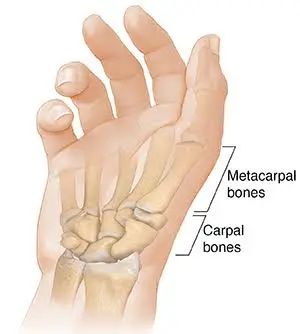
Carpometacarpal Joint
What is Carpometacarpal Joint?
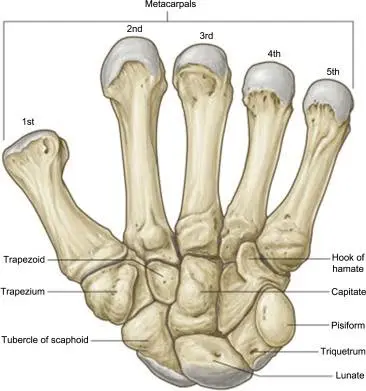
The articulations between the carpal bones (carpals) & metacarpal bones (metacarpals) of the hand are called the carpometacarpal (CMC) joints. There are five carpometacarpal joints with the thumb’s carpometacarpal joint, which is also understood as the trapeziometacarpal joint standing as considerably specialized & flexible.
The remaining 4 carpometacarpal (CMC) joints are active plane synovial joints that attach the medial 4 metacarpal bones (2nd, 3rd, 4th, 5th metacarpal) with the distal row of carpal bones (trapezium, trapezoid, capitate, hamate). The 3 most medial carpometacarpal (CMC) joints collectively create a group named the typical carpometacarpal (CMC) joint.
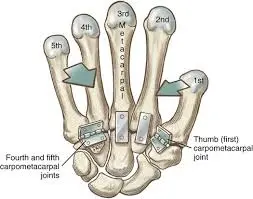
The four CMC joints exhibit varying degrees of mobility from medial to lateral. Metacarpals 2 and 3 have limited mobility, metacarpal 4 can glide to a small degree, while metacarpal 5 can glide extensively, allowing for flexion and rotation. These features make the medial 4 carpometacarpal (CMC) joints extremely stable, demonstrating a powerful association between the wrist & hand, while even delivering sufficient flexibility to allow palm cupping & object holding while thumb opposition actions.
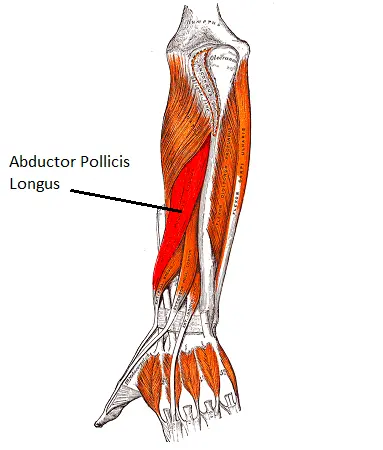
Flexion of these joints is produced by the flexor pollicis longus and brevis muscles, assisted by the opponens pollicis and adductor pollicis. An extension is primarily affected by the abductor pollicis longus, administered by the extensor pollicis longus and brevis. Adduction is taken out by the adductor muscle of the hand, while abduction is mainly accomplished by the abductor pollicis longus and brevis, aided by the extensors muscles of the hand.
| Type | Structural classification: Synovial ellipsoid or complex saddle joints Functional classification: Synovial plane joint Degrees of freedom: 2nd & 3rd CMC joint nonaxial, 4th & 5th CMC joint biaxial |
| Articular surfaces | Anterior & posterior interosseous nerves, deep & dorsal branches of the ulnar nerve (C7-C8) |
| Ligaments | Dorsal and palmar carpometacarpal ligaments, interosseous ligament |
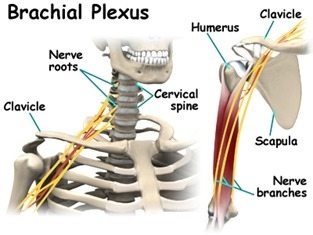
| Innervation | Anterior and posterior interosseous nerves, deep and dorsal branches of ulnar nerve (C7-C8) |
| Blood supply | Palmar and dorsal carpal anastomoses |
| Movements | 2nd-3rd CMC joints: Limited anteroposterior gliding (translation) 4th CMC joint: Flexion-extension 5th CMC joint: Flexion-extension, internal-external rotation |
Thumb
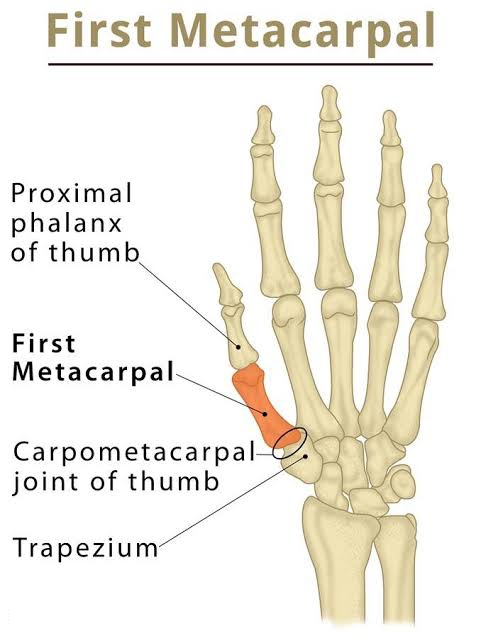
The carpometacarpal joint of the thumb, also known as the first carpometacarpal joint or the trapeziometacarpal joint (TMC), is a crucial joint that connects the trapezium to the first metacarpal bone. It recreates an essential part of the regular functioning of the thumb. Osteoarthritis of the TMC is a highly debilitating condition, particularly prevalent among elderly women, occurring up to twenty times more frequently than average.
The pronation-supination movement of the first metacarpal bone is especially significant for the action of opposition. The range of motion in the first carpometacarpal joint is influenced by the joint’s anatomical structure, the surrounding capsule, ligaments, and the coordination of involved muscles. In cases where the first metacarpal bone is not properly aligned with the trapezium, such as in cases of hypoplasia, the first CMC joint may become subluxated, meaning it is slightly displaced towards the radius.
The joint capsule provides flexibility, allowing a wide range of movements and permitting a distraction of approximately 3 mm. The stability of the joint is reinforced by ligaments and tendons. The dorsal side of the capsule is slightly thicker compared to other regions.
The first carpometacarpal joint is a common site for the development of osteoarthritis, particularly among postmenopausal women.
Ligaments
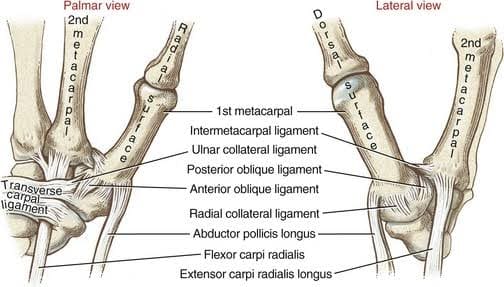
The characterization of the digit & representations of ligaments of the 1st carpometacarpal joint (CMC) can vary wildly in anatomical books. According to Imaeda et al. (1993), the following ligaments are considered the most important for stabilizing the thumb:
- Anterior oblique ligament (AOL): This muscular & wide intracapsular ligament initiates from the palmar tubercle of the trapezium & inserts onto the palmar tubercle of the 1st metacarpal. It is taut during abduction, extension, and pronation. The AOL is known to have a crucial retaining function and may become elongated or absent in cases of CMC joint arthritis.
- Ulnar collateral ligament (UCL): The UCL is an extracapsular ligament located near the AOL. It originates from the flexor retinaculum & connects to the ulnopalmar tubercle of the 1st metacarpal. It becomes taut during abduction, extension, and pronation. In the context of CMC joint arthritis, the UCL is often found elongated. However, the significance of the UCL can vary among researchers.
- First intermetacarpal ligament (IML): This ligament connects the bases of the second and first metacarpals, with its fibers intertwining with those of the UCL at its insertion onto the ulnopalmar tubercle of the first metacarpal. It becomes taut during abduction, opposition, and supination. Several researchers have identified the IML as the most important restraining structure of the first CMC joint. While some question its ability to stabilize the joint on its own, it is widely accepted that, together with the UCL, it plays a significant role in joint stability.
- Posterior oblique ligament (POL): The POL is an intracapsular ligament that originates from the dorsoulnar side of the trapezium to the ulnar-palmar tubercle of the 1st metacarpal. Although not considered a major ligament in the first CMC joint, it tightens during forced adduction and radial abduction.
- Dorsoradial ligament (DRL): Similar to the POL, the DRL is not considered crucial to the stability of the first CMC joint. It attaches the dorsal sides of the trapezium & the 1st metacarpal.
It’s important to note that the exact number and names of these ligaments may vary in different sources, and the significance attributed to each ligament can also differ among researchers.
Movements
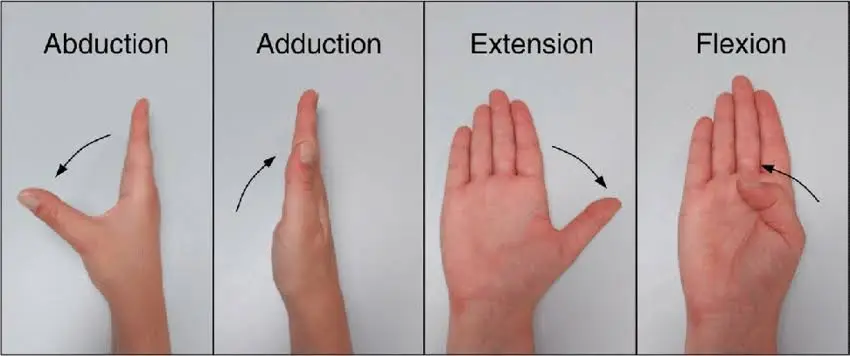
In this articulation, different activities are permitted, containing flexion & extension in the plane of the hand, abduction & adduction in a plane perpendicular to the hand, circumduction, & opposition.
Opposition is the motion that obtains the end of the thumb into connection with the volar surfaces of the slightly bent fingers. This motion is reduced by a little tilted facet on the anterior lip of the saddle-shaped articular surface of the more significant multangular bone (trapezium). The flexor muscles tighten the connected domain of the articular surface of the metacarpal bone into this facet, during which the adductors bring out the motion of opposition.
Flexion of this joint is achieved by the flexor pollicis longus and brevis muscles, assisted by the opponens pollicis and the adductor pollicis.
The extension is primarily carried out by the abductor pollicis longus, with assistance from the extensor pollicis longus and brevis.
Adduction is performed by the adductor muscle, while abduction is primarily achieved by the abductor pollicis longus and brevis, with support from the extensors.
The range of motion (ROM) for the 1st carpometacarpal (CMC) joint contains 53° of flexion/extension, 42° of abduction/adduction, and 17° of rotation. The planes and axes of movement for the thumb’s metacarpophalangeal (MP) and CMC joints involve abduction and adduction occurring in a plane perpendicular to the palm, often referred to as “palmar abduction.” Flexion and extension of these joints occur in a plane parallel to the palm, commonly known as “radial abduction,” as the thumb moves toward the radial side of the hand. Abduction and adduction happen around an anteroposterior axis, while flexion and extension occur around a lateral axis.
For easier understanding, the thumbnail can be considered as resting in the frontal plane of the thumb. Abduction and adduction of the first CMC (and MP) joints take place in this plane, while flexion and extension of the first CMC, MP, and interphalangeal (IP) joints occur in a plane perpendicular to the thumbnail. This remains consistent regardless of how the first metacarpal bone is rotated during opposition and repositioning.
Sexual dimorphism
There are notable differences between the male and female thumb carpometacarpal (CMC) joints. In females, the measure of the trapezial articular surface is much shorter resembling the metacarpal surface, & its shape even varies from that regarded in males. While most carpometacarpal joints of the thumb suggest more useful congruence in the radioulnar direction instead of the dorsovolar direction, female CMC joints till to be less globally congruent resembled male joints.
These differences in the size and shape of the articular surfaces contribute to variations in the overall structure and function of the thumb CMC joint between males and females. It is important to consider these distinctions when studying and understanding the biomechanics and clinical aspects of the thumb joint.
Evolution
A significant development in the evolution of the first ray, including the thumb, can be observed in dinosaurs, where a primitive form of autonomy emerged. However, it was not until approximately 70 million years ago that a true differentiation of the thumb occurred in primitive primates. The distinctive shape of the human thumb carpometacarpal (TMC) joint can be traced back approximately 5 million years ago.
Throughout evolution, the human thumb CMC joint has acquired a particular positioning concerning the stable second and third CMC joints. This positioning includes approximately 80° of pronation, 40° of abduction, and 50° of flexion, following an axis passing through the aforementioned stable joints.
These evolutionary changes reflect the adaptation and refinement of the human thumb, enabling its remarkable dexterity and versatility in various tasks and activities.
Fingers
The second metacarpal primarily articulates with the trapezoid, and to a lesser extent, with the trapezium and capitate.
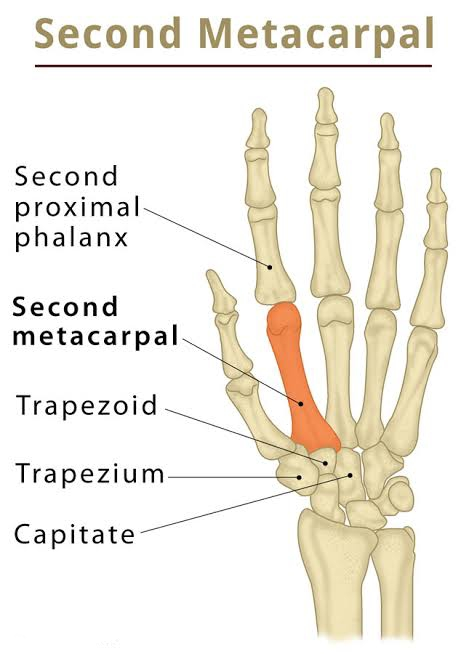
- The third metacarpal primarily articulates with the capitate.
- The fourth metacarpal articulates with both the capitate and hamate.
- The fifth metacarpal articulates with the hamate.
Additionally, the four ulnar metacarpals articulate with their adjacent metacarpals at the intermetacarpal articulations.
These articulations among the metacarpal bones play a vital role in maintaining the stability and functionality of the hand, allowing for a wide range of movements and providing support for gripping and manipulating objects with precision.
Ligaments
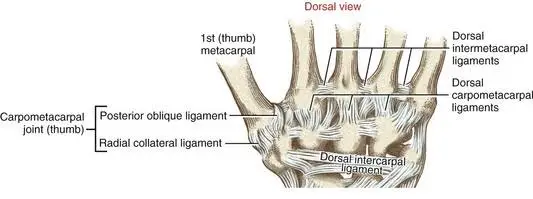
The four carpometacarpal (CMC) joints are reinforced by robust transverse ligaments and comparatively weaker longitudinal ligaments. These include the dorsal carpometacarpal ligaments and the volar or palmar carpometacarpal ligaments.
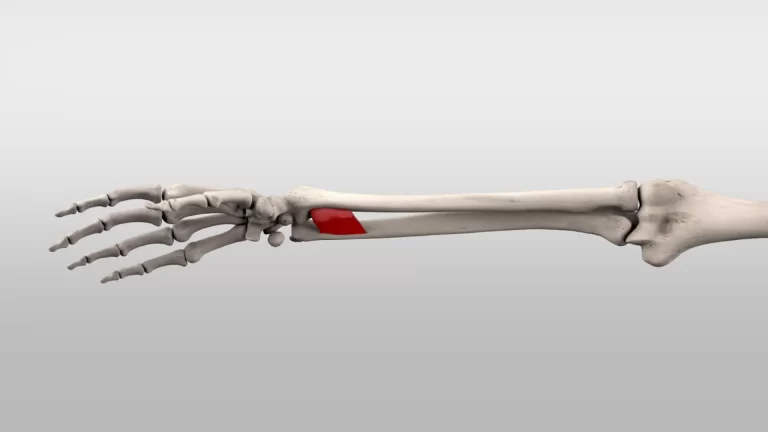
The interosseous ligaments are composed of short and sturdy fibers, and they are localized to specific regions of the carpometacarpal articulation. These ligaments connect the adjacent surfaces of the third and fourth metacarpal bones with the contiguous inferior angles of the capitate and hamate.
The presence of these ligaments provides essential stability and support to the CMC joints, ensuring proper alignment and facilitating coordinated movement of the bones during hand function.
Movements
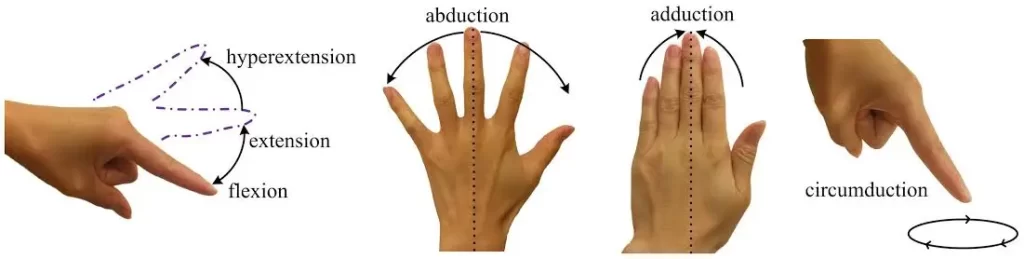
The carpometacarpal (CMC) joints of the second through fifth digits are classified as arthrodial joints. The observable range of motion in these joints is most prominent in the distal heads of the metacarpal bones. The degree of motion gradually decreases from the fifth to the second CMC joints.
The second to fifth CMC joints are considered synovial ellipsoidal joints, primarily allowing flexion and extension. However, the second and third joints are nearly immobile, practically possessing zero degrees of freedom. Nonetheless, they are capable of slight anteroposterior gliding (translation) movements. Additionally, the second and third CMC joints exhibit a small degree of flexion-extension motion, with approximately 11 degrees of flexion-extension for the second CMC joint and 7 degrees for the third CMC joint. These two joints establish a stable axis for the other three CMC joints. While the 4th CMC joint illustrates visual mobility the 1st joint is a saddle joint with 2 degrees of freedom. In addition to flexion and extension, it enables abduction and adduction, along with a limited amount of opposition. The combined movements of the fourth and fifth CMC joints allow the fingers to oppose the thumb effectively.
The unique characteristics and range of motion in each CMC joint contribute to the intricate functionality and precision of hand movements.
Function
The finger carpometacarpal (CMC) joints, along with the thumb, contribute to the palmar arch system. The distal row of carpal bones forms the proximal transverse arch of the palm. The flexibility of the first, fourth, and fifth metacarpal heads around the fixed second and third metacarpal heads enhances the concavity of this arch, creating a flexible structure known as the distal transverse arch. Additionally, each finger has its longitudinal arch. Concurrently, these arches permit the palm & digits to coordinate optimally with things while grasping, facilitating palmar cupping. This maximizes surface contact, enhances stability, and increases sensory feedback. The mobile parts of the palmar arch system are stabilized by the deep transverse metacarpal ligament.
During finger flexion, muscles that cross the finger CMC joints contribute to palmar cupping. The oblique opponens digiti minimi muscle acts specifically on the fifth CMC joint, the only muscle solely acting on the CMC joints. Its position allows for optimal flexion and rotation of the fifth metacarpal bone around its long axis. Palmar arching is also improved when the flexor carpi ulnaris (connect to the pisiform) & intrinsic hand muscles connected to the transverse carpal ligament accomplish on the hook system. The steady 2nd and 3rd CMC joints are betrayed by the radial-wrist muscles containing the flexor carpi radialis, extensor carpi radialis longus, & extensor carpi radialis brevis. The solidity of these 2 CMC joints is a useful transformation that improves the efficiency of these muscles at the midcarpal & radiocarpal joints.
These interactions and adaptations in the finger CMC joints and their associated muscles are crucial in optimizing hand function, facilitating grasping, and enhancing overall hand stability.
Synovial membranes
The synovial membrane of the wrist and carpus is a continuation of the membrane found in the intercarpal joints. In some cases, the joint between the hamate bone and the fourth and fifth metacarpal bones may have a separate synovial membrane.
Overall, there are five synovial membranes observed in the wrist and carpus:
- The first membrane extends from the lower end of the ulna to the ulnar notch of the radius and lines the upper surface of the articular disk.
- The 2nd membrane prolongs from the articular disk & the lower end of the radius beyond to the bones of the first row of carpals bone below.
- The third membrane, the most extensive, passes between the adjacent edges of the two rows of carpal bones. In some cases, when one of the interosseous ligaments is absent, it may extend between the bones of the second row to the carpal ends of the second, third, fourth, and fifth metacarpal bones.
- The 4th membrane extends from the margin of the trapezium to the 1st metacarpal bone of the thumb.
- The 5th membrane drives between the adjoining margins of the triangular (trapezium) & pisiform.
It is worth noting that occasionally, the fourth and fifth carpometacarpal joints may possess their distinct synovial membrane.
These synovial membranes play a crucial role in providing lubrication and facilitating smooth movement within the wrist and carpal joints.
Clinical significance
Osteoarthritis of the carpometacarpal joints is a form of joint disease characterized by the deterioration of both the joint cartilage and the underlying bone. Specifically, when this condition affects the thumb, it is referred to as trapeziometacarpal osteoarthritis.
Carpometacarpal bossing is the presence of a small, fixed protrusion over the joint. This term describes the development of an immovable prominence in the carpometacarpal region.
These conditions can cause pain, stiffness, and reduced mobility in the affected joints, often impacting daily activities and hand function.
FAQs
What is an example of a carpometacarpal joint?
The carpometacarpal joint of the thumb (pollex), also understood as the 1st carpometacarpal joint/the trapeziometacarpal joint (TMC) because it unites the trapezium to the 1st metacarpal bone, recreates an irreplaceable part in the regular functioning of the thumb.
Is carpometacarpal a saddle joint?
The carpometacarpal (CMC) of the thumb is a saddle joint that enables a broad range of motion (ROM) & is mainly liable for the usual agility of human prehension. This joint encountered at the very base of the thumb is subject to extensive physical pressures throughout life.
Which kind of joint is the carpometacarpal of the thumb?
The thumb carpometacarpal (CMC) joint a biconcave-convex saddle joint is the representation between the 1st metacarpal of the thumb & the trapezium bone.
What is the difference between the CMC joint and the MCP joint?
Metacarpophalangeal Joint (MCP): The MP joint is where the metacarpal bone encounters the phalanx bone directed to as the “knuckle.” These joints are elemental permitting us to bend & extend our fingers.Carpometacarpal Joint (CMC Joint): The CMC joint is found at the base of the Metacarpal bone.
What is the first carpometacarpal joint injury?
The symptoms related to carpometacarpal joint damage are identical to those of arthritis of joint, containing: Pain, stiffness, & swelling at the bottom of the thumb. Pain, stiffness, & swelling that happens after gripping/pinching exercises such as turning a doorknob, buttoning buttons, cutting vegetables, etc.
What causes CMC joint pain?
Most usually, CMC joint arthritis is related to repetitious gripping/pinching activities over a prolonged duration of time. These may contain operating scissors, driving, and precise writing with a pen/pencil. For patients who create thumb arthritis, symptoms usually exacerbate when these movements are persisted.


One Comment