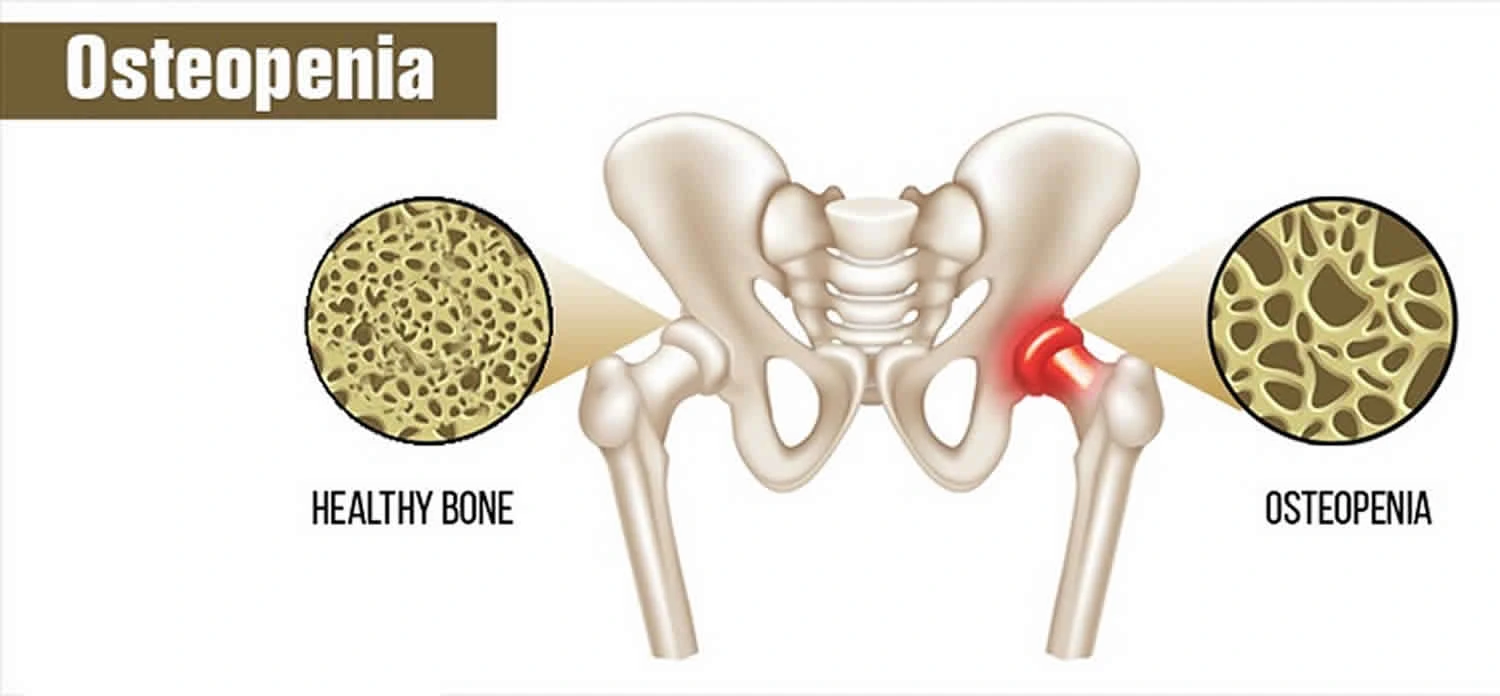
Osteopenia
What is Osteopenia?
Osteopenia is a loss of bone mineral density or BMD. Lower BMD suggests you have fewer minerals in your bones than you should, which creates bones weaker. By description from the World Health Organization osteopenia is described by bone densitometry as a T score of -1 to -2.5.
Epidemiology
Worldwide, Asia has noted the lowest average t-scores by area. Overall, women have a four-fold higher overall majority of osteopenia compared to men. Australia noted an incidence rate of osteopenia in 42% of males and 51% of females. India noted a 52% overall incidence among its residents in 2005. In the United States, 54% of postmenopausal females are osteopenic.
What causes osteopenia?
Bones are created of living tissue. Up until around age 30, a healthy person builds more bone than he or she loses. But after age 35, bones start to break down quicker than they build up. Actually, in healthy people, bone density declines throughout life, by less than 1 percent per year.
Some items can create bone loss to occur more fast, leading to osteopenia, like:
Medical diseases like hyperthyroidism.
Drugs such as prednisone and some therapies for heartburn, cancer, high blood pressure, and seizures.
Hormonal modifications during menopause.
Poor nutrition, specifically a diet too low in calcium or vitamin D.
Surgery on the gastrointestinal system can involve the body’s capability to absorb the required nutrients and minerals.
Unhealthy lifestyle options, like drinking too much alcohol or caffeine, smoking, and not exercising.
What are the symptoms of osteopenia?
Osteopenia generally doesn’t cause any signs or symptoms until it moves to osteoporosis. Infrequently, some people with osteopenia may feel bone pain or weakness. The disease is generally seen when a person has a BMD screening.
Risk factor
So, how precisely do you wind up with low bone density or osteopenia? – By age 30, you’ll have got your peak bone mass the most powerful your bones will be in your lifetime. If you had a childhood condition that involved bone formation or caused malnutrition (for instance, undiagnosed celiac condition or anorexia), your peak bone mass likely isn’t as high as it could be.
Most people don’t have low bone density until mid-life when they begin naturally losing bone mass. But few elements can erode bones earlier, or accelerate loss after age 50. These contain:
Being Born a Female: Anatomy places females at a higher risk for creating low bone density. Female bones are naturally shorter and narrower than men’s, so females have a lower peak bone mass. So, once they begin losing bone with age, there’s small to lose. Analysis has displayed that females age 50 and more seniors are twice as probable to have osteopenia than males.
Smaller Stature: Being a petite, slim, small-boned female is associated with lower bone density levels and a more increased risk of osteoporosis.
Being Caucasian or Asian: These groups manage to have far more increased rates of low bone density than Latinos or African Americans. More than half of white postmenopausal females have the disease.
Genetics: Your bone grade is passed down from your parents. It’s said that up to 80 percent of your peak bone mass is defined by your genetics.
Underlying Conditions: Several conditions can interrupt healthy bone growth by affecting how your body soaks calcium and further nutrients. Examples contain:
- Undiagnosed celiac condition (if not treated through dietary modifications)
- Hyperthyroidism
- Diabetes
- Rheumatoid arthritis
- Eating diseases like anorexia nervosa or bulimia
Rare Bone Diseases: A bone condition, such as those below, can involve your bone density.
- Osteomalacia (softening of bones due to an extreme vitamin D deficiency)
- Pagets condition (which interrupts normal bone remodeling, leaving bones weak)
- Osteogenesis imperfecta is a genetic condition that involves the normal bone formation
Medications: Specific medicines can accelerate bone loss. The biggies are:
- Steroids (long-term use)
- Chemotherapy and different cancer medicines
- Heartburn drugs called Proton pump inhibitors (Prevacid, Nexium)
- Thyroid hormone (extreme quantities)
Diet: A diet chronically low in calcium and vitamin which assists your body soak calcium can involve bone density. Skimping on either nutrient during the first couple of decades of your life may generate your peak bone mass to be low. And failing to obtain sufficient calcium and D as you age will generate your bone to break down quickly. Practicing a balanced, healthy method of eating is best for your bones. Three possibilities that can leave you deficient in many nutrients and vitamins essential for fine bone health:
Having an eating condition
- Excessive dieting
- Weight loss surgery
How do you understand your body is low in calcium? Tell your doctor if you feel any of these symptoms:
- Tingling (especially in your tongue, lips, fingers, and feet)
- Muscle spasms and aches
- Abnormal heart rhythms
Ebbing Hormones: Yup, hormones involve bones, also. The loss of estrogen that arrives with menopause can accelerate bone loss, and going via this change of life early (say, in your 40s) can up your risk of osteopenia. In males, low testosterone levels are also connected to lower bone density.
Excess Alcohol: Chronic, serious drinking (more than two drinks a night) is connected to lower bone density.
Not Enough Exercise (or Too Much): Weight-bearing activities such as dancing, walking, and hiking, as well as resistance exercise place just sufficient stress on bones to facilitate bone formation. This is to build your peak bone mass and support healthy bone mass as you age. Conversely, too much activity doesn’t do a body good. Female competitive athletes are particularly at risk for the female triad: low-calorie intake, interruption of their menstrual cycle, and low bone mineral density.
Socioeconomic Status: For causes, scientists are still analyzing, even when you take exercise, diet, and further lifestyle factors into consideration, females who are of higher socioeconomic class are still 70% less probable to create osteopenia than their lower- and middle-income counterparts, according to a 2020 analysis in the journal Menopause.
Differential Diagnosis
- Homocystinuria
- Hyperparathyroidism
- Imaging in osteomalacia
- Mastocytosis
- Multiple myeloma
- Paget disease
- Scurvy
- Sickle cell anemia
How is bone loss diagnosed?
To analyze low bone mineral density, a healthcare provider will:
Ask questions regarding your family’s medical record, especially osteoporosis.
Ask questions regarding your medical record, involving drugs you’ve taken, medical states you’ve had, lifestyle options you’ve made, etc.
Perform a physical examination.
Order a bone density examination.
Bone density is calculated with dual-energy X-ray absorptiometry (DEXA). DEXA is a fast and painless imaging examination that uses X-rays to specify whether you have healthy bones, osteopenia, or osteoporosis. It provides a score known as a T-score:
- +1 to 1 suggests normal bone density.
- 1 to 2.5 suggests osteopenia.
- 2.5 or lower suggests osteoporosis.
DEXA provides healthcare providers with a baseline measurement. That suggests they can compare the current examination outcomes to future outcomes to specify whether bone density reduces over time.
How are osteopenic bones treated?
Most patients with osteopenia don’t need meds. Little modifications to your lifestyle and diet can do a long method in beefing up your bones, as your physician or doctor will likely tell you. Begin here:
Weight-bearing exercises: Activities that need you to support your body weight (walking, dancing, jogging, etc.) and/or resistance exercise assists to facilitate the new bone formation, which is why they’re suggested for osteopenia and osteoporosis. If your bone density is extremely low, you may like to avoid high-impact activities like running or further falling risks. Non-weight-bearing exercises like swimming and biking are A-okay, as long as you’re even squeezing in weight-bearing activity.
Dietary changes: Increasing your calcium and vitamin D levels can assist in gradual bone deterioration.
The suggestion for calcium is 1200 mg for females over 50 and 1,000 mg for males. Ideally, you should bring your daily dose to your diet. Calcium-rich foods contain:
- Dairy products like yogurt, milk, and cheese
- Dark leafy greens like kale greens and collard greens
- Sardines and salmon with bones
- Fortified foods like orange juice and cereals
Vitamin D arrives from sunlight, as well as foods such as:
- fatty fish like tuna, salmon, and mackerel
- fortified milk
- If you don’t believe you’re getting sufficiently D via diet, a supplement can supply the gap.
Different vitamins and nutrients that have proved useful for bone health are:
- Vitamin C (red peppers, citrus fruits, strawberries)
- Vitamin K (kale, spinach)
- Potassium (raisins, potatoes, bananas)
- Magnesium (tomato products, sweet potatoes, artichoke hearts)
A Mediterranean-style diet of lean proteins, olive oil, and foods rich in omega fatty acids is connected to healthier bone density, also. Some analyses have connected caffeine in coffee and colas to low bone density, but the proof hasn’t been definitive. Specialists say to drink in moderation to play it secure.
Medications
If your FRAX score places you at increased risk for fracture, or you’ve already had a fracture, your doctor or healthcare provider may specify a drug to delay the bone loss. The purpose is to control your osteopenia from progressing to osteoporosis.
What type of med? Bisphosphonates are FDA-approved for controlling osteoporosis in females with osteopenia (as well as managing osteoporosis). These medications delay down those osteoclasts, the cells that break down bone. Most are oral pills brought weekly or monthly. Instances are:
Fosamax (alendronate), carried orally
Boniva (ibandronate), carried orally
Actonel (risedronate), carried orally
Reclast, Zometa, and Aclasta (zoledronic acid or zoledronate), carried through IV
Carrying medicines, if your doctor specifies them, can stave off different bone damage and the breaks that it tends to carry. Giving zoledronate every 18 months for six years decreased the risk of hip fracture in females with osteopenia by 37 percent, likened to those carrying a placebo medicine, one analysis posted In The New England Journal of Medicine displayed. An appointment with your doctor is the first step to beginning therapy to delay your bone loss Don’t wait to make one.
Physiotherapy treatment
Walking, jumping, or running for at least 30 minutes on most days will boost your bones if you have osteopenia, are a young grown-up, or are a premenopausal woman.
These are all instances of weight-bearing activities, which suggests you do them with your feet touching the bottom. While swimming and biking may assist your heart and make muscles, they don’t make bones.
Even small gains in BMD can greatly decrease your risk for fractures after in life.
Yet, as you get more senior, it evolves more difficult for you to create bone. With age, your activity should emphasize muscle strengthening and balance as well.
Walking is still awesome, but now swimming and biking count, also. These activities can assist to decrease your possibility of falling.
Speak with your doctor regarding the best and safest activities for you.
In extra to walking or different exercises, attempt these strengthening activities:
Hip abductors
Hip abductors boost your hips and enhance balance. Accomplish this 2 to 3 times a week.
Stand elevated with your right side facing a chair, grabbing onto the back of the chair with your right hand.
Place your left hand on top of your pelvis and lift your left leg to the side, maintaining it straight.
Maintain toe pointed ahead. Don’t lift so high that your pelvis increases.
More down leg. Recount 10 times.
Switch sides and do the same activity 10 times with your right leg.

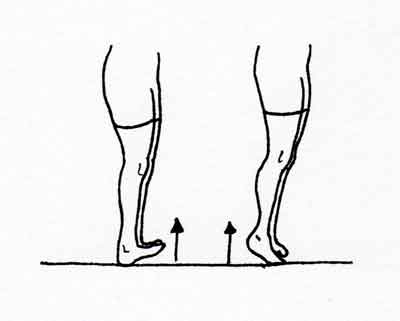
Toe and heel raises
Toe raises and heel lifts boost lower legs and enhance balance. Do them per day. Wear shoes for this activity if you have pain in your feet.
Stand elevated facing the back of a chair. Lightly grab onto it with one or both hands to remain balanced. Work up to being capable to remain balanced using only one hand or a few fingers.
Maintain heels on the bottom and raise toes off the floor. Maintain standing straight with knees straight.
Maintain for 5 seconds. Then more down toes.
Now ascend on toes and maintain for 5 seconds.
Gradually lower heels back to the bottom and recount 10 times.
Prone leg lifts
Prone leg lifts boost your lower back and buttocks and lengthen the front of your thighs. Do this activity 2 to 3 times a week.
Lie on your stomach in a prone position on a mat on the bottom or a firm bed, with a cushion under the abdomen.
Relax your head on your arms, or place a rolled-up towel under your forehead. You can even place a rolled towel under per shoulder and under your feet if you want.
Bring a deep breath, gently push your pelvis against the cushion, and press your buttocks.
Gradually lift one thigh off the bottom, with the knee barely flexed. Maintain for a count of 2, maintaining foot rested.
More down thigh and hip back to the bottom.
Repetition 10 times, then accomplish 10 with the further leg.

Resistance Exercise
One of the most familiar varieties of physical therapy used to manage osteopenia is resistance activity. Resistance exercise allows for an increase in the power and size of skeletal muscles. This can assist to enhance the function of the skeletal system and raise bone density. Resistance activity can be done using a combination of techniques, involving:
Weightlifting: One of the most familiar varieties of resistance activity, weightlifting includes lifting weights utilizing your muscles. Weightlifting can be accomplished with free weights, weight devices, or barbells.
Cardiovascular Exercise: Cardiovascular workout assists to enhance your heart health and raises your overall fitness level. Cardiovascular activity can be done using a mixture of techniques, involving jogging, running, swimming, biking, and rowing.
Resistance Band Exercises: Resistance band activities are another variety of resistance activity that is frequently used in conjunction with different forms of physical therapy. Resistance band activities include using a band to resist the motion of your joints. This variety of activities is frequently used to enhance joint function and decrease pain.
Skeletal Muscle Electrical Stimulation (SMEs): Skeletal muscle electrical stimulation is a variety of resistance exercises that uses electrical currents to facilitate the growth and power of skeletal muscles.
Manual Therapy
Manual therapy is a variety of physical therapy that uses manual techniques to enhance function in the body. Even, Manual therapy is used to manage a mixture of conditions, involving osteopenia. Manual therapy can assist to enhance the range of movement, strength, and flexibility of the joints. It can also assist in decreasing pain and inflammation.
Manual therapy can be performed on a variety of sites, involving the back, neck, hips, shoulders, knees, and feet. The therapist will frequently use a mixture of methods, like stretches, pressure points, and finger activities. In general, manual therapy is most useful when it is mixed with other therapies like osteoporosis drugs or surgery.
Exercise Therapy
Exercise is one of the most familiar states of physical therapy, and for good cause: it functions. Analyses have demonstrated that regular activity can assist to gain bone density and reduce the risk of fractures. The most essential item to recall when beginning an exercise schedule is to slowly add more power and time over time.
Occupational Therapy
Occupational therapy is another variety of physical therapy that is frequently used to assist a person with osteopenia. This variety of therapy concentrates on assisting people with osteopenia to find new methods to use their muscles and bones to enhance their overall physical fitness.
Occupational therapy can assist a person with osteopenia to understand how to do tasks like bathing and dressing, as well as conduct simple activities like balancing on one leg or walking.
Hydrotherapy
One of the most familiar varieties of physical therapy for osteopenia is hydrotherapy. This variety of therapy uses water to assist to enhance the bone health of a person with osteopenia by raising the density and strength of their bones. Hydrotherapy can be done in a mixture of methods, involving shower therapy, bath therapy, and spa therapy.
This variety of therapy is also a good method to reduce stress and tension in the body, which can assist to enhance the bone health of a person with osteopenia.
Chiropractic Care
Another variety of physical therapy that can be used to assist a person with osteopenia is chiropractic care. Chiropractic care concentrates on the help of spinal adjustments and further chiropractic treatments to enhance the overall health of the patient’s bones.
Chiropractic care is useful in assisting to enhance the bone health of a person with osteopenia, and it is a safe variety of therapy that does not need any drugs or surgery.
This may be useful for you.
Acupuncture
There are many varieties of acupuncture, per its precise uses. Here are only a few:
Acupuncture and Tui Na: Acupuncture uses sterile syringes to stimulate detailed points on the body. Tui Na, or Chinese massage, is a variety of acupuncture that utilizes pressure and strokes along the meridians to facilitate relaxation and healing.
Acupuncture and Traditional Chinese Medicine: Acupuncture is frequently used in mix with Chinese drug treatments, which use herbs and different therapies to restore balance in the body. Also, Acupuncture can assist to enhance circulation, reducing pain, and boost the immune system.
Acupuncture for Chronic Pain: Acupuncture is useful in managing chronic pain disorders like fibromyalgia and tension headaches. By managing the root cause of the pain, acupuncture can deliver ease for a longer duration than traditional drugs.
Yoga
Many varieties of yoga can be useful for people with osteopenia. In special, Iyengar and Hatha yoga are two famous varieties of yoga that can assist to enhance balance, flexibility, and postural awareness. Yoga also assists to raise energy levels and facilitates restful sleep.
In addition, yoga can enhance muscle strength and function, conducting to improved mobility and quality of life.
Yoga can be conducted separately or in a group setting. It is essential to talk with your physical therapist regarding what kind of yoga may be best suited for you based on your situation and requirements.
Preventing osteopenia
The best method to control osteopenia is to avoid the manners that cause it. If you already smoke or drink a lot of alcohol or caffeine, stop particularly if you’re more youthful than age 35, when you can still make bone.
If you’re more senior than age 65, your doctor will probably recommend a DEXA scan at least once to examine for bone loss.
Person of all ages can assist their bones to remain strong by keeping a healthy diet, making certain they get sufficient calcium and vitamin D. In extra to food, another method to obtain vitamin D is with a small quantity of sun exposure. Speak with your doctor regarding safe sun exposure based on your further health diseases.
FAQ
Is osteopenia a serious condition?
Though osteoporosis is thought the more extreme form of osteopenia, osteopenia can be only as risky as osteoporosis when mixed with other risk factors, like smoking, lack of vitamin D, a low-calcium diet, hormonal changes due to age
Can osteopenia be cured?
Osteopenia can be managed either with activity and nutrition or with drugs. But some doctors are increasingly wary of overmedicating people who have osteopenia. The fracture risk is low to start with, and analysis has shown that the drug may not decrease it that much.
Can you rebuild bone if you have osteopenia?
You can change the loss of bone density with medical treatments that may delay, maintain, or even raise your bone density. Your doctor may suggest carrying specific drugs to control or manage bone loss, and some may even assist you to rebuild bone density.
Can you go from osteopenia to normal?
Some drugs can assist to place bone density back into the normal range, but not everyone will or should bring long-term drugs. Yet, there are further actions you can bring to delay the progression from osteopenia to osteoporosis.
Does walking improve osteopenia?
You can control bone loss with regular exercises, like walking. If you have osteoporosis or fragile bones, normal brisk walking can assist to maintain your bones strong and decrease the risk of a fracture in the future. How should you walk and how frequently? You should walk briskly regularly.




4 Comments