Hand Joint Pain
What is a Hand Joint Pain?
Hand joint pain is a common complaint that can significantly impact daily activities and quality of life. The hands are intricate structures composed of numerous joints, tendons, ligaments, and muscles, facilitating a wide range of movements essential for various tasks.
Joint pain in the hands can arise from a myriad of causes, including injury, overuse, inflammatory conditions such as arthritis, and degenerative changes associated with aging. Understanding the underlying cause of hand joint pain is crucial for effective management and treatment.
This introduction sets the stage for exploring the diverse factors contributing to hand joint pain and strategies for alleviating discomfort and improving hand function.
Introduction
What is hand degenerative arthritis?
- The illness known as arthritis damages the tissues in your joints. A joint is where two bones meet. Both the cartilage, or smooth coating at the ends of bones and the lining of your joint may be attacked by arthritis.
- Your bones’ ends eventually become exposed, grind against one another, and wear away as the cartilage degrades. Because the hand has so many joints, arthritis frequently develops there.
- Hand arthritis results in discomfort, edema, stiffness, and deformity. As arthritis worsens, you cannot perform daily duties with your hands.
- Given the variety of elements that make up the hand, there are numerous potential reasons for hand discomfort. In addition to helping the hands perform a variety of functions, the bones, ligaments, tendons, nerves, skin, and other components can also cause discomfort.
- Rheumatoid arthritis affects roughly 0.24% of the population, but osteoarthritis affects over 3.8% of people. About 1-2% of people in the West will experience gout at some point in their life. In the United States, almost 20% of people suffer from some form of arthritis, compared to 15% in Australia.
- In general, the condition is more common as people get older. People frequently miss work due to arthritis, which can also lower their quality of life. The Greek terms arthr-, which means “joint,” and itis, which means “inflammation,” are the source of the name.
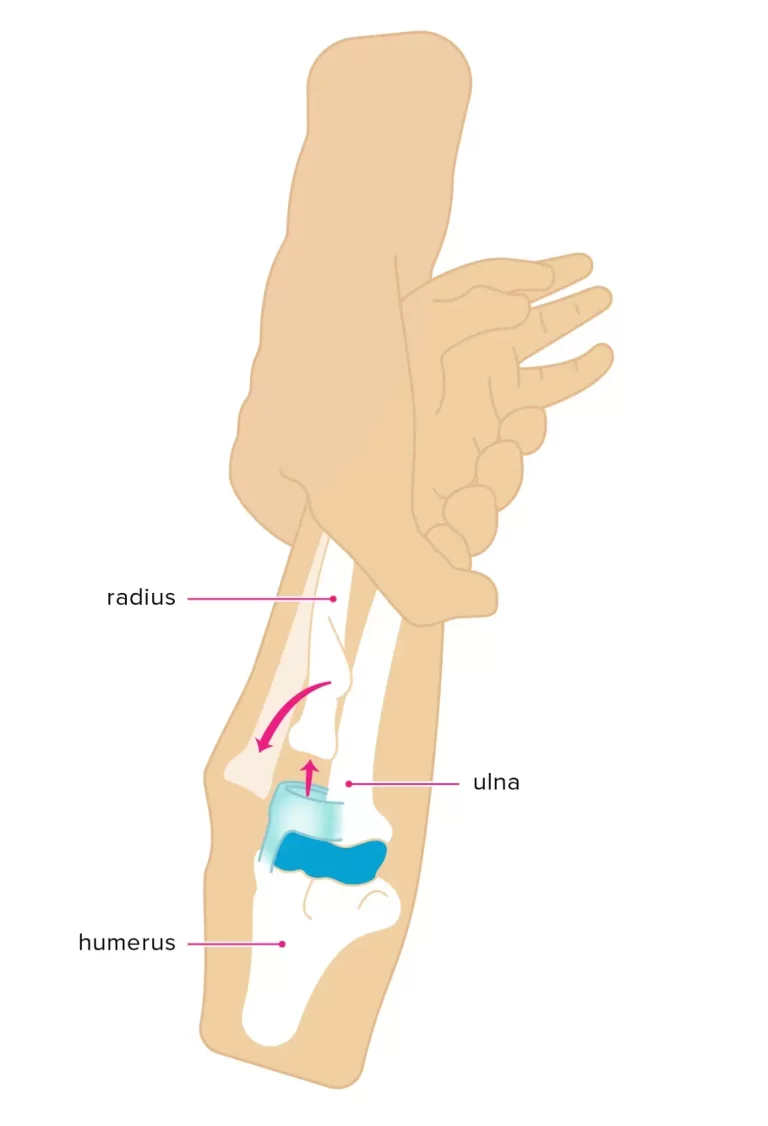
Anatomy of the hand
- The hand’s extensive range of motion and dexterity are made possible by its numerous bones, muscles, and ligaments. The hand itself consists of three main types of bones, which are as follows
- Phalanges: The fourteen bones are located in each foot’s toe as well as each hand’s finger. The thumb only has two phalanges, but each finger has three: the distal, middle, and proximal.
- Bones in the metacarpal region: the five bones that make up the hand’s middle section.
- Bones of the carpal region: the wrist’s eight forming bones. The ulnar and radius bones are the two arm bones to which the carpal bones are attached.
- The hand is made up of many muscles, ligaments, and sheaths. The structures are the muscles.
- It can contract, enabling the hand’s bones to move. The fibrous structures known as ligaments aid in holding the hand’s joints together. The tubular structures known as sheaths encircle a portion of the fingers.
Structure of the hands and wrists
- The 27 little bones that make up each hand and wrist. There are eight bones in your wrist. Every digit contains three bones, while the thumb, has two. The five bones that connect the thumb, each finger, and the wrist form the palm of your hand.
- The hand and wrist are controlled by more than 30 muscles. Your hands, wrists, and forearms contain them.
- Tendons connect muscles to bones. These are tiny, incredibly durable bits of connective tissue. Tendons go through the carpal tunnel, a bony passageway in the wrist. This tunnel is also used by the median nerve.
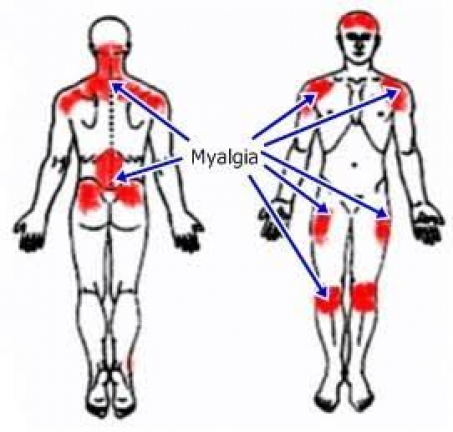
Symptoms related to Hand Joint Pain
- Almost all forms of arthritis are accompanied by pain, which can range in intensity. Additional signs and symptoms include redness, hurting near the joint(s), swelling, and stiffness in the joints.
- Numerous symptoms can arise from arthritis conditions that impact other organs in the body, such as rheumatoid arthritis and lupus.
- Among the symptoms could be:
- unable to walk or use their hands
- rigidity in one or more of the joints
- Itching or rash
- Weakness and exhaustion
- Loss of weight
- Insufficient sleep
- weakened muscles
- Diminished adaptability
- Reduced capacity for aerobic exercise
- Along with the main symptoms, these alterations can significantly affect the quality of life.
- Achy or burning joint pain that develops hours or days after you use your hands more frequently.
- Your hand(s) hurts and feel stiff in the morning.
- Swelling in the joint(s) of your hand.
- If you’ve experienced long-term arthritis in one or more of your hands:
- There are more frequent symptoms.
- A subtle aching could become a searing pain.
- Pain could keep you up at night.
- You might adjust how you use your hand(s) if you are in pain.
- Your afflicted joint’s surrounding tissue may turn red and sensitive to touch.
- When you bend your fingers, you’ll experience a grating, grinding, cracking, or clicking sensation (crepitus).
- You cannot fully open and close your fingers.
- Bouchard’s nodes, or little bone nodules, can develop at the top or middle joints of your fingers.
- Your fingers grow weak and less able to perform daily duties as a result of the enlargement, deformity, and abnormal bending of your finger joints.
Causes of Hand Joint Pain
Injury
- Pain can result from injuries to the palm.
- Knocks and blows, landing on the hands after a fall, wounds, burns, and repetitive trauma from sports or other activities are some of the causes of palm injuries.
- Repetitive strain injury (RSI), another name for overuse, is the result of repeated actions that make the hand sore or stiff. Hand pain and tension can also originate from the muscles in the arms and shoulders.
- RSI can be brought on by prolonged durations of high-intensity or repetitive activity, as well as by gripping the hands awkwardly.
- RSI is more frequent in the fingers or wrists, but it can happen anywhere on the hand, including the palms.
Disability
- Every day, about 20 million people with arthritis experience significant functional difficulties. People with arthritis often suffer absenteeism and make frequent doctor appointments. People with arthritis may find it difficult to engage in physical activity, and some may end up bedridden.
- An estimated $100 billion is spent on arthritis cases overall, with lost wages accounting for over half of that amount. approximately 1 million hospital admissions and approximately 45 million outpatient visits to medical facilities are caused by arthritis each year.
- When combined with the symptoms mentioned above, decreased mobility might make it difficult for a person to maintain an active lifestyle, which raises the risk of obesity, high cholesterol, or heart disease.
- Individuals who have people with arthritis are more likely to experience sadness, which can be brought on by a variety of emotions, such as anxiety about their symptoms getting worse.
Which hand portions are most commonly impacted by hand joint pain?
Your hand’s four regions that arthritis is attacking are:
- The point where your thumb and wrist connect at its base.
- Your knuckles.
- The finger joints are in the middle.
- The finger joint on top that is closest to your nails.
Types of Arthritis
Osteoarthritis
- The most prevalent type of arthritis is osteoarthritis. It affects not only people but also other animals, including cats and horses, but most commonly dogs. Both the body’s bigger and smaller joints may be impacted. This covers the hands, wrists, feet, back, hips, and knees in humans. This covers the stifle (knee), elbow, hip, shoulder, and back in dogs.
- Osteoarthritis is mostly a condition brought on by normal joint wear and tear, though injuries can also cause the condition. The disease known as osteoarthritis starts in the cartilage and progressively erodes the two opposing bones into one another.
- When engaging in physical activity, the ailment first causes little discomfort, but soon it can become constant and can happen when in a state of relaxation. It is possible for the discomfort to be incapacitating, making certain activities impossible.
- Dogs experiencing this pain may have difficulty walking on slick floors, climbing stairs, getting up after lying down, being unable to hop in and out of cars, having trouble jumping on and off furniture, and behavioral changes (such as aggression or difficulty squatting to relieve themselves).
- All of these symptoms can have a significant negative impact on a dog’s quality of life. Usually, osteoarthritis affects weight-bearing joints like the hip, knee, and back. In contrast to rheumatoid arthritis, osteoarthritis primarily affects the older population.
- Growing older is the best indicator of osteoarthritis, probably because chondrocytes are losing their capacity to preserve the structural integrity of cartilage. Over thirty percent of women possess a degree of osteoarthritis by the time one is 65. Obesity, a sedentary lifestyle, and previous joint injuries are other risk factors for osteoarthritis.
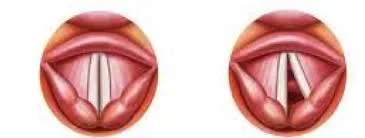
Rheumatoid arthritis
- The condition known as rheumatoid arthritis (RA) occurs when the body’s immune system begins to target bodily tissues.
- Numerous other bodily parts are also targeted by the attack in addition to the joint. The majority of damage in rheumatoid arthritis is to the cartilage and joint lining, which ultimately leads to the erosion of two opposing bones.
- RA frequently affects joints in the fingers, wrists, knees, and elbows, is symmetrical (appears on both sides of the body), and can develop into severe deformity in a few years if not addressed. Most cases of RA occur in adults over the age of 20.
- Children with the disorder may experience skin rashes, fevers, pains, disabilities, and difficulties with day-to-day activities
- With prompt diagnosis and intensive care, many people can have a higher quality of life than if they wait a long time to get a diagnosis after RA first appears.
- The highest correlations between risk variables and the development of rheumatoid arthritis are female sex, age, obesity, prior joint damage from an injury, and tobacco smoke exposure.
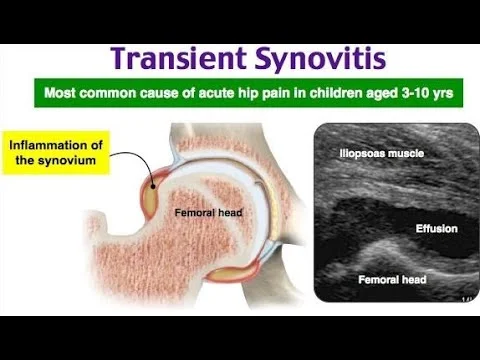
- One main characteristic of rheumatoid arthritis is bone deterioration. Osteoclasts that resorb bone and osteoblasts that produce new bone are constantly modifying bone.
- An important factor contributing to bone erosion in rheumatoid arthritis joints is synovial inflammation, which is triggered by the release of pro-inflammatory cytokines and the cell surface protein receptor activator of nuclear factor kappa B ligand (RANKL), which is found in Th17 cells and osteoblasts.
- The activity of osteoclasts can be directly introduced by osteoblasts via the RANK/RANKL pathway.
Diagnosis
- Depending on the type of probable arthritis, additional tests including blood and radiological examinations may be used to confirm the diagnosis, which is confirmed by a clinical examination performed by a qualified healthcare provider.
- Pain is a possible component of all arthritis. Depending on the location and the arthritis, different pain patterns may occur.
- Rheumatoid arthritis typically causes stiffness that lasts longer than thirty minutes and is worst in the morning. After taking a warm shower, patients may not experience any symptoms in the early stages.
- Conversely, stiffness in the morning that goes away somewhat quickly with movement and exercise is often linked to osteoarthritis.
- Pain may not always be the primary presenting symptom in the elderly or young; in the former case, the patient simply moves less, while in the latter case, the patient refuses to use the affected limb.
- The diagnosis is guided by some aspects of the disorder’s history. The rapidity and timing of the start, the pattern of joints involved, the symmetry of the symptoms, the stiffness and discomfort in the morning, the gelling or locking with inactivity, the aggravating and alleviating factors, and other systemic symptoms are important elements.
- It could involve assessing joints, monitoring motions, looking for rashes or nodules on the skin, and looking for signs of lung inflammation.
- A physical examination could support the diagnosis or point to a systemic illness. Radiographs are frequently used to monitor development or assist in determining severity.
- To make the diagnosis, X-rays of the afflicted joints and blood tests are frequently carried out. If a particular type of arthritis is suspected, screening blood tests should be performed. These could consist of particular antibodies, extractable nuclear antigens, antinuclear factor (ANF), and rheumatoid factor.
- Patients with rheumatoid arthritis frequently exhibit elevated levels of C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR, sometimes referred to as sed rate), which shows that the body is undergoing an inflammatory process.
- Two more frequently performed blood tests are rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) antibodies. While negative results help rule out this autoimmune illness, positive results indicate the possibility of rheumatoid arthritis.
- Imaging studies used to diagnose and track arthritis include MRIs, ultrasounds, and X-rays. Additional imaging procedures for rheumatoid arthritis that could be taken into consideration are bone scanning, dual-energy X-ray absorptiometry (DEXA), computed tomography (CT), and positron emission tomography (PET).
Specific hand and wrist conditions
The tendinopathy of De Quervain
- Tendon issues in the hand and wrist can arise.
- Tendons possess a sheath, or protective covering, filled with synovial fluid. This viscous liquid shields the tendon and facilitates its movement.
- Tendons or their sheaths may occasionally become inflamed. This is known as tendinopathy and can result in discomfort, edema, and stiffness.
- Overuse of tendons, such as from prolonged sports participation, can cause it.
- Tendinopathy can result from arthritis, and in rare instances, an infection as well. There may not always be a clear reason.
- De Quervain’s (Dey were-veins) tendinopathy is a frequent disorder that can cause discomfort around the base of the thumb and the wrist due to damage to the tendons in the wrist. Pain often subsides with rest and may intensify with movement.
- Using moist towel-wrapped ice and taking
- An NSAID can be beneficial. Surgery, hand therapy, splints, steroid injections, or other treatments may be beneficial if your problem is not getting better and is negatively impacting your quality of life.
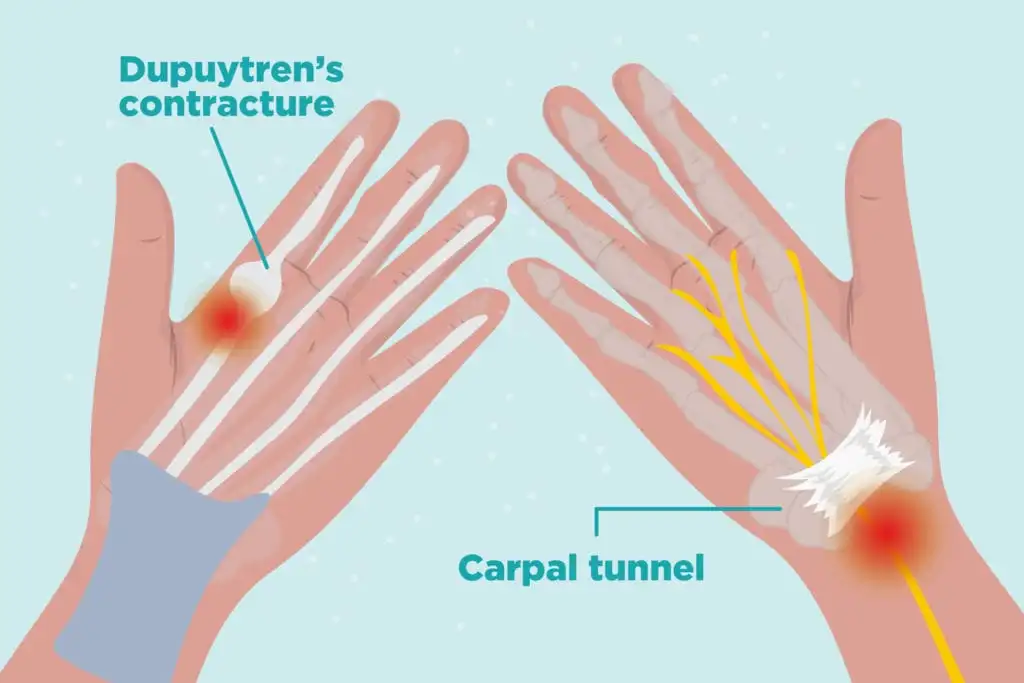
Carpal tunnel syndrome
- The condition known as carpal tunnel syndrome
- When the median nerve experiences pressure while it travels through the carpal tunnel, carpal tunnel syndrome develops.
- This may result in discomfort, tingling, and numbness, mostly in your fingers and hands. Similar symptoms may also be experienced in the forearm and wrist. Often, the symptoms worsen at night.
- Make an appointment at your general practitioner’s office if you believe you may have carpal tunnel syndrome.
- In a few weeks or months, carpal tunnel syndrome may disappear. An injection of steroids or the use of a splint can be beneficial.
Trigger finger
- An inability to properly straighten a finger or thumb is known as a trigger finger. To straighten it, you might even need to use your other hand. On rare occasions, a finger may become too painful to move and may become frozen in place.
- The thumb, ring, and middle fingers are most frequently impacted by the trigger finger. Multiple fingers can be impacted simultaneously.
- It can hurt, and the affected finger might enlarge.
- Particularly in the morning, there may be a popping or clicking sound coming from the finger.
- It is believed to be brought on by tendon or tendon sheath edema.
- Nodules may sometimes develop as a result of the swelling. These little protuberances appear beneath the dermis.
- People who are generally healthy may experience trigger fingers for unknown reasons. It affects women over 40 more frequently.
- If you’ve already sustained an injury to your hand’s palm, your chances are higher. An underactive thyroid, gout, diabetes, rheumatoid arthritis, and other medical disorders may also raise a person’s chance of developing it.
- Treatment is not necessary for the trigger finger; it can heal on its own. If it’s believed that any particular activity is aggravating your symptoms, you might need to stop doing it.
Dupuytren’s contracture
- The fingers of a person with Dupuytren’s (due-per-tren’s) contracture may bend inward into the palm.
- The reason behind this is that as the tissues in the palms of the hands increasingly thicken, the fingers are drawn inward toward the palm.
- Since this ailment is usually mild, no special treatment may be required. Middle-aged men are more likely to experience it. It is believed that certain strenuous, repetitive jobs, like mining, raise the risk of Dupuytren’s.
- Usually, the little, ring, and middle fingers are affected.
- Although it’s not always uncomfortable, it might make it challenging to correctly use your hands and straighten out your fingers.
- Or if you have improper hand function.
- During the initial phases, injectable collagenase (colla-gen-ayse) injections were one of the possible treatment choices. The thicker tissues may be broken down by this. This is a simple, short therapy that doesn’t require an operation.
- It may be quite uncomfortable for you to have your fingers stretched and straightened by a medical practitioner afterward.
- Surgery can be used to remove the thicker tissue or to chop it away. This can be performed at an outpatient clinic as an operation or with a needle.
Raynaud’s phenomenon
- The illness known as Raynaud’s phenomenon lowers blood flow to the body’s extremities, especially the fingers.
- It might occur in chilly weather or under pressure. It can also happen when you use vibrating hand tools.
- A Raynaud’s attack can cause color changes in the fingers. They may first appear waxy or turn white. After that, they may turn blue, and in extreme circumstances, even purple or black. When the blood rushes back, they may become uncomfortable, tingling, and numb in addition to likely turning red.
- In colder climates, staying warm can help lower the risk of a Raynaud’s attack. It will be beneficial to wear gloves, a scarf, a cap, and multiple layers of clothes.
- Heated gloves and hand warmers, whether reusable or disposable, can be useful.
- Applying moisturizer to your fingertips at least once or twice a day can help to maintain the healthiest possible skin on them. Which ones are suitable for those with Raynaud’s disease can be determined by speaking with your pharmacist.
- Regular exercise also improves blood circulation.
Treatment of Hand Joint Pain
How is hand arthritis treated?
- Options for treatment vary depending on the kind and stage of arthritis, number of affected joints, age, degree of activity, affected hand (if dominant), and coexisting medical disorders.
- Reduction of stiffness and pain in the joints is the main aim of treatment.
- Enhance function and movement.
- Increase your standard of living.
- To slow the disease’s course in cases with psoriatic or rheumatoid arthritis.
- Options for treatment include bracing or splinting, medication, injections, non-pharmacological methods, and surgery.
- Braces or splinting
- In addition to reducing deformity, providing joint stability, reducing strain, and promoting normal joint alignment, splits or braces support and preserve the injured joint.
- The hand therapist, occupational therapist, or healthcare practitioner will go over the various splinting and bracing alternatives with you.
Medical Treatment
- If you have rheumatoid or psoriatic arthritis, your doctor may prescribe medicine to lessen joint pain and swelling as well as to prevent joint deterioration. The kind and severity of your arthritis may determine which drug classes your doctor tries.
- The only medications that are advised for osteoarthritis symptom treatment are acetaminophen or nonsteroidal anti-inflammatory medicines, to be used sparingly (as needed). As of right now, no drugs have been licensed to assist in slowing the advancement of osteoarthritis.
- The medications on this list are used to treat psoriatic and rheumatoid arthritis. As there are hazards and reasons not to use over-the-counter medications (depending on your other health issues and/or prescriptions), make sure you consult with your provider before taking any.
- Acetaminophen: This medication aids with pain relief.
- Anti-inflammatory non-steroidal medications: These medications lessen joint discomfort and edema. Ibuprofen, diclofenac, naproxen, and celecoxib are a few examples. For osteoarthritis, topical NSAIDs are the primary line of treatment.
- Antirheumatic medications that change disease: These reduce symptoms and delay the course of rheumatoid arthritis. Methotrexate, hydroxychloroquine, leflunomide (Arava®), and sulfasalazine (Azulfidine®) are a few examples.
- Steroids: These drugs, which can be taken orally, injected into a muscle, or administered intravenously, lessen inflammation and other rheumatoid arthritis symptoms. Prednisolone, prednisone, triamcinolone, and methylprednisolone are a few examples.
- Anti-immunization Medications: These lessen damage to the bone that surrounds joints and decrease the course of rheumatoid arthritis. Azathioprine and cyclosporine are two examples.
- Biological agent: These can lessen rheumatoid arthritis-related joint degradation. Adalimumab (Humira®), etanercept (Enbrel®), infliximab (Remicade®), and tofacitinib are a few examples
- of injections of steroids
- Steroids ease pain and lessen inflammation. When anti-inflammatory drugs fail to control the inflammation or if it is confined to a small number of joints, steroids are typically employed. Injections are administered directly to the wounded joint
- Injections are only given a few times because steroids have the potential to damage tendons and ligaments.
Surgery
- Surgery can be necessary if nonsurgical therapies are no longer effective and your bone ends’ cartilage has deteriorated.
- There are various methods:
Arthritis (fusion of the joints): To maintain the integrity of your joint’s bones, this operation uses screws and a plate. Although your joint will be more stable and pain-free, your range of motion and flexibility will be restricted. - Arthroplasty, or replacement of a joint: Surgeons replace your injured joint with an artificial implant composed of plastic, ceramic, silicone, or metal, much like they do with other joint replacements. Remember that typical finger movement is not replicated by hinged finger implants.
- Transfer of tendon: Tendons are what join muscles and bones. The muscles in your palm and forearm are where the tendons that govern your fingers attach. Chronic inflammation brought on by arthritis may rupture tendons. In such a case, hand function can be restored using a segment of a healthy tendon.
- You can lessen pain and swelling by applying an ice pack to your hands and wrists. Use a packet of frozen peas that has been moist towel-wrapped. Avoid putting ice directly on your skin as this may cause irritation or burning. Applying ice many times a day for up to 20 minutes at a time is possible.
- Using heat may help ease the discomfort and stiffness in your hands. Some items, such as wheat bags, can be heated in a microwave and are available from chemists. You may need to cover your skin with a cloth or tea towel to prevent burning.
- Taking a warm bath or shower, or placing your hand and wrist on a hot water bottle with the cover on, can also offer a little comfort. Moving your hand in a warm bowl of water can be helpful and soothing.
- Avoid applying heat to your hand or wrist if it’s swollen or you have suffered an injury because it could make the situation worse.
A wax bath is an additional form of heat therapy that relieves pain and stiffness. It’s a good idea to utilize one before engaging in hand exercises to maximize the benefits. - Find out where to buy one and ask your physician, pharmacist, or hand therapist for advice on how to use it. Make sure you adhere to the instructions exactly and don’t heat the wax too much.
- Use caution when using them if you have cuts or open sores.
alternating throughout the day between ice and heat therapy might be useful. Ice reduces pain and swelling by reducing blood flow. - Heat promotes blood flow, which may be beneficial if your hands are tense and your muscles are worn out. Moreover, heat aids in the healing of soft tissue injuries.
Which kind of hand surgery is most frequently used for the particular joints that arthritis affects?
- Thumb base: The point where your thumb and wrist meet. Common surgical procedures include tendon transfer, joint fusion, or partial or complete removal of one of the trapezium bones (the wrist bone just below your thumb joint).
- Knuckles (metacarpophalangeal joints): For this type of repair, joint replacement is nearly always an option. Your knuckles may sustain major damage and become disabled as a result of rheumatoid arthritis.
- Your finger’s proximal interphalangeal joints, or second joint: Loss of mobility and stiffness are frequent symptoms of osteoarthritis. For these joints, joint fusion or replacement are options.
- There’s a danger that your implant may wear out because you utilize these joints so often. In this situation, your physician might advise more surgery.
- Distal interphalangeal joints, or the top of the finger joint: Joint fusion is frequently done to treat arthritis in the joint.
- The hand and wrist can be supported by wearing splints. While some are meant to be used throughout daily activities, others are meant to be used during sleep or relaxation.
- A hand therapist, physiotherapist, or occupational therapist can provide you with advice on whether a splint would be helpful, which sort would be best for you, and how to use it properly.
- Among the hand surgery complications are:
- Lack of progress in terms of mobility.
- Need to swap out a worn-out or broken implant
- inability of the bones to correctly align or grow together (for fusion surgery).
Recovery after Surgery
- Numerous variables affect recovery time, such as the extent of your illness, the kind of surgery you underwent, the expertise of your surgeon, and how well you adhere to treatment.
- After joint repair surgery, the majority of patients can resume their normal activities in three months. The most accurate estimate of how long your specific recovery will take comes from your team of caregivers.
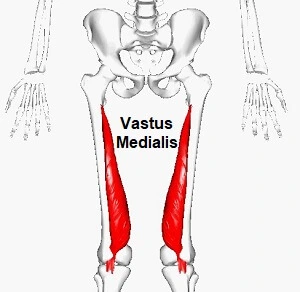
Physiotherapy Treatment
- These extra methods are part of a comprehensive treatment plan for hand arthritis:
- Exercises to increase function and lessen symptoms include stretching and strengthening. The exercises that are most appropriate for your hand arthritis will be recommended by a hand therapist in collaboration with you.
- packs that are both hot and cold. The cold can aid with edema and pain relief. Stiffness can be lessened by heat. Apply for a maximum of twenty minutes at a time.
- Relax. Frequent breaks can be beneficial.
- reduce joint discomfort and inflammation.
- eating well and controlling cholesterol and diabetes.
- If you’re overweight, lose weight.
- giving up smoking. Smokers are more prone to get arthritis.
- occupational therapy to learn how to operate self-help gadgets, such as those that help with getting dressed or cooking
Prevention
Is it possible to avoid having hand arthritis?
- There is no way to avoid arthritis. But as you get older, keep an eye out for arthritis symptoms and consult your doctor if you have any changes in your joints.
- Additionally, you have the option to control some risk factors. Consume wholesome foods to keep your weight stable and nourish your body.
- Your joints are under increased stress when you are overweight, defined as having a body mass index (BMI) of more than 25. Avoid smoking. Arthritis is more likely to develop among smokers.
Summary
- Arthritis symptoms include hand edema and stiffness in the morning. Hand arthritics can be of many different kinds.
- Various therapy options are available based on the specific form of arthritis you have. Drugs can lessen swelling and pain in the joints.
- Methods to reduce the rate at which osteoarthritis progresses are still being investigated. If you suspect that you may have hand arthritis, consult your physician.
- They will conduct a thorough examination and provide you with a comprehensive treatment plan that includes standard therapies including medication, braces or splints, steroid injections, surgery, and hand exercises in addition to other lifestyle advice and the use of hot and cold packs.
FAQ
What is the source of hand joint pain?
Arthritis symptoms include swollen joints in your hands, morning stiffness, and dull or burning joint pain. Hand arthritics can be of many different kinds. Various therapy options are available based on the specific form of arthritis you have. Drugs can lessen swelling and pain in the joints.
How is pain in the hand joints treated?
These include non-steroidal anti-inflammatory medicines (NSAIDs), such as ibuprofen, and painkillers like paracetamol. You can apply NSAID gels on your hands and wrists. Alternatively, you can ingest pills. Combining gels and tablets should be done with caution to avoid taking too much since they both enter your bloodstream
Which inadequacy results in pain in the hands and joints?
Indeed, several research indicates that joint discomfort and swelling may result from vitamin deficiencies. A vitamin D shortage will have a detrimental effect on the bones because it is necessary for bone growth and health. We have known since elementary school how crucial vitamin D is to the health of our bones.
What illness symptoms include hand pain?
Hand arthritis can cause excruciating discomfort. Rheumatoid arthritis is a disorder that can damage joints anywhere in the body, but it typically affects the tendons and joints around the wrist and fingers. It may result in painful, swollen, and even malformed joints. This may impair hand function normally.
References
- Hand and wrist pain. (n.d.). Versus Arthritis. https://versusarthritis.org/about-arthritis/conditions/hand-and-wrist-pain/
- Professional, C. C. M. (n.d.). Arthritis of the Hand. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/7082-arthritis-of-the-wrist-and-hand
- Cluett, J. (2023, August 29). Hand Pain Causes and Treatment Options. Verywell Health. https://www.verywellhealth.com/hand-pain-causes-treatment-and-when-to-see-a-doctor-4178830
- Arthritis. (2023, December 6). Wikipedia. https://en.wikipedia.org/wiki/Arthritis
- Hand Pain and Problems. (2021, October 22). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/hand-pain-and-problems#:~:text=Arthritis%20of%20the%20hand%20can%20be%20very%20painful.


One Comment