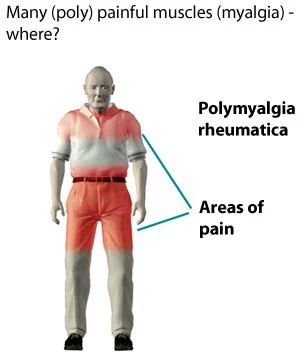
Polymyalgia Rheumatica
What is Polymyalgia rheumatica?
Polymyalgia indicates “multiple muscle pains.” Rheumatica indicates “changing” or “in flux.” Polymyalgia rheumatica is an inflammatory disease that generates muscle pain and stiffness, especially in the shoulders and hips. The disease develops most frequently in people aged 65 and more aged, and it might be connected to another inflammatory disease called giant cell arteritis.
Epidemiology
The annual incidence of polymyalgia rheumatica per 100,000 people of age more or equal to 50 years was seen to be between 58 to 96 in the predominantly white populations. Incidence rates rise with age until 80 years.
Polymyalgia rheumatica – PMR has been noted as the second most familiar inflammatory autoimmune rheumatic disorder after rheumatoid arthritis in some mostly white populations. Polymyalgia rheumatica – PMR is much less familiar in Black, Asian, and Hispanic populations.
Symptoms of Polymyalgia Rheumatica
The signs and symptoms of polymyalgia rheumatica usually appear on both sides of the body and might contain:
- Aches or pain in your shoulder joints
- Aches or pain in your upper arms, neck, hips, buttocks, or thighs
- Stiffness in involved sites, especially in the morning or after being inactive for a time
- Limited range of movement in involved sites
- Pain or stiffness in your elbows, wrists, or knees
You might also have more-general signs and symptoms, involving:
- Mild fever
- Fatigue
- A general feeling of not being well (malaise)
- Loss of appetite
- Unintended weight loss
- Depression
What causes polymyalgia rheumatica?
The cause of polymyalgia rheumatica isn’t learned. Yet, its believed that specific genes and gene variations may raise your risk of developing it.
Environmental aspects may also play a part in the development of the disease. New cases of polymyalgia rheumatic are frequently diagnosed in cycles and generally happen seasonally.
This indicates that there may be an environmental stimulus, like a viral infection, that causes the disease. The rapid beginning of symptoms also indicates that polymyalgia rheumatica may be activated by an infection. Yet, no such connection has been seen.
Risk factors
You are more probable to get polymyalgia rheumatica and giant cell arteritis if you have specific risk factors. These contain:
Age. They appear almost exclusively in persons more senior than age 50, generally in a patient in their late 60s and their 70s.
Sex. Females get these diseases more often than males do.
Ethnic and racial background. They are more familiar in Caucasians, particularly populations of Northern European ancestry, but are also marked in peoples of further ethnic and racial backgrounds.
Differential Diagnosis
Polymyalgia rheumatica has nonspecific characteristics that many different entities could mimic. Further entities should be excluded from the studies, as deemed required by clinical suspicion, before analyzing polymyalgia rheumatica – PMR. Some important differentials are listed below:
- Rheumatoid arthritis
- GCA
- Anti-neutrophil cytoplasmic antibody (ANCA) related vasculitis
- Inflammatory myositis and statin-induced myopathy
- Gout and calcium pyrophosphate dihydrate crystal deposition disease (CPPD) disorder
- Fibromyalgia
- Overuse or degenerative shoulder pathology eg. osteoarthritis, rotator cuff tendinitis and tendon tear, adhesive capsulitis
- Cervical spine disorders eg. radiculopathy, osteoarthritis
- Crown dens syndrome
- Hypothyroidism
- Obstructive sleep apnea
- Depression
- Viral infections such as EBV, hepatitis, human immunodeficiency virus, parvovirus B19
- Systemic bacterial infections, septic arthritis
- Cancer
- Diabetes
Diagnosis
Physical examination
On physical assessment, diffuse tenderness is generally proof over the shoulder without localization to precise structures. The ache generally restricts the active shoulder range of movement, and the passive range of movement could be normal when carefully analyzed. Restriction of neck and hip motions because of aches is also familiar. Muscle tenderness of arms, neck, and thigh may be present. Even though the person might complain of non-specific weakness, muscle strength is generally intact on a more thorough study.
Lab test
Doctors or physician base the diagnosis of polymyalgia rheumatica on symptoms and the outcomes of a physical inspection. Doctors or physicians do further tests, like blood tests, to determine polymyalgia rheumatica from other diseases. Blood tests generally contain the following:
Erythrocyte sedimentation rate (ESR), C-reactive protein levels, or both: In a patient with polymyalgia rheumatica, outcomes of both tests are generally very high, demonstrating active inflammation.
Complete blood count: This examination is done to study for anemia and high platelet count, which generally evolves in a patient with polymyalgia rheumatica.
Thyroid-stimulating hormone (TSH): This examination is done to rule out hypothyroidism, which can induce weakness and occasionally ache of the shoulder and hip muscles.
Creatine kinase: This examination is done to study muscle tissue injury (myopathy), which can generate weakness and aches in the shoulder and hip muscles. If the level of creatine kinase in the blood is elevated, muscle injury is probable. Muscle injury is absent in a patient with polymyalgia rheumatica, so the creatine kinase level is normal.
Rheumatoid factor and anti-cyclic citrullinated peptide antibodies testing: These antibodies are present in up to 80% of patients with rheumatoid arthritis but not in those with polymyalgia rheumatica. This examination assists doctors or physicians differentiate between the two.
The diagnosis is also helped by how patients answer to corticosteroids because most patients with polymyalgia rheumatica feel much better very fast when managed with low doses of corticosteroids.
Treatment of Polymyalgia Rheumatica
Medical treatment
Polymyalgia rheumatica – PMR is commonly treated with a long period of corticosteroids. There is no agreement on the initial dosage and following titration of the corticosteroid dosage. Some recommend an initial dose of 15-20 mg/day of prednisone and then a gradual tapering over several weeks or months to see a keeping dosage.
Although polymyalgia rheumatica – PMR reacts very well to corticosteroids, there is still a concern for the adverse outcomes that happen with long-term steroid use. This contains osteoporosis, diabetes, worsening of cataracts, hypertension, muscle weakness, and infection.
Persons assuming corticosteroids must have their blood pressure, blood sugar, and body weight routinely inspected. Due to the raised risk for osteoporosis, vitamin D and calcium supplements should be started when the corticosteroids are started.
Complete clinical remission may carry up to 5 years to happen.
People’s reactions to corticosteroids can be dramatic, but the medications arrive with their side effects. Long-term corticosteroid use can raise a patient’s probability of developing the subsequent conditions:
- Depression
- High cholesterol
- Weight gain
- High blood pressure
- Osteoporosis
- Cataracts
- Diabetes
Physiotherapy treatment in Polymyalgia Rheumatica
The main purpose of physiotherapy for polymyalgia is to relieve any inflammation, pain, and stiffness you are experiencing using a mixture of strategies. Further plans contain boosting energy levels, education to enhance lifestyle, pain management, and assisting sort sleep habits.
Physiotherapy may contain:
- Pain modalities
- Manual procedures
- Stress management and relaxation methods
- Massage
- Heat or ice (ice) for muscle and joint or junction pain
- Electrical stimulation
- Therapeutic ultrasound ( to decrease inflammation)
- Hydrotherapy
- Stretching and strengthening exercises for involved sites to control deconditioning
- Cardiovascular exercise to enhance overall health and fitness levels
- Education on how to make lifestyle modifications that may involve your situation advice on diet, controlling sleep, and managing rest
- Acupuncture
- Functional activities to assist issues associated with daily living
Physiotherapy, involving a range of motion exercises for the shoulders, can assist to decrease aches and maintain mobility.
Weight-bearing activity is useful for supporting bone strength and decreasing the risk of osteoporosis.
Weight-bearing activity is anything such as walking, jogging, tennis, dancing, or lifting weights, where some force or the weight of the body is affected by bones during the activity. This is in contrast to swimming, for instance, where the water helps the weight of the body. Walking is generally the most appropriate weight-bearing activity for a patient with polymyalgia rheumatica.
Sitting for any length of time may generate stiffness, making movements like driving more challenging. Stop from time to time on a long travel to stretch your arms, shoulders, and legs.
Simple steps like a hot bath or shower can assist to reduce aches and stiffness, either first thing in the morning or after activity.
Exercise for polymyalgia rheumatica generally means light physical exercise. The activities are meant to assist to enhance the symptoms and provide you with an overall understanding of well-being.
A patient who suffers from polymyalgia rheumatica – PMR notice that they find the best results with exercises like cycling, walking, swimming, and light running. Cardio activity not only assists you to keep a healthy weight, but it also lowers pressure on bones and joints or junctions. Some patients see that raising light weights is also useful for the bones.
Flexibility and stretching activities, involving yoga and tai chi activities, are good choices. When it arrives to yoga, you should bring it gradually and advance only if you are satisfied and feel no ache.
With polymyalgia rheumatica – PMR. it’s essential to limit pressure since it can worsen symptoms. Deep breathing activities can be very useful. You can attempt it lying down. You gradually breathe in and visualize your body calming all over. It is a fine idea to rehearse this several times a day. It only brings a few minutes.
It is essential to set realistic plans when you’re exercising with polymyalgia rheumatica – PMR. Most patients do well when they create their routine gradually in five to 10-minute blocks of time. If you accept this method, before you know it, you will be up to 30 minutes, which is the suggested amount of daily activity.
Polymyalgia rheumatica is uncomfortable but it can be controlled with the right therapy, involving diet and activity. When you feel as if you have tried everything but still aren’t obtaining better or you are obtaining worse, you should pursue a medical alert.
Stretching – Stretching can assist to enhance your range of movement and relieve pain.
Massage – Massage therapy includes using a massage therapist to manage the soft tissues in your body.
They may utilize their hands or a machine like an ultrasound device to do this. It can assist reduce tension, stress, and pain.
Living with polymyalgia rheumatica
Steroid therapy is generally very useful in treating polymyalgia rheumatica. Yet, because it can raise your risk of obtaining osteoporosis, it’s essential to think about further risk factors associated with this disease.
Smoking or drinking a lot of alcohol will raise your risk of creating osteoporosis.
Providing you obtain sufficient calcium and vitamin D, and that you do some weight-bearing activity will decrease the risk of obtaining osteoporosis.
Keeping active
If you have polymyalgia rheumatica, you’ll require to see the right balance between rest and exercise. Too much activity is probable to make your symptoms more harmful, but exercise generally helps to reduce aches and stiffness in the muscles of the hips, shoulders, and thighs.
Diet and nutrition
Steroid therapy decreases the quantity of calcium in the body.
If you’re on steroid therapy, it’s suggested you aim for daily input of 7001200 mg of calcium.
A pint of milk a day, concurrently with a reasonable quantity of different foods that have calcium, should be sufficient.
Calcium and vitamin D
Calcium is an important nutrient for supporting good bone health, while vitamin D helps the absorption of calcium into the body. People with PMR must contain these in their diet, as corticosteroids can induce bone loss with long use.
Some dairy products, like milk and cheese, are useful references to calcium. Non-dairy meals that are high in calcium contain:
- soybeans
- okra
- kale
- spinach
- sardines
- salmon
Good sources of vitamin D contain:
- cheese
- fatty fish, like mackerel or tuna
- egg yolk
- mushrooms
products reinforced with vitamin D, like specific cereals or bread
If a patient is unable to contain these foods in their diet, they can assume calcium and vitamin D supplements.
Healthful or good fats
Fats are an important nutrient. The patient should avoid some kinds of fats, like trans-fats, but many useful fats exist, and patients with polymyalgia rheumatica – PMR should contain them in a balanced diet.
Omega-3 fatty acids have anti-inflammatory effects that may assist to decrease symptoms of polymyalgia rheumatica – PMR Foods that include high quantities of omega-3 contain:
- fish oils, like cod liver oil or salmon oil
- mackerel
- sardines
- eggs
- flaxseeds
- flax milk
- chia seeds
- walnuts
Anti-inflammatory foods
Many foods contain anti-inflammatory possessions. Ingesting these foods as part of a balanced diet may also assist to relieve the symptoms of polymyalgia rheumatica – PMR.
- tomatoes
- fatty fish
- berries
- almonds
- green leafy vegetables
- olive oil
Meal plan
Many combinations of foods can assist to decrease symptoms and the risk of side effects from a drug in a patient with polymyalgia rheumatica – PMR. The following meal plan documents two choices per meal, as well as some healthy snacks:
Breakfast
- eggs and salmon on wholemeal bread
- a bowl of fortified cereal with dairy or plant-based milk spread with flaxseeds and blueberries
Lunch
- a tuna salad
- a turkey breast sandwich on wholemeal bread, using home-cooked turkey rather than packaged pieces
Dinner
- chicken and steamed vegetables with brown rice
- baked cod with a side of cooked vegetables
Snacks
- fresh fruit
- a mix of walnuts and almonds
Foods to avoid
Some foods are connected to rising levels of inflammation. Patients with polymyalgia rheumatica – PMR should avoid these foods to control making symptoms worse.
Foods related to raised inflammation contain:
- refined carbohydrates, like white bread or white rice
- fried foods, like french fries
- sugary drinks
- processed meats, like salami or hotdogs
- red meat
- margarine
- foods with added sugar
- alcohol
Prognosis
When the diagnosis is completed promptly, and proper therapy is started, polymyalgia rheumatica – PMR has an outstanding prognosis. Mortality among people with polymyalgia rheumatica is not greatly raised compared to the general inhabitants.
Complications
Symptoms of polymyalgia rheumatica can significantly affect your capability to complete everyday activities, like:
- Reaching out of bed, standing up from a chair, or bringing out of a car
- Combing your hair or bathing
- Getting dressed
- These problems can impact your social interactions, fitness, physical exercise, sleep, and general well-being.
FAQ
Is polymyalgia rheumatica a serious condition?
If you have polymyalgia rheumatica, you are at a more increased risk of acquiring a disease known as giant cell arteritis (GCA). This includes inflammation of the blood vessels known as arteries. This requires urgent therapy as there’s a risk of permanent loss of your eyesight or a stroke with giant cell arteritis.
Does polymyalgia rheumatica go away?
Although your symptoms should enhance within a few days of beginning therapy, you’ll likely require to continue bringing a low dose of prednisolone for almost 2 years. Polymyalgia rheumatica mostly improves gradually on its own after this time. Yet, there’s a possibility it will return after therapy stops.
What is the difference between polymyalgia rheumatica and polymyalgia?
Polymyalgia, or polymyalgia rheumatica, is an inflammatory condition of the muscle. The cause is debatable but it is considered to be an autoimmune condition in which the body’s immune system attacks the connective tissues. The immediate symptoms are extreme stiffness and aches in the muscles of the shoulder, neck, and hip regions.
Can you live a normal life with polymyalgia rheumatica?
Patients with polymyalgia rheumatica – PMR generally respond well to therapy and most ultimately heal entirely from the condition within one to five years. With proper therapy and routine follow-up care, people with polymyalgia rheumatica – PMR, and even those who create GCA, can experience a full and fruitful life.
What is a natural steroid for inflammation?
Omega-3 fatty acids, which are abundant in fatty fish like cod, are among the most powerful anti-inflammatory accessories. These supplements may assist fight several kinds of inflammation, involving vascular inflammation.





One Comment