Pancuronium Bromide
Introduction
Pancuronium bromide is a synthetic, non-depolarizing neuromuscular blocking agent used in medical settings to induce muscle relaxation and paralysis during certain procedures. It belongs to the class of drugs known as neuromuscular blockers or muscle relaxants.
The drug is administered intravenously and acts by blocking the transmission of nerve impulses at the neuromuscular junction, which is the point where nerves communicate with muscles. By interfering with this communication, pancuronium bromide causes temporary paralysis of skeletal muscles, including the respiratory muscles. This paralysis can be beneficial during surgeries, endotracheal intubation, or other medical procedures where muscle relaxation is necessary.
Generic Name – Pancuronium
Metabolism: Hepatic
Routes of administration: Intravenous
Excretion: Renal and biliary
Protein binding: 77 to 91%
Pregnancy category: AU: B2
AHFS/Drugs.com: Monograph
ATC code: M03AC01 (WHO)
Type – Small Molecule
Groups – Approved
Chemical Formula – C35H60N2O4
Synonyms
- Pancuronium
Associated Therapies
- General Anesthesia
- Facilitation of small bowel intubation therapy
- Smooth muscle relaxation before radiological procedures therapy
Pancuronium bromide has been used primarily in anesthesia and critical care settings. Its effects are reversible with acetylcholinesterase inhibitors, such as neostigmine or edrophonium, which restore neuromuscular function after the procedure is completed. It is important to note that pancuronium bromide should only be administered by trained medical professionals, as improper use or dosage can lead to serious complications, particularly regarding respiratory function. Therefore, its use is strictly regulated and closely monitored to ensure patient safety.
What is pancuronium bromide?
Pancuronium bromide is a synthetic, non-depolarizing neuromuscular blocking agent, also known as a muscle relaxant. It is used in medical settings to induce temporary muscle paralysis, particularly in surgical and critical care situations. Neuromuscular blocking agents like pancuronium bromide act at the neuromuscular junction, which is the connection point between nerves and muscles. These drugs interfere with the transmission of nerve impulses, specifically blocking the action of acetylcholine, a neurotransmitter responsible for muscle contraction. By doing so, pancuronium bromide causes muscle relaxation and temporary paralysis.
The primary medical uses of pancuronium bromide include facilitating endotracheal intubation (placement of a breathing tube into the windpipe), providing muscle relaxation during surgeries, and aiding mechanical ventilation in intensive care units. It is essential to administer pancuronium bromide carefully and under the supervision of trained medical professionals, as incorrect dosage or administration can lead to complications, particularly respiratory-related issues. The effects of pancuronium bromide are reversible with the use of specific antidotes called acetylcholinesterase inhibitors, which restore normal neuromuscular function after its use.
While pancuronium bromide has been used effectively in medical practice, the decision to use this drug is made based on the patient’s individual needs, medical condition, and the expertise of the medical team involved in their care. As with any medication, potential risks and benefits should be carefully considered before administration.
Who can take pancuronium bromide ?
Pancuronium bromide is a prescription medication used in medical settings and is not intended for self-administration. It is administered by healthcare professionals, typically anesthesiologists or critical care specialists, to induce muscle relaxation and temporary paralysis during certain medical procedures. The drug is used in specific situations where muscle relaxation is essential for facilitating procedures, such as endotracheal intubation for mechanical ventilation during surgery or critical care, or when precise muscle control is required for surgical procedures.
Pancuronium bromide should not be taken by individuals without a valid medical reason and appropriate medical supervision. It is not prescribed for general use or to treat any medical condition. There are certain contraindications and precautions to consider when administering pancuronium bromide. It should be used with caution or avoided altogether in individuals with certain medical conditions, including:
- Hypersensitivity: People who have known hypersensitivity or allergic reactions to pancuronium bromide or any other neuromuscular blocking agents should not receive this medication.
- Myasthenia Gravis: Pancuronium bromide can exacerbate muscle weakness in individuals with myasthenia gravis, a neuromuscular disorder characterized by muscle weakness and fatigue.
- Respiratory Conditions: The drug can cause respiratory muscle paralysis, so it should be used with caution or avoided in patients with severe respiratory disorders, like severe asthma or chronic obstructive pulmonary disease (COPD).
- Kidney or Liver Impairment: Pancuronium bromide is primarily eliminated from the body through the kidneys and liver, so it should be used with caution in patients with impaired kidney or liver function.
- Cardiovascular Conditions: It should be used carefully in patients with cardiovascular diseases, as it may cause changes in heart rate and blood pressure.
- Electrolyte Imbalances: Pancuronium bromide may alter potassium levels in the blood, so it should be used cautiously in individuals with known electrolyte imbalances.
As with any medication, the decision to administer pancuronium bromide is based on a thorough assessment of the patient’s medical history, current health status, and the specific medical procedure or situation requiring muscle relaxation. The dosage and administration are carefully determined by the healthcare team to ensure patient safety and optimal outcomes.
Who cannot take pancuronium bromide?
Certain individuals should not receive pancuronium bromide due to the potential risks and complications associated with its use. These contraindications and precautions include:
- Hypersensitivity: If a person has a known allergy or hypersensitivity to pancuronium bromide or any other neuromuscular blocking agent, they should not receive this medication.
- Myasthenia Gravis: Pancuronium bromide can worsen muscle weakness in individuals with myasthenia gravis, a neuromuscular disorder that causes muscle weakness and fatigue. Using this medication in such patients can lead to severe respiratory compromise and other complications.
- Severe Respiratory Conditions: Individuals with severe respiratory disorders, such as acute or severe bronchial asthma, chronic obstructive pulmonary disease (COPD), or other conditions affecting lung function, should not take pancuronium bromide. The drug can cause respiratory muscle paralysis, which could be life-threatening in individuals with compromised respiratory function.
- Severe Cardiovascular Conditions: Pancuronium bromide may cause changes in heart rate and blood pressure. It should be used with caution or avoided in patients with severe cardiovascular diseases, such as severe heart failure or significant cardiac arrhythmias.
- Kidney or Liver Impairment: The elimination of pancuronium bromide primarily occurs through the kidneys and liver. Individuals with severe kidney or liver impairment may experience delayed clearance of the drug, leading to prolonged effects and potential adverse reactions.
- Electrolyte Imbalances: Pancuronium bromide can affect potassium levels in the blood. Patients with pre-existing electrolyte imbalances, such as hyperkalemia (high potassium levels) or hypokalemia (low potassium levels), should be carefully evaluated before receiving this medication.
- Pregnancy and Breastfeeding: Pancuronium bromide’s safety during pregnancy has not been well-established, and it is generally avoided during pregnancy unless the benefits outweigh the potential risks. The drug may also pass into breast milk, so it is not recommended for breastfeeding women.
It is crucial for healthcare professionals to thoroughly assess a patient’s medical history, current health status, and potential risks before administering pancuronium bromide. Dosage and administration should be carefully determined to minimize adverse effects and ensure patient safety during its use. As with any medication, the decision to use pancuronium bromide is made based on a careful evaluation of the individual’s specific medical needs and the potential benefits of muscle relaxation during medical procedures.
Classification of pancuronium bromide
Pancuronium bromide belongs to the pharmacological class of drugs known as neuromuscular blocking agents (NMBAs) or muscle relaxants. Specifically, it is classified as a non-depolarizing neuromuscular blocking agent.
Neuromuscular blocking agents are medications that act on the neuromuscular junction, which is the point of communication between nerves and muscles. They interfere with the transmission of nerve impulses and block the action of acetylcholine, a neurotransmitter responsible for muscle contraction. By doing so, these drugs induce muscle relaxation and temporary paralysis.
The two major categories of neuromuscular blocking agents are:
- Non-Depolarizing NMBAs: Pancuronium bromide falls into this category. These agents bind to the acetylcholine receptors on the muscle membrane, preventing the receptor from being activated and thus inhibiting muscle contraction. Non-depolarizing NMBAs do not produce muscle twitching during onset and have a longer duration of action.
- Depolarizing NMBAs: Drugs in this class, like succinylcholine, produce a brief initial muscle contraction (fasciculations) before inducing muscle relaxation. They act as agonists at the acetylcholine receptors and initially depolarize the muscle membrane before causing prolonged paralysis.
Pancuronium bromide is commonly used in medical settings for muscle relaxation during surgeries, endotracheal intubation, and mechanical ventilation in critical care situations. Its effects can be reversed using acetylcholinesterase inhibitors, such as neostigmine or edrophonium, which restore normal neuromuscular function after the procedure is completed.
It’s essential to use neuromuscular blocking agents like pancuronium bromide with caution and under the supervision of trained medical professionals to prevent potential complications, especially regarding respiratory function, and to ensure patient safety during their use.
Mechanism of Action of pancuronium bromide
Pancuronium bromide exerts its pharmacological effects by acting as a competitive antagonist at the nicotinic acetylcholine receptors located on the motor end plate of skeletal muscles. These receptors are responsible for transmitting nerve impulses from motor neurons to the muscle fibers, leading to muscle contraction.
The mechanism of action of pancuronium bromide can be summarized as follows:
- Competitive Antagonist: Pancuronium bromide competes with acetylcholine, a neurotransmitter, for binding to the nicotinic acetylcholine receptors on the motor end plate. It binds to these receptors without activating them, effectively blocking the binding sites for acetylcholine.
- Blockade of Acetylcholine Binding: By occupying the acetylcholine receptors on the muscle membrane, pancuronium bromide prevents acetylcholine from binding and activating these receptors. As a result, acetylcholine cannot trigger the muscle fiber to contract.
- Muscle Relaxation: With acetylcholine unable to activate the nicotinic receptors, the signal for muscle contraction is effectively blocked. This leads to muscle relaxation and temporary paralysis.
- Reversibility: Importantly, the effects of pancuronium bromide are reversible. Once the drug is metabolized and cleared from the body, and the concentration of acetylcholine increases, normal neuromuscular function is restored.
The temporary paralysis induced by pancuronium bromide is beneficial in various medical procedures, such as surgeries and endotracheal intubation, where muscle relaxation is necessary for proper patient management and to facilitate the intervention. It is essential to administer pancuronium bromide carefully and under the supervision of trained medical professionals. Improper use or dosage can lead to serious complications, particularly respiratory-related issues. The drug’s dosage and administration are closely monitored to ensure patient safety and minimize potential risks associated with its use. Additionally, as a neuromuscular blocking agent, pancuronium bromide is typically used in conjunction with anesthesia to ensure patient comfort during surgical procedures.
Pharmacodynamics of pancuronium bromide drug
The pharmacodynamics of pancuronium bromide refers to how the drug interacts with the body and produces its effects, particularly its neuromuscular blocking action. As a non-depolarizing neuromuscular blocking agent, pancuronium bromide acts at the neuromuscular junction, the site where nerves communicate with skeletal muscles. Here are the key pharmacodynamic actions of pancuronium bromide in detail:
- Neuromuscular Blockade: Pancuronium bromide binds competitively to the nicotinic acetylcholine receptors on the motor end plate of skeletal muscles. By doing so, it blocks the binding of acetylcholine, the neurotransmitter responsible for muscle contraction, to these receptors. The blockade of acetylcholine receptors prevents nerve impulses from reaching the muscle fibers, leading to muscle relaxation and temporary paralysis.
- Dose-Dependent Effects: The neuromuscular blocking effect of pancuronium bromide is dose-dependent. Higher doses of the drug result in more extensive neuromuscular blockade, leading to increased muscle relaxation and paralysis. The dosage of pancuronium bromide is carefully titrated based on the patient’s needs and the desired level of muscle relaxation.
- Time to Onset and Duration of Action: The onset of action of pancuronium bromide is relatively slow, typically taking around 2 to 5 minutes to reach its maximal effect. The drug’s duration of action is moderate to long, with effects lasting for approximately 60 to 90 minutes.
- Reversibility: Pancuronium bromide is a non-depolarizing neuromuscular blocking agent, meaning its effects can be reversed. After the procedure or intervention is complete, and muscle relaxation is no longer needed, the drug is metabolized and eliminated from the body. The effects are reversed using acetylcholinesterase inhibitors, such as neostigmine or edrophonium, which increase the levels of acetylcholine and restore neuromuscular function.
- Respiratory Muscle Paralysis: One of the critical effects of pancuronium bromide is the paralysis of the respiratory muscles. While this is beneficial during certain medical procedures that require controlled ventilation, it also poses a risk if the drug is not used appropriately or in patients with compromised respiratory function. Adequate ventilation and monitoring are essential during the administration of pancuronium bromide to ensure adequate oxygenation and prevent respiratory complications.
- Synergistic Effects with Anesthetics: Pancuronium bromide is often used in conjunction with general anesthetics during surgical procedures. Anesthetics can enhance the neuromuscular blocking effect of the drug, reducing the required dosage and minimizing side effects.
Overall, the pharmacodynamics of pancuronium bromide is centered around its ability to induce muscle relaxation and temporary paralysis by competitively blocking acetylcholine receptors at the neuromuscular junction. This property makes it a valuable tool in various medical settings, particularly in surgeries and critical care situations, where precise muscle control and relaxation are necessary. However, its use requires careful monitoring and expertise to ensure patient safety and optimize outcomes.
Metabolism of pancuronium bromide drug
Pancuronium bromide undergoes several steps of metabolism in the body, primarily involving the liver and excretion by the kidneys. The process of metabolism helps to break down the drug into metabolites that are more easily eliminated from the body. Here’s a detailed explanation of the metabolism of pancuronium bromide:
- Hepatic Metabolism: After administration, pancuronium bromide is primarily metabolized in the liver. The drug undergoes chemical transformations through enzymatic reactions to form various metabolites.
- Hydrolysis: One of the major metabolic pathways for pancuronium bromide involves hydrolysis. Enzymes in the liver break down the drug by hydrolyzing ester linkages present in the molecule. This hydrolysis process leads to the formation of inactive metabolites.
- Cytochrome P450 Enzymes: The hepatic metabolism of pancuronium bromide involves certain cytochrome P450 (CYP) enzymes, such as CYP3A4 and CYP2D6. These enzymes play a crucial role in breaking down the drug into its metabolites.
- N-Dealkylation: Another metabolic pathway for pancuronium bromide is N-dealkylation. In this process, a nitrogen atom is removed from the molecule, resulting in the formation of an inactive metabolite.
- Elimination: After metabolism, the inactive metabolites of pancuronium bromide are excreted from the body mainly through the kidneys. The medication and its metabolites are wiped out overwhelmingly in the pee.
- Biliary Excretion: Some of the metabolites of pancuronium bromide may also undergo biliary excretion, where they are excreted into the bile and eventually eliminated through the feces.
- Plasma Half-Life: The plasma half-life of pancuronium bromide, which represents the time it takes for half of the drug concentration to be eliminated from the bloodstream, is approximately 90 to 150 minutes in healthy individuals.
It’s important to note that individual variations in metabolism can occur due to factors such as age, liver function, genetics, and interactions with other drugs. For example, patients with impaired liver or kidney function may experience altered metabolism and excretion of pancuronium bromide, which can affect its duration of action and clearance from the body.
As with any medication, the metabolism of pancuronium bromide is carefully considered when determining the dosage and administration to ensure optimal therapeutic effects and minimize the risk of adverse reactions. Medical professionals closely monitor patients during and after the use of pancuronium bromide to ensure safe and effective outcomes.
Absorption of pancuronium bromide drug
Pancuronium bromide is administered intravenously, which means it is directly introduced into the bloodstream. As a result, absorption is not a significant factor for this drug, as it bypasses the need to be absorbed through the gastrointestinal tract.
Here’s a brief overview of how pancuronium bromide is administered and its lack of absorption concerns:
- Route of Administration: Pancuronium bromide is typically administered intravenously (IV) as an injection or as part of an IV infusion. It is given directly into a vein, allowing it to rapidly enter the bloodstream.
- Rapid Onset of Action: Due to its intravenous administration, pancuronium bromide exhibits a quick onset of action. It usually takes about 2 to 5 minutes to achieve its maximum effect, making it suitable for use in situations where rapid muscle relaxation is required, such as during endotracheal intubation or surgical procedures.
- Lack of Absorption: Since pancuronium bromide is not orally ingested or absorbed through the gastrointestinal tract, the concept of absorption, as it applies to oral medications, does not apply. Instead, the drug immediately enters the systemic circulation after being administered intravenously, leading to its pharmacological effects at the neuromuscular junction.
- Redistribution and Metabolism: After achieving its maximum effect, pancuronium bromide undergoes hepatic metabolism, as explained in the previous response. The metabolites are then excreted through the kidneys and, to a lesser extent, through the bile into the feces.
- Short Duration of Action: While pancuronium bromide has a rapid onset of action, its duration of effect is moderate to long. The drug’s effects generally last for about 60 to 90 minutes, depending on the dose and individual patient factors.
In summary, the absorption of pancuronium bromide is not a concern, as it is administered directly into the bloodstream via intravenous injection. The primary focus is on its rapid onset of action and duration of effect, along with its metabolism and elimination from the body, which are essential considerations for its safe and effective use in medical settings. Medical professionals carefully monitor patients during and after the administration of pancuronium bromide to ensure proper muscle relaxation and minimize potential risks or adverse reactions.
The volume of distribution of pancuronium bromide drug
The volume of distribution (Vd) of a drug is a pharmacokinetic parameter that indicates the theoretical volume in which the total amount of the drug would need to be uniformly distributed to produce the observed plasma concentration. It is a mathematical concept used to describe the apparent distribution of a drug in the body, and it helps to determine the extent of distribution beyond the bloodstream.
The volume of distribution is calculated using the following formula:
Vd = Total amount of drug in the body (mg) / Concentration of drug in the plasma (mg/L). The volume of distribution can vary depending on the drug’s properties, such as its molecular size, lipophilicity, protein binding, and tissue permeability. As of my knowledge cutoff in September 2021, I don’t have specific data on the volume of distribution for pancuronium bromide. The Vd for pancuronium bromide may differ between individuals based on factors such as age, weight, and health status.
To obtain the most accurate and up-to-date information on the volume of distribution for pancuronium bromide, I recommend consulting the latest pharmacokinetic references or medical literature or reaching out to a qualified healthcare professional or clinical pharmacologist.
Protein binding of pancuronium bromide drug
As of my knowledge cutoff in September 2021, pancuronium bromide is known to have a high degree of protein binding in the bloodstream. Approximately 77 to 88% of pancuronium bromide is bound to plasma proteins, primarily albumin. Protein binding refers to the extent to which a drug attaches to proteins in the blood, particularly albumin. When a drug is highly protein-bound, only the unbound or free fraction of the drug is pharmacologically active and can exert its effects on the body. The bound portion acts as a reservoir, helping to maintain a steady concentration of the drug in the bloodstream.
The high protein binding of pancuronium bromide contributes to its prolonged duration of action. Only the unbound fraction of the drug is available to interact with the neuromuscular junction and induce muscle relaxation. As the drug becomes unbound and metabolized over time, the bound fraction releases more pancuronium bromide into circulation, sustaining the effect.
It’s important to note that protein binding interactions can be affected by factors such as concurrent medications that compete for binding sites on plasma proteins, as well as changes in the patient’s health status or liver function. As always, for the most current and accurate information regarding the protein binding of pancuronium bromide or any medication, it is advisable to refer to the latest drug references, and pharmacology textbooks, or consult with a qualified healthcare professional or clinical pharmacologist.
Route of elimination of pancuronium bromide drug
Pancuronium bromide is primarily eliminated from the body through hepatic metabolism and renal excretion. Here’s a breakdown of the route of elimination for this drug:
- Hepatic Metabolism: After administration, pancuronium bromide undergoes metabolism in the liver. The drug is subject to various chemical transformations, including hydrolysis and N-dealkylation. These enzymatic reactions convert pancuronium bromide into inactive metabolites.
- Renal Excretion: The inactive metabolites of pancuronium bromide, along with a small portion of unchanged drug, are eliminated from the body primarily through the kidneys. The metabolites and unchanged drugs are filtered by the kidneys and excreted in the urine.
- Biliary Excretion: Some of the metabolites of pancuronium bromide may also undergo biliary excretion. This means they are eliminated into the bile and eventually excreted through the feces.
- Reversibility: Pancuronium bromide is a non-depolarizing neuromuscular blocking agent, and its effects are reversible. Once the drug and its metabolites are cleared from the body, and acetylcholine levels increase, normal neuromuscular function is restored.
The time it takes for pancuronium bromide and its metabolites to be eliminated from the body depends on various factors, including the individual’s kidney and liver function, the dosage of the drug, and any concurrent medications that might affect its metabolism or excretion.
As with any medication, it is crucial to consider factors such as patient characteristics, dosing, and potential drug interactions when determining the appropriate use of pancuronium bromide. Healthcare professionals closely monitor patients during and after the administration of this drug to ensure safe and effective outcomes.
The half-life of pancuronium bromide drug
As of my last update in September 2021, the half-life of pancuronium bromide is approximately 80 to 150 minutes in healthy adults. The half-life is the time it takes for the concentration of a medicine in the bloodstream to reduce by half. The duration of action of pancuronium bromide is influenced by its relatively long half-life. After administration, the drug remains active for a significant period, inducing muscle relaxation and temporary paralysis. This prolonged effect is beneficial during medical procedures where sustained muscle relaxation is required, such as surgeries or endotracheal intubation.
It’s important to note that individual variations in drug metabolism and elimination can affect the half-life of pancuronium bromide. Patients with impaired kidney or liver function may experience a prolonged half-life, leading to a slower clearance of the drug from the body. As always, for the most current and accurate information about the half-life of pancuronium bromide or any medication, I recommend consulting the latest drug references or medical literature or reaching out to a qualified healthcare professional or clinical pharmacologist.
Clearance of pancuronium bromide drug
Clearance is a pharmacokinetic parameter that represents the rate at which a drug is removed from the bloodstream. It indicates how efficiently the body eliminates a drug and is calculated as the volume of plasma from which the drug is completely removed per unit of time. Clearance is expressed in volume per time units, such as milliliters per minute (mL/min) or liters per hour (L/hr).
The clearance of pancuronium bromide is influenced by several factors, including hepatic metabolism, renal excretion, and protein binding. Here’s a detailed explanation of each aspect:
- Hepatic Metabolism: Pancuronium bromide is subject to hepatic metabolism, primarily through hydrolysis and N-dealkylation processes. These enzymatic reactions occur in the liver and convert the drug into inactive metabolites. The rate of hepatic metabolism contributes to the drug’s clearance from the bloodstream.
- Renal Excretion: After metabolism, the inactive metabolites of pancuronium bromide, along with a small portion of the unchanged drug, are eliminated from the body through the kidneys. Renal excretion plays a significant role in the overall clearance of the drug.
- Protein Binding: Pancuronium bromide has a high degree of protein binding in the bloodstream, with approximately 77-88% of the drug bound to plasma proteins, primarily albumin. The bound fraction of the drug is not cleared from the plasma since only the unbound or free fraction is pharmacologically active and available for elimination.
- Renal and Non-Renal Clearance: The total clearance of pancuronium bromide consists of both renal and non-renal clearance components. Renal clearance involves the excretion of the drug and its metabolites through the kidneys. Non-renal clearance includes the processes of hepatic metabolism and other elimination pathways, such as biliary excretion.
Overall, the clearance of pancuronium bromide is affected by its hepatic metabolism, renal excretion, and protein-binding properties. It’s important to note that individual variations, such as liver or kidney function, can influence drug clearance, which may impact the duration of action and potential accumulation of the drug in the body.
As with any medication, the clearance of pancuronium bromide is an essential consideration when determining the appropriate dosage and administration to achieve the desired therapeutic effect while minimizing the risk of adverse reactions. Healthcare professionals closely monitor patients during and after the administration of this drug to ensure safe and effective outcomes.
Toxicity of pancuronium bromide drug
Pancuronium bromide, like all medications, can be associated with potential toxicity if not used appropriately or in certain patient populations. The toxic effects of pancuronium bromide are primarily related to its pharmacological action as a neuromuscular blocking agent. Here are some details on the toxicity of pancuronium bromide:
- Respiratory Depression: One of the most significant concerns with pancuronium bromide is its potential to cause respiratory depression. The drug induces muscle relaxation, including the muscles responsible for breathing. Inappropriately high doses or rapid administration can lead to profound respiratory muscle paralysis, which may result in respiratory distress or failure.
- Cardiovascular Effects: Pancuronium bromide can cause changes in heart rate and blood pressure. It may lead to tachycardia (rapid heart rate) or bradycardia (slow heart rate) and alterations in blood pressure, particularly if the patient has pre-existing cardiovascular conditions.
- Prolonged Paralysis: Pancuronium bromide’s effects are relatively long-lasting, with a duration of action of around 60 to 90 minutes. Inadequate monitoring or excessive dosing can result in prolonged muscle paralysis, potentially leading to delayed emergence from anesthesia or difficulties in weaning from mechanical ventilation.
- Hypersensitivity Reactions: Some individuals may experience allergic reactions or hypersensitivity to pancuronium bromide or other neuromuscular blocking agents. These reactions can range from mild skin rashes to severe anaphylactic reactions, which require immediate medical attention.
- Drug Interactions: Pancuronium bromide’s effects can be potentiated or prolonged in the presence of certain medications, such as anesthetics and other neuromuscular blocking agents. Concurrent administration of other drugs that affect neuromuscular transmission or metabolism can increase the risk of adverse effects.
- Cumulative Effect: In patients with impaired liver or kidney function, the clearance of pancuronium bromide may be delayed, leading to a cumulative effect. This can increase the risk of prolonged paralysis and respiratory depression.
To minimize the risk of toxicity, pancuronium bromide should only be administered by trained healthcare professionals in a controlled medical environment. Dosing should be carefully adjusted based on the patient’s age, weight, medical history, and current health status. Proper monitoring of vital signs, respiratory function, and neuromuscular recovery is essential during the administration of pancuronium bromide.
Reversal agents such as acetylcholinesterase inhibitors (e.g., neostigmine) can be used to counteract the effects of pancuronium bromide and restore neuromuscular function if necessary. As with any medication, the decision to use pancuronium bromide should consider the potential benefits, the patient’s individual needs, and the availability of appropriate monitoring and resuscitation equipment to manage potential complications.
What is the function of the pancuronium bromide?
The primary function of pancuronium bromide is to induce muscle relaxation and temporary paralysis, primarily in the context of medical procedures and surgeries. As a non-depolarizing neuromuscular blocking agent, pancuronium bromide acts at the neuromuscular junction, which is the site where nerves communicate with skeletal muscles. Here’s a detailed explanation of the function of pancuronium bromide:
- Muscle Relaxation: Pancuronium bromide competitively binds to the nicotinic acetylcholine receptors on the motor end plate of skeletal muscles. By occupying these receptors without activating them, the drug prevents the binding of acetylcholine, the neurotransmitter responsible for muscle contraction. As a result, muscle relaxation occurs, and the ability of the nerves to communicate with the muscle fibers is temporarily blocked.
- Facilitating Intubation: One of the main medical uses of pancuronium bromide is to facilitate endotracheal intubation. Endotracheal intubation involves placing a breathing tube into the windpipe to establish an airway for patients undergoing general anesthesia or who require mechanical ventilation. Pancuronium bromide’s muscle relaxation makes the process of intubation smoother and helps prevent complications related to inadequate muscle relaxation during the procedure.
- Surgery and Anesthesia: During surgical procedures, pancuronium bromide is used to provide muscle relaxation, which is essential for surgeries requiring precise muscle control or during specific operations where muscle relaxation is necessary for better surgical access.
- Mechanical Ventilation: In intensive care units (ICUs), pancuronium bromide is used to provide muscle relaxation for patients requiring mechanical ventilation. By temporarily paralyzing the respiratory muscles, the drug ensures that the ventilator can effectively deliver breaths without interference from patient-initiated muscle movements.
- Reducing Anesthetic Requirements: When used in combination with general anesthetics, pancuronium bromide allows for reduced anesthetic requirements. By inducing muscle relaxation, the drug helps achieve surgical immobility with lower doses of anesthetics, potentially minimizing the risk of adverse effects associated with higher doses.
- Adjunct to Electroconvulsive Therapy (ECT): In some cases, pancuronium bromide is used as an adjunct to electroconvulsive therapy (ECT) to prevent excessive muscle contractions during the procedure.
It is essential to administer pancuronium bromide with caution and under the supervision of trained medical professionals. Incorrect use or dosing can lead to respiratory complications or prolonged paralysis. Reversal agents, such as acetylcholinesterase inhibitors, can be used to restore normal neuromuscular function once the drug’s effect is no longer required. The use of pancuronium bromide is carefully tailored to the individual patient’s needs, medical condition, and the specific procedure or situation requiring muscle relaxation. Proper monitoring and assessment of the patient’s response to the drug are crucial to ensure patient safety and optimal outcomes.
How long should I use an over-the-counter pancuronium bromide drug?
Pancuronium bromide is not available over-the-counter (OTC). It is a prescription medication and is not intended for self-administration or use without medical supervision. Pancuronium bromide is a potent neuromuscular blocking agent used in medical settings by healthcare professionals, typically anesthesiologists or critical care specialists. It is administered intravenously to induce muscle relaxation and temporary paralysis during specific medical procedures, surgeries, and critical care situations.
As a prescription medication, pancuronium bromide should only be used under the guidance of a qualified healthcare professional. Its use requires careful titration, monitoring, and expertise to ensure patient safety and avoid potential complications, especially related to respiratory function.
If you have any concerns or questions about medications or treatments, including pancuronium bromide, please consult your healthcare provider. They can provide personalized advice based on your specific medical needs and conditions.
How long does the drug take to work?
The onset of action of pancuronium bromide, also known as the time it takes for the drug to start working, is relatively slow compared to some other neuromuscular blocking agents. The drug is administered intravenously, and its onset of action depends on various factors, including the dose, patient’s age, weight, and general health status. Here’s a detailed explanation of the onset of action of pancuronium bromide:
- Intravenous Administration: Pancuronium bromide is typically administered intravenously (IV). The IV route allows for rapid delivery of the drug directly into the bloodstream, ensuring a quick distribution throughout the body.
- Time to Onset: The onset of action of pancuronium bromide usually occurs within 2 to 5 minutes after its IV administration. However, the exact timing can vary depending on individual factors, such as the dose and the patient’s physiological response.
- Rapid Sequence Induction: In some cases, pancuronium bromide may be used as part of a rapid sequence induction (RSI) technique during anesthesia induction. RSI involves the rapid administration of an anesthetic agent and a neuromuscular blocking agent, such as pancuronium bromide, to quickly induce unconsciousness and muscle paralysis for tracheal intubation.
- Duration of Action: After its onset of action, pancuronium bromide provides sustained muscle relaxation for approximately 60 to 90 minutes. This relatively long duration of action is beneficial during surgical procedures or critical care interventions where controlled muscle relaxation is required for an extended period.
- Reversibility: It is essential to note that pancuronium bromide is a non-depolarizing neuromuscular blocking agent, and its effects are reversible. Once the procedure or intervention is completed, and muscle relaxation is no longer necessary, the drug is metabolized and eliminated from the body. The effects can be reversed using acetylcholinesterase inhibitors, such as neostigmine or edrophonium, which restore normal neuromuscular function.
As with any medication, the dosage and administration of pancuronium bromide are carefully determined by trained medical professionals. The goal is to achieve the desired level of muscle relaxation while minimizing the risk of adverse effects, particularly those related to respiratory function. Healthcare providers closely monitor patients during and after the administration of pancuronium bromide to ensure safe and effective outcomes.
Why this Pancuronium bromide drug is prescribed?
Pancuronium bromide is prescribed for its muscle relaxant and neuromuscular blocking properties. It is used in medical settings by healthcare professionals, primarily anesthesiologists and critical care specialists, to achieve controlled muscle relaxation and temporary paralysis during specific medical procedures, surgeries, and critical care situations. Here’s a detailed explanation of why pancuronium bromide is prescribed:
- Facilitating Intubation: One of the main medical uses of pancuronium bromide is to facilitate endotracheal intubation. Endotracheal intubation involves placing a breathing tube into the windpipe to establish an airway for patients undergoing general anesthesia or who require mechanical ventilation. Pancuronium bromide’s muscle relaxation makes the process of intubation smoother and helps prevent complications related to inadequate muscle relaxation during the procedure.
- Surgical Procedures: During surgical procedures, pancuronium bromide is used to provide muscle relaxation, which is essential for surgeries requiring precise muscle control or during specific operations where muscle relaxation is necessary for better surgical access.
- Mechanical Ventilation: In intensive care units (ICUs), pancuronium bromide is used to provide muscle relaxation for patients requiring mechanical ventilation. By temporarily paralyzing the respiratory muscles, the drug ensures that the ventilator can effectively deliver breaths without interference from patient-initiated muscle movements.
- Reducing Anesthetic Requirements: When used in combination with general anesthetics, pancuronium bromide allows for reduced anesthetic requirements. By inducing muscle relaxation, the drug helps achieve surgical immobility with lower doses of anesthetics, potentially minimizing the risk of adverse effects associated with higher doses.
- Electroconvulsive Therapy (ECT): In some cases, pancuronium bromide is used as an adjunct to electroconvulsive therapy (ECT) to prevent excessive muscle contractions during the procedure.
It is important to emphasize that pancuronium bromide is a potent medication and should only be administered by trained healthcare professionals in a controlled medical environment. Its use requires careful titration, monitoring, and expertise to ensure patient safety and avoid potential complications, especially related to respiratory function.
The decision to use pancuronium bromide is carefully tailored to the individual patient’s needs, medical condition, and the specific procedure or situation requiring muscle relaxation. Proper monitoring and assessment of the patient’s response to the drug are crucial to ensure patient safety and optimal outcomes.
How does my doctor choose a Pancuronium bromide drug that’s good for me?
The selection of pancuronium bromide or any other medication depends on several factors, and your doctor will carefully consider these factors to choose the most appropriate drug for your specific medical condition and needs. Here’s how your doctor may choose a pancuronium bromide drug that’s good for you:
- Medical Condition: Your doctor will first assess your medical condition and the specific procedure or intervention requiring muscle relaxation. Different medical conditions may require different levels of muscle relaxation, and the choice of pancuronium bromide or another neuromuscular blocking agent will be based on the intended effect.
- Procedure Type: The type of medical procedure or surgery you are undergoing will influence the choice of the muscle relaxant. For example, some surgeries may require deeper muscle relaxation for better surgical access, while others may require more moderate muscle relaxation to avoid interference with specific functions.
- Duration of Action: The duration of action of the muscle relaxant is also an essential consideration. Pancuronium bromide has a relatively long duration of action, which may be beneficial for surgeries or interventions that require sustained muscle relaxation.
- Patient Characteristics: Your age, weight, medical history, and overall health status play a role in drug selection. Different patient populations may respond differently to medications, and your doctor will consider these factors when choosing the most suitable drug and dosage for you.
- Drug Interactions: Your doctor will review your current medications and medical history to ensure that there are no potential drug interactions between pancuronium bromide and other drugs you may be taking. Some medications can potentiate the effects of pancuronium bromide or increase the risk of adverse reactions.
- Individual Response: Every patient may respond differently to medications. Your doctor will monitor your response to pancuronium bromide during the procedure to ensure it is working effectively and to adjust the dosage if necessary.
- Patient Safety: Patient safety is of utmost importance. Your doctor will select a muscle relaxant that provides the necessary level of muscle relaxation while minimizing the risk of adverse effects, particularly those related to respiratory function.
It’s important to communicate openly with your doctor about your medical history, any allergies, and any medications or supplements you are currently taking. This information will help your doctor make an informed decision about the best muscle relaxant for your specific situation. Always follow your doctor’s instructions regarding the use of pancuronium bromide or any other prescribed medication. Never self-administer any medication, and seek medical attention if you have any concerns or experience unexpected side effects during or after the procedure.
What are the side effects of the Pancuronium bromide drug?
Pancuronium bromide is a potent medication used as a neuromuscular blocking agent, and like all medications, it can cause side effects. These side effects are primarily related to its pharmacological action on the neuromuscular system and its effects on other body systems. Here’s a detailed explanation of the potential side effects of pancuronium bromide:
Respiratory Effects:
- Respiratory Depression: Pancuronium bromide can cause respiratory depression, leading to a decrease in respiratory rate and depth. This can be a significant concern, especially if the drug is not carefully titrated, or in patients with compromised respiratory function.
- Apnea: In some cases, pancuronium bromide may lead to temporary apnea (cessation of breathing), particularly when high doses are administered or when used in combination with other medications affecting the respiratory system.
Cardiovascular Effects:
- Changes in Heart Rate: Pancuronium bromide can cause changes in heart rate, leading to either tachycardia (rapid heart rate) or bradycardia (slow heart rate).
- Blood Pressure Changes: The drug may cause fluctuations in blood pressure, either hypotension (low blood pressure) or hypertension (high blood pressure).
Hypersensitivity Reactions:
- Allergic reactions: Some individuals may experience allergic reactions or hypersensitivity to pancuronium bromide. These reactions can range from mild skin rashes to severe anaphylactic reactions, which require immediate medical attention.
Musculoskeletal Effects:
- Prolonged Paralysis: Pancuronium bromide’s effects can be long-lasting, with a duration of action of around 60 to 90 minutes. Inadequate monitoring or excessive dosing can result in prolonged muscle paralysis.
Gastrointestinal Effects:
- Nausea and Vomiting: Pancuronium bromide may cause nausea and vomiting as a side effect.
Central Nervous System Effects:
- Sedation: The drug may cause sedation or drowsiness in some patients.
Other Effects:
- Increased Intraocular Pressure: Pancuronium bromide may increase intraocular pressure, which is a concern for patients with certain eye conditions.
It is important to emphasize that pancuronium bromide is a potent medication and should only be administered by trained healthcare professionals in a controlled medical environment. The dose and administration should be carefully adjusted based on the patient’s individual needs, medical condition, and response to the drug. Proper monitoring and assessment of the patient’s vital signs, respiratory function, and neuromuscular recovery are crucial to ensure patient safety and prevent or manage potential side effects.
As with any medication, if you experience any unexpected or concerning side effects during or after the administration of pancuronium bromide, it is essential to seek immediate medical attention. Always follow your doctor’s instructions regarding the use of pancuronium bromide or any other prescribed medication.
What should I know regarding the storage and disposal of this Pancuronium bromide?
When it comes to the storage and disposal of medications, including pancuronium bromide, it is essential to follow specific guidelines to ensure safety and prevent harm to yourself, others, and the environment. Here’s a detailed explanation of what you should know regarding the storage and disposal of pancuronium bromide:
Storage:
- Keep in Original Packaging: Store pancuronium bromide in its original packaging, typically a vial or ampule. The packaging provides important information, such as the expiration date, which is crucial for determining the drug’s potency and safety.
- Temperature: Store pancuronium bromide at room temperature, typically between 20°C to 25°C (68°F to 77°F). Avoid exposure to extreme temperatures, such as excessive heat or freezing, as it can affect the drug’s stability and efficacy.
- Protect from Light: Some medications, including pancuronium bromide, can be sensitive to light. Store the drug in a container that protects it from direct sunlight or excessive light exposure.
- Keep Out of Reach of Children and Pets: Store pancuronium bromide in a secure location, out of the reach of children and pets. The drug is a potent medication and should only be used under the supervision of trained healthcare professionals.
- Do Not Use Expired Medication: Check the expiration date on the packaging, and do not use pancuronium bromide if it has expired. Expired medications may not be effective or safe to use.
- Separate from Other Medications: Store pancuronium bromide separately from other medications to avoid mix-ups or confusion.
Disposal:
- Follow Local Regulations: When it comes to disposing of medications, including pancuronium bromide, it’s essential to follow your local regulations and guidelines. Some regions have specific guidelines for safe medication disposal to protect the environment and prevent misuse.
- Do Not Flush Down the Toilet: Do not flush pancuronium bromide or any other medication down the toilet or drain. Flushing medications can also contaminate water sources and/or harm aquatic life.
- Medication Take-Back Programs: Check if there are any medication take-back programs or drug disposal locations in your area. Many pharmacies, hospitals, or law enforcement agencies offer safe medication disposal options.
- Mix with Unpalatable Substance: If there are no specific drug disposal programs available, you can mix pancuronium bromide with an unpalatable substance, like coffee grounds or cat litter, and place it in a sealed container before throwing it in the rubbish. This forestalls unintentional ingestion by creatures or individuals.
- Remove Personal Information: Before disposing of the medication packaging, remove any personal information to protect your privacy.
If you have any questions or concerns regarding the storage or disposal of pancuronium bromide or any other medication, consult your pharmacist or healthcare provider for guidance. They can also provide specific instructions established on your location and local regulations. Always prioritize safety and responsible medication use and disposal.
In what conditions would it be advisable for me to check with my medic before taking this medication?
Since pancuronium bromide is a prescription medication used as a neuromuscular blocking agent, it is not taken by individuals on their initiative. Instead, it is administered in medical settings by qualified healthcare professionals, such as anesthesiologists or critical care specialists, during specific procedures or surgeries. Therefore, there are no circumstances where an individual should check with their doctor before taking pancuronium bromide.
If you are scheduled to undergo a medical procedure or surgery that may require the use of pancuronium bromide or any other medication, it is essential to communicate openly with your healthcare provider. They will review your medical history, current medications, and any potential drug allergies or contraindications to ensure that pancuronium bromide or any other prescribed medication is safe and appropriate for you.
During this pre-procedure evaluation, you should inform your doctor if you have any of the following circumstances or conditions:
- Allergies: If you have a known allergy to pancuronium bromide or any other neuromuscular blocking agents, it is crucial to inform your doctor to avoid potential adverse reactions.
- Medical Conditions: Your doctor needs to know about any underlying medical conditions you have, such as heart problems, lung diseases, kidney or liver issues, or neuromuscular disorders.
- Medications: Make sure to inform your doctor about any prescription medications, over-the-counter drugs, supplements, or herbal remedies you are taking. Some medications can interact with pancuronium bromide, affecting its effectiveness or increasing the risk of side effects.
- Pregnancy or Breastfeeding: If you are pregnant or breastfeeding, your doctor needs to consider the potential risks and benefits of using pancuronium bromide during these periods.
- Previous Anesthesia Experience: If you have had prior experiences with anesthesia or muscle relaxants, share your experiences and any adverse reactions you may have had.
- Recent Illness or Infection: Your doctor will need to know if you have had any recent illness or infection that could affect your response to pancuronium bromide.
- Pre-existing Neuromuscular Disorders: If you have a pre-existing neuromuscular disorder, your doctor will need to carefully evaluate the use of pancuronium bromide to avoid complications.
It is essential to have a comprehensive discussion with your healthcare provider before any medical procedure involving pancuronium bromide or any other medications. This will ensure that you receive safe and effective care tailored to your individual needs and medical condition. Remember that pancuronium bromide is a potent medication that should only be administered by qualified medical professionals in a controlled medical environment.
Can Pancuronium bromide drugs cause allergic reactions?
Yes, pancuronium bromide can cause allergic reactions in some individuals. Allergic reactions are immune responses triggered by the body’s immune system when it identifies a specific substance, in this case, pancuronium bromide, as harmful. These reactions can vary in severity and may range from mild skin rashes to severe and life-threatening anaphylactic reactions. Here are the details regarding allergic reactions to pancuronium bromide:
Hypersensitivity and Allergies: Pancuronium bromide is a synthetic compound, and like any medication, it can potentially elicit hypersensitivity reactions in susceptible individuals. Allergic reactions occur when the body’s immune system recognizes pancuronium bromide as a foreign substance and releases chemicals, such as histamine, in response. These chemicals cause the symptoms associated with an allergic reaction.
Symptoms of Allergic Reactions: Allergic reactions to pancuronium bromide may manifest in various ways, including:
- Skin Reactions: Itching, hives (urticaria), redness, or skin rashes.
- Respiratory Symptoms: Difficulty breathing, wheezing, shortness of breath, or chest tightness.
- Cardiovascular Symptoms: Rapid or irregular heart rate, low blood pressure, or fainting.
- Gastrointestinal Symptoms: Nausea, vomiting, or abdominal discomfort.
Anaphylactic Reaction: In rare cases, an allergic reaction to pancuronium bromide can progress to a severe and life-threatening condition known as anaphylaxis. Anaphylaxis is a medical emergency that needs immediate awareness. Symptoms of anaphylaxis may include difficulty breathing, swelling of the face and throat, a drop in blood pressure, severe hives, and loss of consciousness.
Risk Factors: Some individuals may be at a higher risk of experiencing an allergic reaction to pancuronium bromide. People with a history of allergies to other medications, neuromuscular blocking agents, or other substances may be more susceptible.
Precautions: Before administering pancuronium bromide or any medication, healthcare providers carefully assess a patient’s medical history, including any known allergies. They may perform skin testing or use other methods to evaluate the risk of an allergic reaction in susceptible patients.
Treatment: If an allergic reaction occurs during the administration of pancuronium bromide, medical personnel are trained to respond immediately. Treatment may include discontinuation of the medication, administration of antihistamines or corticosteroids, and, in severe cases, the use of epinephrine to counteract the severe allergic response.
Due to the potential risk of allergic reactions, pancuronium bromide is administered under close medical supervision, and healthcare providers are prepared to manage any adverse reactions promptly. If you suspect that you may be allergic to pancuronium bromide or any other medication, inform your healthcare provider immediately. It is crucial to communicate any known allergies to healthcare providers to ensure your safety during medical procedures or treatments.
What should I do if I forget a dose of the Pancuronium bromide drug?
If you are prescribed pancuronium bromide, it is important to understand that the medication is not taken by individuals on their initiative. Instead, it is administered by qualified healthcare professionals, such as anesthesiologists or critical care specialists, in medical settings during specific procedures or surgeries. Therefore, as a patient, you do not have control over the administration of pancuronium bromide, and there is no risk of forgetting a dose.
Pancuronium bromide is given intravenously and is carefully administered by trained medical personnel based on the specific needs of the procedure and the patient. The dosage and timing of pancuronium bromide administration are precisely determined by healthcare professionals, taking into account factors such as the patient’s weight, age, medical condition, and response to the drug. As a patient, it is essential to communicate openly with your healthcare provider about any medical history, allergies, or pre-existing conditions before any medical procedure involving pancuronium bromide or any other medication.
If you have any questions or concerns about the medications you are receiving, including pancuronium bromide, do not hesitate to discuss them with your healthcare provider. They will provide you with the necessary information and address any potential concerns you may have. Always prioritize safety and trust the expertise of your medical team when it comes to the administration of medications during medical procedures.
Enhancing Healthcare Team Outcomes rocuronium bromide drug
Rocuronium bromide is a neuromuscular blocking agent used in medical settings to provide muscle relaxation during procedures, surgeries, and mechanical ventilation. To enhance healthcare team outcomes when using rocuronium bromide, collaboration, and effective communication among the members of the healthcare team are essential. Here are some key aspects that can contribute to improved outcomes:
- Interprofessional Collaboration: A multidisciplinary approach involving anesthesiologists, surgeons, nurses, respiratory therapists, and other healthcare professionals is crucial when using rocuronium bromide. Each team member plays a specific role in patient care and safety, and effective collaboration ensures that everyone is working together toward common goals.
- Proper Dosing and Administration: Accurate dosing and administration of rocuronium bromide are critical to achieving the desired level of muscle relaxation while minimizing the risk of adverse effects. Healthcare professionals should carefully calculate the appropriate dosage based on the patient’s weight, age, and medical condition.
- Patient Assessment and Monitoring: Regular patient assessment and monitoring are essential during the administration of rocuronium bromide. Monitoring should include vital signs, respiratory function, neuromuscular blockade, and level of sedation. Close monitoring helps detect any adverse reactions promptly and allows for timely interventions.
- Airway Management: Since rocuronium bromide can cause respiratory muscle paralysis, airway management is vital to ensure adequate ventilation. Proper intubation and mechanical ventilation are necessary to maintain oxygenation and prevent respiratory complications.
- Reversal Agents: Healthcare professionals should be familiar with the use of acetylcholinesterase inhibitors, such as neostigmine, as reversal agents to counteract the effects of rocuronium bromide once muscle relaxation is no longer needed.
- Patient Safety Protocols: Adherence to patient safety protocols, such as the World Health Organization (WHO) Surgical Safety Checklist, helps reduce the risk of errors and ensures that critical steps are not missed during the administration of rocuronium bromide and other medications.
- Emergency Preparedness: The healthcare team should be well-prepared to handle any adverse reactions or emergencies that may arise during the use of rocuronium bromide. This includes having necessary medications, equipment, and emergency protocols in place.
- Communication with Patients: Clear and empathetic communication with patients and their families is crucial in providing information about the use of rocuronium bromide, potential risks, and the reasons for its administration. Educating patients and families helps reduce anxiety and promotes patient satisfaction.
- Documentation and Record Keeping: Accurate documentation of the dosage, administration, patient response, and any adverse reactions is essential for continuity of care and legal purposes.
By focusing on interprofessional collaboration, patient safety, proper dosing, monitoring, and communication, the healthcare team can enhance outcomes and ensure the safe and effective use of rocuronium bromide for patients undergoing medical procedures.
What is the dosage of the Pancuronium bromide drug?
The dosage of pancuronium bromide is determined by qualified healthcare professionals, typically anesthesiologists or critical care specialists, based on the specific medical procedure, the patient’s weight, age, medical condition, and response to the drug. The medication is managed intravenously and requires cautious titration to accomplish the ideal degree of muscle unwinding while at the same time limiting the gamble of antagonistic impacts.
It is important to note that pancuronium bromide is a potent medication and should only be administered by trained medical professionals in a controlled medical environment. Patients do not self-administer pancuronium bromide; rather, it is given during medical procedures, surgeries, or critical care interventions by healthcare professionals.
The dosing of pancuronium bromide may vary depending on the purpose of its use:
- Intubation and Surgical Procedures: For endotracheal intubation or surgical procedures requiring muscle relaxation, the typical initial adult dose of pancuronium bromide is approximately 0.06 to 0.1 mg/kg administered intravenously. Subsequent doses may be administered based on the patient’s response and the duration of the procedure.
- Mechanical Ventilation in the ICU: In the intensive care unit (ICU) setting, pancuronium bromide may be used for muscle relaxation in patients requiring mechanical ventilation. The initial adult dose is usually around 0.04 to 0.1 mg/kg, with additional doses as needed based on patient response and ventilation requirements.
- Electroconvulsive Therapy (ECT): For adjunctive use during ECT, pancuronium bromide is given at a dose of approximately 0.06 to 0.1 mg/kg.
It is essential to note that the dosing of pancuronium bromide may be adjusted for pediatric patients, elderly individuals, or patients with specific medical conditions, such as liver or kidney impairment.
Because pancuronium bromide is administered by healthcare professionals during medical procedures, it is crucial for the medical team to closely monitor the patient’s response, vital signs, and neuromuscular function throughout the procedure. The goal is to achieve the appropriate level of muscle relaxation for the specific procedure while ensuring patient safety and minimizing the risk of complications, particularly those related to respiratory function.
As with any medication, healthcare professionals consider the patient’s characteristics and needs when determining the dosage of pancuronium bromide. Patients should trust their medical team’s expertise and follow their instructions for the safe and effective use of this medication.
What other drugs interact with the pancuronium bromide drug?
Pancuronium bromide, being a potent neuromuscular blocking agent, can interact with other medications, potentially affecting its effectiveness or increasing the risk of adverse reactions. Healthcare professionals must be aware of possible drug interactions when administering pancuronium bromide to patients. Here are some examples of medications that may interact with pancuronium bromide:
- Anesthetic Agents: Other anesthetic agents, such as inhalational anesthetics (e.g., isoflurane, sevoflurane) and intravenous anesthetics (e.g., propofol, thiopental), may potentiate the effects of pancuronium bromide. This combination may result in deeper muscle relaxation and prolonged paralysis. Dosage adjustments may be necessary to avoid excessive neuromuscular blockade.
- Cholinesterase Inhibitors: Cholinesterase inhibitors, such as neostigmine or pyridostigmine, are used as reversal agents to counteract the effects of pancuronium bromide once its use is no longer needed. These agents enhance the action of acetylcholine at the neuromuscular junction, effectively reversing the neuromuscular blockade caused by pancuronium bromide.
- Aminoglycoside Antibiotics: Aminoglycoside antibiotics, such as gentamicin or tobramycin, can enhance the neuromuscular blockade caused by pancuronium bromide. This interaction may lead to prolonged paralysis, especially in patients with impaired renal function who may have increased levels of aminoglycosides in their system.
- Calcium Channel Blockers: Calcium channel blockers, such as verapamil or diltiazem, may enhance the effects of pancuronium bromide by reducing calcium influx at the neuromuscular junction, thereby increasing neuromuscular blockade.
- Magnesium Sulfate: Magnesium sulfate, often used for tocolysis in obstetric care or cases of preeclampsia, can enhance the neuromuscular blockade caused by pancuronium bromide.
- Other Neuromuscular Blocking Agents: Concurrent use of other neuromuscular blocking agents, such as succinylcholine or vecuronium, may result in additive effects, leading to excessive muscle relaxation and prolonged paralysis.
- Beta-Adrenergic Blockers: Beta-adrenergic blockers, such as propranolol or metoprolol, may potentiate the effects of pancuronium bromide, potentially leading to increased muscle relaxation.
Healthcare professionals need to review a patient’s medication history thoroughly and consider possible drug interactions before administering pancuronium bromide. Dosage adjustments or the use of alternative medications may be necessary in some cases to ensure patient safety and optimal outcomes.
Patients should inform their healthcare providers about all the medications they are currently taking, including prescription drugs, over-the-counter medications, herbal supplements, and vitamins. This information helps the healthcare team make informed decisions regarding the use of pancuronium bromide and other medications to provide safe and effective care.
Precautions to take when using this pancuronium bromide drug
When using pancuronium bromide, which is a potent neuromuscular blocking agent, several precautions should be taken to ensure safe and effective administration. Healthcare professionals, including anesthesiologists and critical care specialists, should adhere to these precautions to minimize the risk of complications and provide optimal care to patients. Here are the precautions to consider when using pancuronium bromide:
- Trained Healthcare Professionals: Only qualified and trained healthcare professionals, experienced in the administration of neuromuscular blocking agents, should handle and administer pancuronium bromide. They should have a comprehensive understanding of the drug’s pharmacology, dosing, and potential adverse effects.
- Proper Dose and Titration: The dosage of pancuronium bromide should be carefully calculated based on the patient’s weight, age, medical condition, and specific procedure or intervention. The drug should be titrated to achieve the desired level of muscle relaxation without causing excessive paralysis.
- Monitoring: Continuous monitoring is essential during the administration of pancuronium bromide. Vital signs, neuromuscular response, and respiratory function should be closely monitored to detect any adverse reactions promptly.
- Reversal Agents: Healthcare professionals should have appropriate reversal agents, such as cholinesterase inhibitors (e.g., neostigmine), readily available to reverse the neuromuscular blockade caused by pancuronium bromide once its effects are no longer needed.
- Respiratory Support: Adequate respiratory support should be available during the administration of pancuronium bromide, especially in patients undergoing mechanical ventilation or those with compromised respiratory function.
- Individualized Approach: The use of pancuronium bromide should be individualized for each patient, taking into account their medical history, allergies, age, and any other relevant factors that may affect drug response.
- Drug Interactions: Healthcare professionals should be aware of potential drug interactions with other medications the patient may be receiving. Some drugs may potentiate or diminish the effects of pancuronium bromide, affecting its safety and efficacy.
- Patient Education: Patients and their families should be informed about the purpose, risks, and benefits of using pancuronium bromide during medical procedures. They should also be aware of any potential side effects or adverse reactions.
- Anaphylaxis Preparedness: Healthcare professionals should be prepared to manage anaphylactic reactions promptly, as pancuronium bromide can rarely trigger severe allergic responses.
- Disposal: Proper disposal of pancuronium bromide and any related medical waste should be done following local regulations and guidelines to protect the environment and prevent misuse.
- Controlled Environment: Pancuronium bromide should only be administered in a controlled medical environment, such as a hospital or surgical center, where appropriate equipment and skilled personnel are available to manage potential complications.
By adhering to these precautions, healthcare professionals can ensure the safe and effective use of pancuronium bromide and provide optimal care to patients during medical procedures and critical care situations. Patient safety remains the top priority, and any concerns or unexpected reactions should be promptly addressed by the healthcare team.
Conclusion
In conclusion, pancuronium bromide is a potent neuromuscular blocking agent used in medical settings, primarily during anesthesia and critical care procedures. It acts by impeding the transmission of nerve motivations at the neuromuscular intersection, prompting muscle unwinding and impermanent loss of motion. This effect is crucial for facilitating endotracheal intubation, providing surgical muscle relaxation, and supporting mechanical ventilation in intensive care units. Pancuronium bromide’s dosage and administration require careful consideration by qualified healthcare professionals, such as anesthesiologists and critical care specialists. The drug’s dose is individualized based on the patient’s weight, age, medical condition, and specific procedure. Close monitoring of the patient’s response, vital signs, and respiratory function is essential to ensure safety and optimal outcomes.
While pancuronium bromide is generally well-tolerated when administered by trained medical personnel, it is not without risks. Potential side effects include respiratory depression, cardiovascular changes, and hypersensitivity reactions, which can vary in severity. Anaphylactic reactions, though rare, can be life-threatening and require immediate medical attention.
Disclaimer: The following article is supplied for informational purposes only and does not include professional advice. The data contained in this article depends on the writer’s comprehension and understanding of the subject at the hour of composing. The content of this article should not be considered exhaustive, and/or additional research or consultation with experts may be necessary. The reader is prompted to independently verify the accuracy, currency, and relevancy of the information provided.
The perspectives and suppositions addressed in this article are those of the writer and don’t be guaranteed to mirror the authority strategy or position of any association, organization, or person. Any connection or mention of specific products, services, or organizations does not imply endorsement or recommendation by the author or the publisher. While every effort has been made to provide the accuracy and reliability of the information presented, the author and the publisher assume no responsibility for any errors, omissions, and/or damages arising from the use of the information provided in this article.
FAQs
What is the conventional name for pancuronium bromide?
Pavulon (pancuronium bromide) Mixture is a neuromuscular hindering expert employed to give skeletal muscle loosening up during tracheal intubation and operation. Pavulon is accessible in conventional structures.
What advantages does pancuronium provide?
Restorative Advantages – PANCURONIUM has a place with the gathering of prescriptions called muscle relaxants used to diminish and ease muscle compression (extreme pressure in the muscles) during medical procedures, different methodologies, and concentrated care. Quieting muscles while on a breathing machine is likewise utilized.
What is the intricacy of pancuronium?
Pancuronium is somewhat utilized in the liver and discharged as the parent compound or as a metabolite by the kidneys. Critical renal or hepatic brokenness might prompt delayed loss of motion. Different difficulties of pancuronium result from its vagolytic impact, which can bring about tachycardia and hypertension.
Does pancuronium increment pulse?
Pancuronium 0.08 mg kg”‘ constrained a basic development in beat (20%), immaterial changes in vein pressure, and huge changes in systolic time extends reasonably with an ostensible positive inotropic movement.
What is the cure for pancuronium?
Pyridostigmine bromide, neostigmine, or edrophonium, related to atropine or glycopyrrolate, will for the most part alienate the skeletal muscle relaxant activity of pancuronium bromide. Acceptable inversion can be decided by the sufficiency of skeletal muscle tone and by the ampleness of breath.
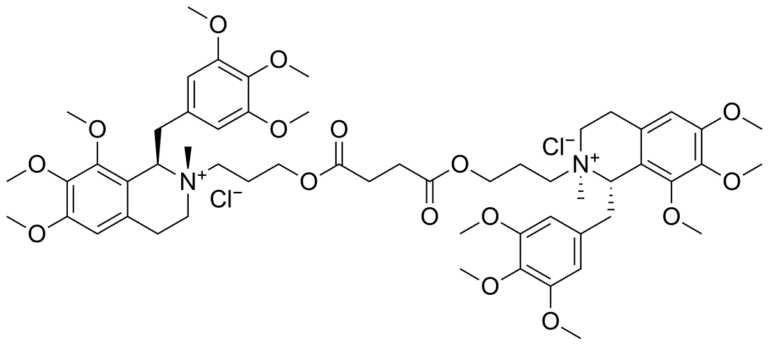
What elements makeup pancuronium bromide?
Nondepolarizing neuromuscular blocking agent Pancuronium Bromide is referred to chemically as the aminosteroid 2-16-dipiperidino-5-androstane-3,17-diol diacetate dimethobromide, C35H60Br2N2O4. A fine white unscented powder is solvent in water, liquor, and chloroform.
What are the dosages of pancuronium?
At first, 0.04 to 0.1 mg/kg IV followed by steady portions beginning at 0.01 mg/kg IV; these additions marginally increment the greatness of the bar and fundamentally increment the term of the bar because countless myoneural intersections are as yet impeded when there is need for more medication.
What are the cardiovascular impacts of pancuronium?
Pancuronium created tachycardia and expanded blood vessel pressure; this cardiovascular excitement has been credited to vagolytic activity, an arrival of norepinephrine from the thoughtful nerve terminals, or hindrance of neuronal take-up of norepinephrine.
For what reason is pancuronium bromide utilized in deadly infusion?
Pancuronium bromide and its fresher cousins are individuals from a class called neuromuscular blockers. Those medications deaden the body’s skeletal muscles. In a deadly infusion, the impact of the medication is to loosen up the chest wall muscles and the stomach in the now oblivious prisoner.