Brainstem Stroke
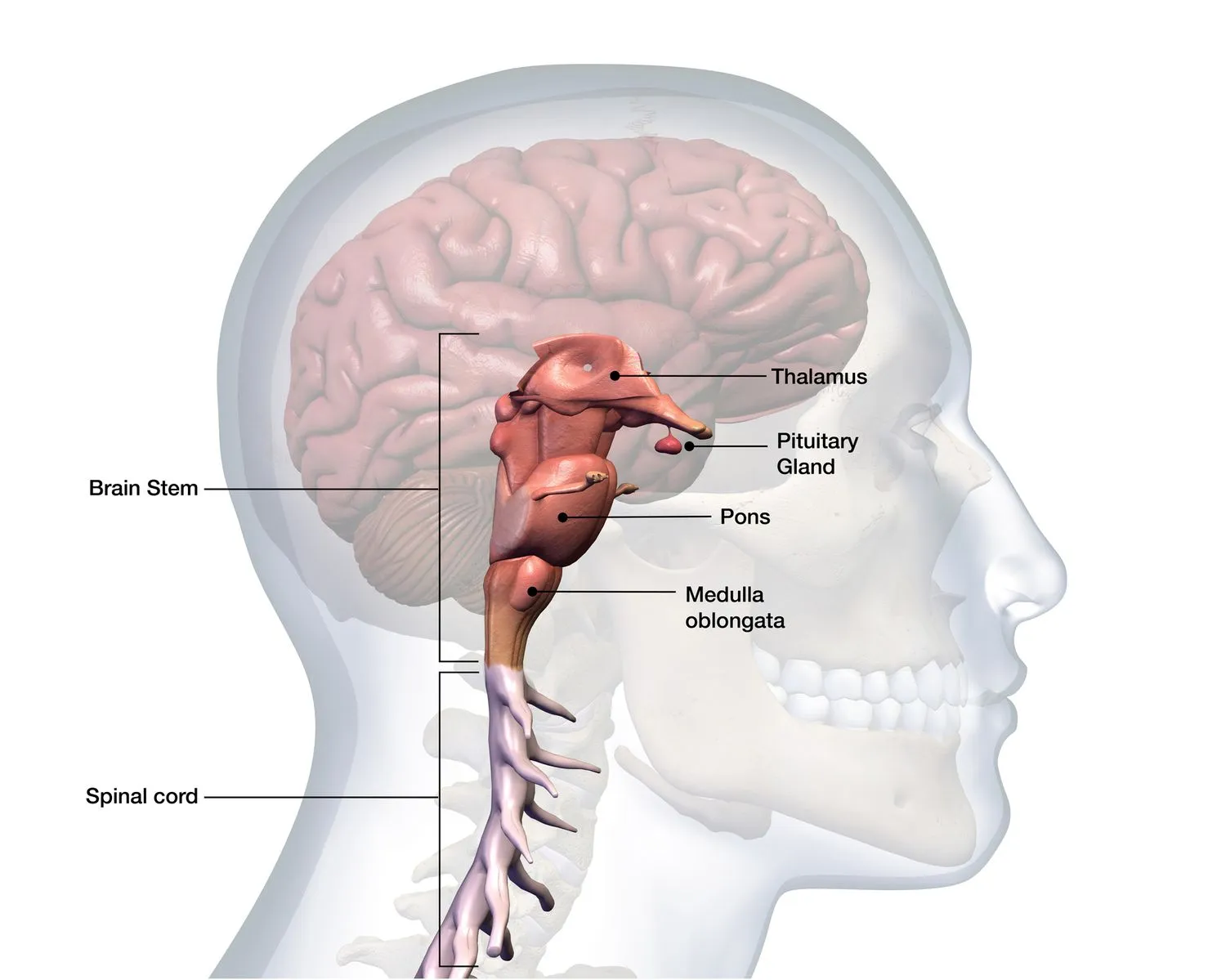
What is Brainstem Stroke?
According to the World Health Organization (WHO), stroke is the second leading reason of death and the third leading reason of disability worldwide. A Brainstem stroke happens when the blood supply to a portion of the brainstem is interrupted, either due to a clogged artery or a leaking blood vessel. The brain stem is found at the bottom of the brain and is liable for receiving and relaying details throughout the body. The brain stem controls fundamental body functions, like:
- breathing
- swallowing
- eye movement
- facial movement and sensation
- hearing
- heart rate
- blood pressure
Brain stem strokes can involve a patient’s fundamental bodily functions and may conduct to long-term difficulties.
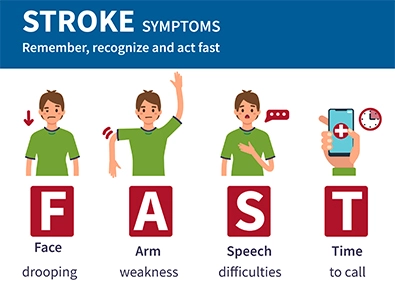
An acronym, FAST, describes the telltale indications that a stroke is taking place:
Face. The face evolves weak or droopy, with the result generally more observable on one side
Arm. One arm evolves numb or weak, and there may be a problem lifting it
Speech. Speaking evolves hard, and the involved patient’s voice evolves slurred
Time to call. If any of the above is detected, emergency assistance should be contacted immediately.
Types of strokes
There are two main kinds of strokes, both of which can involve the brain stem:
Ischemic stroke
Ischemic strokes happen when blood clots develop in the narrow arteries in the head or neck, trimming off the blood supply to a region of the brain.
Ischemic strokes are the most familiar type, accounting for 87 percent of all strokes. Approximately 10 percent of all ischemic strokes involve the brain stem.
A transient ischemic attack (TIA), also known as a mini-stroke or a warning stroke happens when the blood supply to the brain is interrupted shortly. TIAs – transient ischemic attacks cause milder symptoms than whole ischemic strokes, and most symptoms go out within an hour.
Hemorrhagic stroke
Hemorrhagic strokes or brain bleeds happen when a fragile blood vessel leaks or cracks open, producing swelling and pressure. This pressure harms tissues and cells in the brain.
Hemorrhagic strokes are less familiar than other kinds of stroke, but they account for 40 percent of all stroke deaths.
Causes of Brainstem Stroke
Brain stem strokes are induced by the blood supply to the region of the brain stem getting trimmed off, either due to a blockage in the blood vessels (ischemic stroke) or due to bleeding in the blood vessels providing the brain stem (hemorrhagic stroke).
Ischemic stroke causes
Ischemic stroke happens when a blood vessel of the brain evolves blocked. This can occur as a result of several various situations, involving most generally:
- Atherosclerosis
- Small vessel disease
- Atrial fibrillation
In rarer circumstances:
- Arterial dissection, eg. due to trauma or fibromuscular dysplasia
- Certain blood clotting issues known as coagulopathies, eg. polycythemia, or as an effect of hormonal drugs
- Inflammation of the blood vessels, called vasculitis, eg. giant cell arteritis
- Sickle cell condition
Hemorrhagic stroke causes
In a hemorrhagic stroke, the injury is caused by bleeding in or near the brain. The consequent accumulation of blood coming out of the bleed starts to put stress upon and harms the brain tissue covering the bleeding area. This initial damage can lead to additional swelling and inflammation within the brain, placing it under more stress.
Although a big portion of the brain injury from a hemorrhagic stroke happens because of the initial bleeding, persistent bleeding and later swelling can guide to even more difficulties. That is why it is so essential to get a stroke managed as fast as possible.
Risk Factors
Anyone can contain a stroke, but precise genetic factors, like a family record, race, gender, and age placed some patients at higher risk for stroke than others.
According to the American Stroke Association, females have more strokes than males and are more probable to die from a stroke than males.
Some risk factors that are unique to women contain:
- use of hormone replacement treatments
- long-term use of birth control pills in combination with further risk factors, like smoking
- pregnancy
- People of African-American and Hispanic descent are also at a more elevated risk of stroke.
The prevalence of strokes happens in a patient over the age of 65. Yet, research indicates that the rate of stroke hospitalizations and the reality of stroke risk factors in younger grown-ups has risen greatly.
Medical diseases that increase the risk of stroke contain:
- high blood pressure
- high cholesterol
- arterial fibrillation (AFib)
- diabetes
- obesity
- cardiovascular disease (CVD)
Lifestyle risk factors
A patient cannot maintain genetic factors, but they can manage lifestyle factors that raise the risk of stroke. Behaviors that raise high blood pressure or the risk of clot building can lead to a more elevated risk of stroke.
Behaviors that can increase the risk of stroke contain:
- smoking tobacco
- excessive alcohol use
- illegal drug use
- a sedentary lifestyle
- poor diet
Symptoms of Brainstem Stroke
Because the brain stem maintains a combination of motor functions, strokes in this region of the brain generate a diverse range of symptoms.
Brain stem strokes can disrupt vital bodily roles, like:
- breathing
- swallowing
- heart rate
The brain stem accepts varied signals from the brain and transmits them to various regions of the body. Brain stem strokes disrupt these signs, which is why patients feel physical symptoms, involving numbness or weakness in the arms, face, or legs.
Other familiar stroke symptoms contain:
- dizziness
- loss of balance
- vertigo
- blurred or double vision
- difficulties with speech or swallowing
- a headache
- confusion
Ischemic brain stem stroke symptoms
Vertigo and dizziness. A brain stem stroke can generate a patient to sense like they have failed a feeling of where their body is in space. Vertigo is the feeling that the body is moving when someone is even standing or sitting yet. This feeling may also show a sensation of nausea and thereafter lead to vomiting.
Changes to hearing. Some ischemic brain stem strokes can show the perception of sounds when none are present, otherwise called tinnitus. The someone involved may also evolve more sensitive to specific sounds or frequencies, a condition called hyperacusis.
Changes to eye movements. One or both of the patient’s eyes may shift unusually during and after a brain stem stroke. The eyes may involuntarily shift from side to side or up and down. One eye may remain off-center, or the eyelid may seem droopy. The involved patient’s pupils may evolve smaller. The tracks the eyes are involved by a brain stem stroke can generate vertigo and dizziness defined above and may also show double vision.
Loss of coordination of muscle control Medically called ataxia, this is when the involved somebody is unable to maintain their muscles adequately. This can teach them to lose balance or fall to the bottom.
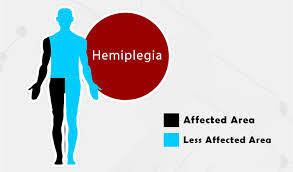
Defect on one side of the body. Otherwise called hemiparesis, this can involve the whole of the body or precise sites, like the tongue, face, or arms
Loss of ability to speak. Otherwise called dysarthria, someone involved in brain stem stroke may find it hard to speak in the manner that they generally do. Vocabulary may be slurry, or somebody may not be capable to talk at all. Different regions of the mouth, throat, or tongue may be involved by a brain stem stroke generating problems in swallowing, for instance.
Loss of body feeling. Somebody involved in brain stem stroke might see it more difficult to sense pain or shifts in temperature. This sensation may only involve specific regions of the body, like the arms, face, chest, or tongue. They may also perceive feelings in incorrect locations, such as when the foot is touched, it may sense like the leg is touched.
Difficulty swallowing. There may be an uncommon feeling on the tongue, the interior of the mouth, or the throat. This can also donate to problem swallowing, speaking, or eating.
Unusual breathing patterns. Someone may find it hard to breathe as they generally would. Doctors or physicians may require to take action to support the patient’s breathing during therapy.
Locked-in syndrome is a rare disease that generally occurs when there is an injury to the region of the brain stem known as the pons, eg. via a stroke. One of the causes the pons is essential is because it transmits data between the brain and the spinal cord. Locked-in syndrome happens when all of these signals that are essential in maintaining muscle motion in the body are disrupted. The regions of the brainstem that regulate facial motion and speaking are also involved during locked-in syndrome:
- A patient is quadriplegic, which suggests they have small or no capability to move their legs, arms, or torso
- They are incapable to speak
- They stay conscious and capable to perceive the world
- A patient involved in this syndrome typically can only roll their eyes and blink after the stroke has carried place. Their capability to breathe and swallow may also be involved.
Symptoms of brain stem hemorrhages
A hemorrhagic stroke in the blood vessels providing the brain stem is much rarer than an ischemic stroke. Yet, when bleeding does happen in this region of the brain, then the results are generally severe, and there is a high risk of the patient not prevailing the stroke.
The following symptoms are all familiar results of a brain stem hemorrhage:
- Incapability to see straightforward with eyes rolling out of their normal position
- Weakness in both the arms and the legs
- A problem in eating, breathing, or swallowing
- Loss of consciousness and coma
Diagnosis
A brain scan can assist define:
- If a stroke has carried the place
- Whether the stroke is hemorrhagic or ischemic
- The damage that has been generated to the brain thus far
- It can also assist to see any possible brain abnormalities that may have contributed to or generated the stroke.
Given the risk of ongoing harm from an untreated stroke, a brain scan must be taken out promptly after the involved patient gets to a hospital.
CT scan
A ct scan is normally one of the first examinations made after a supposed stroke because it is much faster than an MRI scan. CT scans utilize X-Ray technology.
MRI scan
A magnetic resonance imaging (MRI) scan utilizes radio waves and a strong magnetic field to create a detailed picture of the interior of the body. An MRI scan generally delivers a more precise image than a CT scan, so could be useful given harm in the brain stem can be very little.
Stroke, angiography, and contrast dye
In the early phases of a brain stem stroke, the blockage or bleeding in the brain stem may be too difficult to notice by a standard CT scan. In this issue, a doctor or physician may insert a small quantity of dye in the blood before conducting the scan.
In both a computed tomography angiogram (CTA scan) and a magnetic resonance angiogram (MRA), the dye is generally injected via an intravenous drip in the arm. It can also be injected into a vein on the back of the hand or through a narrow tube, called a catheter, via another blood vessel.
Treatment of Brainstem Stroke
Medical treatment
Emergency maintenance will be required. The heart and lungs may require support. A tube may also be set to assist with breathing. A brain stem stroke is a medical crisis. It needs immediate therapy to save lives and decrease the risk of lasting difficulties. Therapy depends on the location, type, and severity of the stroke:
Ischemic stroke
Therapy for an ischemic stroke includes restoring blood flow by stopping the clot. Techniques contain the following:
Clot-busting medicines, like tissue plasminogen activator (t-PA), will assist dissolve the clot and fix blood flow to the involved region.
Anti-platelet drugs, like warfarin. A doctor or physician may suggest aspirin if a patient has an increased risk of a heart attack or stroke and a lower risk of bleeding. Current approaches do not suggest the regular help of aspirin for the most patient, as was the issue in the past.
Hemorrhagic stroke
Therapy for hemorrhagic strokes concentrates on managing bleeding and decreasing stress in the brain. Therapy procedures contain:
Administering medications to regulate blood pressure and control seizures.
Emergency therapy for brain stem stroke
The immediate therapy of a brain stem stroke relies on:
- The type of stroke
- The severity of the symptoms
- The regions of the brain stem involved
- The first step is normally to stabilize the patient involved, creating sure that they can breathe and bringing any lifesaving measures required
Thrombolysis
If a brain stem stroke is induced by a blood clot, then medicine can be provided that can break down the clot and permit blood to flow generally via the blood vessel again. This method is called thrombolysis and should be distributed within a few hours of symptoms beginning to show.
Acute endovascular therapy
In some circumstances, the doctor or physician may select to apply for the clot-dissolving medicine straight to the blood clot to aid removal. This is accomplished by inserting a catheter into the involved patient’s groin and operating it up to the involved blood vessel supplying the involved brain stem region.
Other instruments, like balloons or stents, can be used to open up constricted blood vessels and enhance blood flow.
Hemorrhagic brain stem stroke treatment
If the stroke evolves into hemorrhagic, then hospital treatment will aim to control the bleeding and decrease any stress on the brain. This normally contains a mixed therapy method, involving surgery and drugs such as:
Coil embolization is a surgical technique that allows the formation of a blood clot in the weakened vessel. The clot will decrease bleeding and control the blood vessel from breaking open too.
Once bleeding in the brain is under management, doctors or physician may conduct surgical methods to fix the broken blood vessel to control it from hemorrhaging again.
Breathing assistance and other measures
After a brain stem stroke, the patient involved may require assistance with breathing. This may include the insertion of a line down a patient’s windpipe to provide air to the lungs or simply a mask that provides air via the nostrils.
Swallowing and further involuntary functions might be involved by the stroke. For instance, the involved patient may be at higher risk of aspiration pneumonia, which is when fluids or solid particles, like food, go into the windpipe or lungs.
Brain stem stroke rehabilitation and aftercare
Following a brain stem stroke, a patient’s physical capabilities are frequently restricted. The quantity to which the patient is involved can differ from a feeling of numbness or weakness to full paralysis of the body (locked-in syndrome). This can show several potential problems involving:
Deep vein thrombosis, potentially harmful blood clots which are more probable to form if the patient is not moving about for long periods
Unhealthy nutrition, because of problem swallowing or chewing
Aspiration pneumonia is a kind of pneumonia induced by food or drinks being accidentally inhaled into the lungs
Skin issues, due to raised stress on the skin induced by the lack of motion
Falls and further accidents connected to a sudden loss of balance and/or physical deficiency
Breathing issues
Most of these can be controlled with good nursing supervision and the asset of a physical therapist to help with how the issues can be avoided, once the patient is released from the hospital and after perhaps further in- and/or outpatient rehabilitation.
Physical therapy
A physical therapist will assist with addressing the issues generated by a stroke in the brain stem. This contains assisting a patient with:
- Balance
- Gait
- Wheelchair usage, if required
- Eye movement difficulties
Occupational therapy
An occupational therapist will help a patient involved stroke in recover the capability to complete tasks required for living day to day, like:
- Getting dressed
- Washing the body
- Eating
- Getting around
This treatment will frequently affect a patient’s family or the people they are near. An occupational therapist can help with accessing further assets, like a wheelchair or machines that make bringing in and out of a bath more comfortable.
Difficulties in speaking and swallowing after a stroke
A patient may have a problem speaking or swallowing after a stroke in the brain stem. An ineptitude to speak can generate frustration and make it hard for the involved patient to communicate their requirements. An incapacity to swallow can lead to problems eating and bringing the right nutrition, as well as some further diseases like aspiration pneumonia.
Speech and language therapists will be capable to assist a patient to overcome or deal best with these problems, which can enhance over time.
Emotional difficulties after stroke
After a stroke, many patients feel emotional issues, feel afraid of living with future difficulties or long-term disability, and may sense a loss of confidence in performing everyday tasks or social movements.
These problems may contain:
- Low, depressed mood and mood swings
- Clinical depression
- Crying or laughing easily, occasionally with no apparent cause or in socially unacceptable conditions
- Feeling angry a lot more than earlier
- The feeling that the patient’s personality has altered
- Creating generalized anxiety condition
- Developing post-traumatic stress condition
- Denial about the effects of the stroke and requiring assistance in day-to-day tasks
Emotional problems tend to enhance with time and therapy, and there are various therapy choices available to assist and help someone experiencing them, involving:
- Support groups like those registered with the National Stroke Association
- Talking therapies, like psychotherapy
- Medications, like antidepressants
Physiotherapy treatment in Brainstem Stroke
The purposes of rehabilitation are to optimize how the patient works after a stroke and the level of independence and to gain the best feasible quality of life.
Breathing exercise
Breathing exercises are a state of activity that can be used for a combination of health-related causes. eg. to improve the respiratory system by enhancing ventilation, creating breathing more efficient, boosting respiratory muscles, and for stress decrease.
Wrong breathing can disturb the oxygen and carbon dioxide interaction and contribute to panic attacks, anxiety, fatigue, and further physical and emotional troubles.
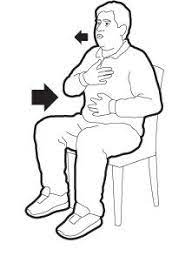
Deep Breathing
Deep breathing exercise assists to reduce shortness of breath by controlling air from obtaining trapped in the lungs and assists inhalation of more fresh air to the bottom of the lungs. It may assist the client to sense more calm and centered.
While standing or sitting, pull your elbows back just to permit your chest to inflate.
Bring a deep inhalation via the nose.
Keep your breath for a count of 5.
Gradually dismiss your breath by exhaling via the nose
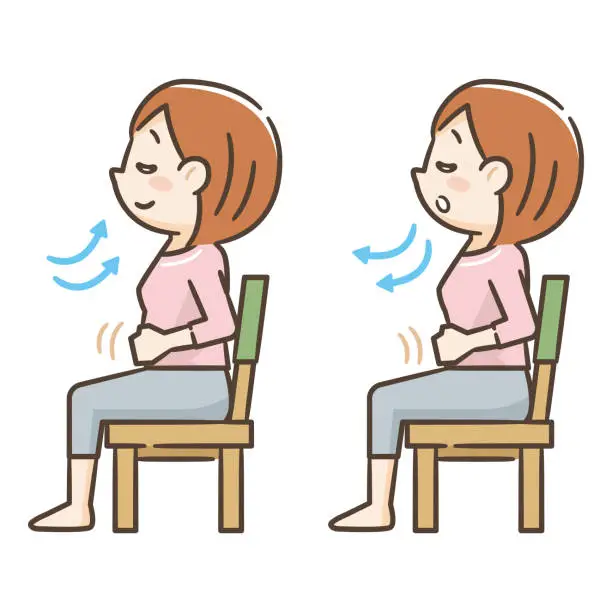
Diaphragmatic Breathing
Diaphragmatic breathing is a kind of breathing exercise that assists boost the diaphragm, an essential muscle that assists with breathing, as it means 80% of breathing. Diaphragmatic activities assist to make a patient feel calm and rested.
This breathing activity is also occasionally known as belly breathing or abdominal breathing.
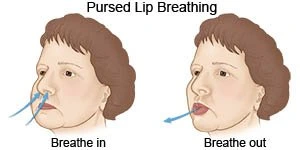
Pursed Lips Breathing
Pursed-lip breathing is a breathing process that consists of exhaling via tightly squeezed (pursed) lips and inhaling via the nose with the mouth closed. It is a simple breathing method that assists with making deep breaths gradually and more intentionally.
This method has been seen to help a patient who has anxiety-associated lung diseases eg. emphysema, and chronic obstructive pulmonary disease – COPD.
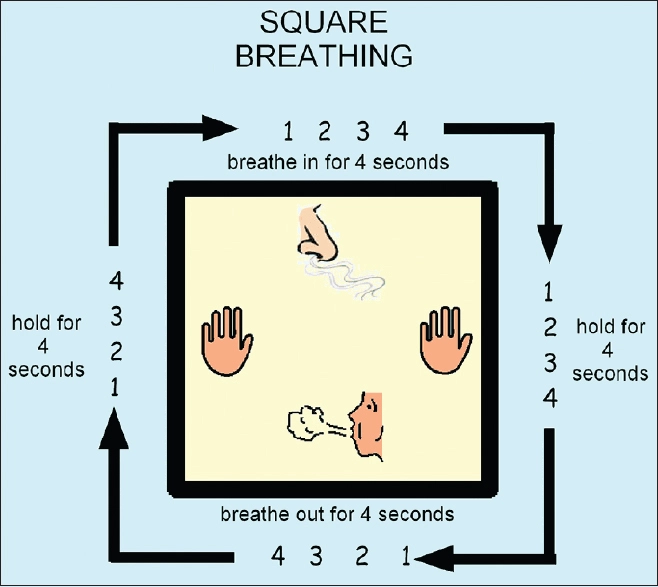
Box Breathing
Box breathing can be useful for relaxation. Box breathing is a breathing activity to help persons with stress control and can be executed before, during, and/or after stressful incidents. Box breathing includes imagining a journey near the four sides of a square, staying while crossing horizontally, and breathing in while crossing up the square and out while crossing down it. This activity can be executed in many atmospheres, not needing a calm atmosphere to be useful.
Step One: Breath in via the nose for a count of 4.
Step Two: Maintain your breath for a count of 4.
Step Three: Breath release for a count of 4.
Step Four: Maintain your breath for a count of 4.
Repeat
Pranayama
Pranayama is utilized as a technical word in yoga, it is frequently translated more precisely as “breath control”.
Traditional pranayama was established on different parts of physical and spiritual well-being, rehearsed from a seated position. In the current world where everyone is at their desks for long durations moving with pranayama in movement is a good option, and has changed for this.

Mindful Breathing
Mindfulness meditation includes concentrating on your breathing and bringing awareness to the present without permitting your mind to drift off to the past or future.
A relaxing focus is selected, involving a sound (“om”), positive phrase (“peace”), or word (“breathe in quiet, breathe out stress”) to replicate silently as the consumer inhales or exhales.
The mind and body then allow go and calm.
When the client sees the mind has drifted, they bring a deep breath and slightly return awareness to the present.
Range of Motion Exercises
After lower extremity damage, you may require to work on recovering and supporting a normal range of motion (ROM) in your joints. Frequently after surgery, swelling may restrict the joint range of motion – ROM.
Range of motion may also be restricted by tight muscles or structures that appear after a period of immobilization following damage or surgery. Working to recover that movement may be a region of your gait training activity schedule.
Exercises to enhance lower extremity range of motion – ROM may contain:
- Ankle pumps
- Calf stretch with a towel
- Heel slides to enhance knee range of motion – ROM
- Hamstring stretches
- Hip rotation stretches
Sustaining full range of motion – ROM, as you learn to walk again, can assist your joints to move willingly as you step and take weight onto per leg.
Lower Extremity Strengthening
Strengthening exercises may be integrated into your gait training activity schedule. If you have weakness in your knees, hips, or ankles, this may control you from walking safely. Activities for your lower extremities may contain:
- Straight leg raises
- Quad sets and short arc quads
- Ankle strengthening with resistance bands
- Mini squats
- Step-ups
Activities should be done gradually, and it is suggested that you use light resistance and high repeats for lower extremity gait training activities. Because walking is a low-resistance, high-repetition exercise. Your activities should simulate that kind of motion.
Balance training
Balance training schedules purpose to:
- Strengthen balance control in daily activities conducted to enhance fall-related self-efficacy, decreased fear of falling, and raised walking speed
- Enhance physical function
- Enhance the quality of life
Examples of balance exercises contain:
Standing, weight on one leg and lifting the further leg to the side or behind.

Placing heel right in front of your toe eg. tandem stance

Standing awake and sitting down from a chair without utilizing hands

Walking while alternating knee raises per step
Accomplishing tai chi or yoga. Tai chi is a time-honored martial art that includes rhythmic motions, slow, involving moving weight, rotation of the trunk, coordination, and an incremental progression to constricting the lower extremity stance. It has achieved distinction as a good activity option for seniors. Analyses have indicated that tai chi enhances postural equilibrium more so than other activities. It also shows multiple musculoskeletal and cardiopulmonary advantages.
Using tools, such as a Bosu, (or different balance board) which has an inflatable dome on top of a circular medium, which challenges the equilibrium

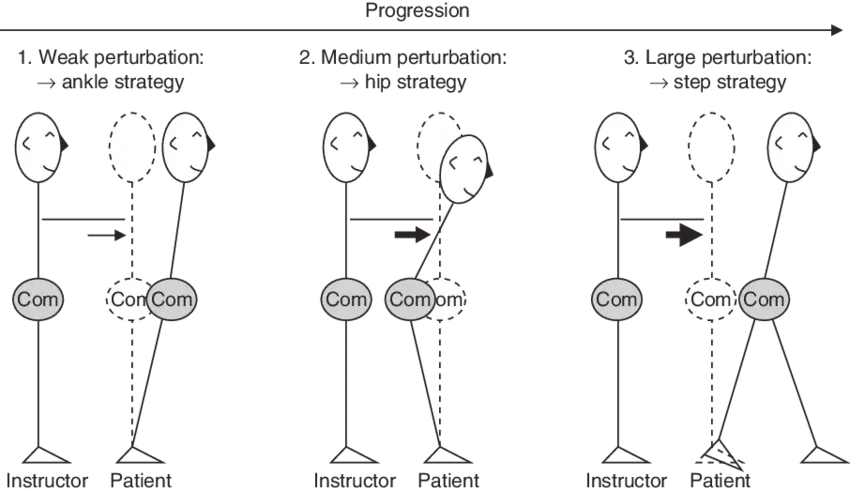
Perturbation-based balance activity (an intervention including reprised postural perturbations purpose to enhance control of rapid balance reactions). This training has been verified to enhance reactive balance control in post-stroke people during the sub-acute stage.
Over time, you can make these movements harder by:
- Maintaining the position for a longer quantity of time
- Walking tandem stance with help then without (visit Otago)
- Closing eyes
- Letting go of chair or further asset
Stepping Over Obstacles
One way to enhance your gait is to accentuate the movements that happen in your legs while walking. One manner to accomplish that repetitively is to complete stepping activities over obstacles or small hurdles. This causes you to bend your hip joints up high and flex your knee joints up behind you when walking.
Obstacle Gait Training
Here is how to conduct obstacle gait activity:
Put up five or six small blocks in a row approximately 15 inches apart. Obstacles can be rolled up athletic hurdles, towels, or small stacks of books.
Stand confronting the obstacles, and step over one with one foot.
Put your further foot following your first foot.
Reprise walking over the blocks with one foot. Then, twist about and step over the blocks conducting with your further foot first.
When this evolves easily, step over the first block, then step over the following block in the row. Be certain to raise your knee high and raise your foot and ankle towards your buttocks when bringing steps.
Reprise walking over the blocks for 10 repeats.

Side-Stepping Gait Exercises
Once obstacle stepping has evolved comfortably when stepping ahead over the hurdles, you can attempt stepping over sidewards. This alteration to your normal ahead gait can assist you to move in various directions while walking.
Here’s how to conduct side-stepping gait activities:
Stand with your barriers to your side
Step one foot sideward over the first barrier. Be foolproof to lift your knee joints high.
When putting your foot down on the further side of the barrier, be certain to leave sufficient room for your second foot to land.
Raise your second foot, high knee.
Put your second foot following your first foot. Reprise over all the obstacles.

Precautions
Since barrier stepping needs you to bring big steps with high knees, it needs you to expend additional time standing on one leg as you step. This can assist to enhance gait, but it may also make instability as you step. So, be confident you are secure while conducting this activity; a person should be with you to assist to guide you as you walk.
If you are uncertain of your capability to do this gait training activity, see your local PT. They will be capable to assist.
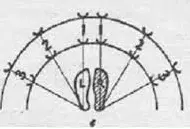
Target Stepping
To enhance lower extremity coordination during your gait training activity training, you may wish to conduct target stepping. To accomplish target stepping:
Put four or five targets on the bottom in a semicircle. The marks should be approximately one foot separated. You can utilize small parts of paper or paper plates as marks.
Stand to one side of the marks on the bottom.
Gradually step with one foot to tap a mark.
Return that foot to the beginning position, then reach out similarly to another mark and swab it with your foot.
Reprise tapping per mark with one foot, and then the further. Attempt to softly and gradually land per tap.
This activity allows you to enhance your capability to put your foot precisely where you like it while walking and has the counted use of promoting single-leg standing.
Retro Walking
Backward walking may be suggested by your physical therapist to assist to enhance your gait. The advantages of backward walking may contain:
- Improved hamstring flexibility
- Improved quadriceps activation
- Improved balance
- Improved coordination
- Improved walking speed
- Improved step length and stride length
Backward walking appears to reset your neuromuscular system, challenging your lower extremity muscles and joints in precise manners that may enhance your gait.
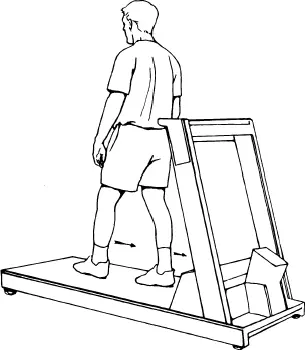
The securest way to execute retro walking into your gait training activity schedule is with a treadmill:
To begin, stand on the treadmill confronting backward.
Begin the belt moving at the gradual speed feasible.
On the treadmill, get one foot backward and put your toe down.
Move onto your midfoot and then to your heel.
Retro walking should be done gradually and in management. Be sure you stay secure while retro walking by utilizing the security emergency stop part on the treadmill.
Exercise for swallowing difficulty
Shaker Exercise
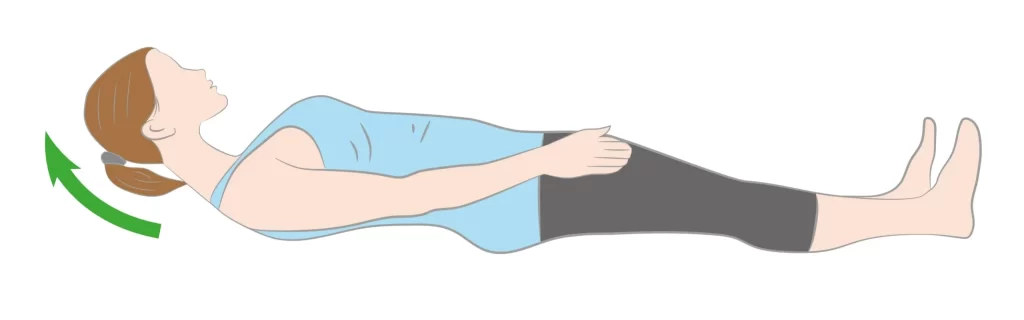
Purpose: To boost muscles and enhance your capability to swallow
First, lie flat on your back in a supine position and lift your head barely off the bottom. Have your head lifted high sufficiently so that your eyes are spot on your toes. Maintain this position for a few seconds and then put your head back down. Reprise this same motion a few more additional times. For best outcomes, accomplish this activity three to six times throughout the day. Over time, you can improve the duration of the head raise and the number of repeats.
Hyoid Lift Maneuver
Purpose: Makes swallowing muscle power and control
Put multiple small parts of paper on a towel in front of you. Subsequently, put a straw in your mouth and stink on the straw, permitting the paper to get reaped up by the tip of the straw. Hold stinking on the straw as you have the straw over to a cup, and prevent stinking to remove the paper from the cup. You should aim to successfully put all of the parts of the paper into the cup. You can begin out with only 3 to 5 pieces of paper and gradually rise to about 10.
Effortful Swallow
Purpose: Enhance the communication and coordination between the various muscles used while swallowing
While dry swallowing, press all of the muscles associated with swallowing as difficult as possible. Reprise this up to 10 times in a single session. You should accomplish 3 sessions of this activity per day to adequately boost your muscles.
Supraglottic Swallow
Purpose: Enhances your capability to swallow food
Bring a deep breath and maintain holding your breath as you put a small bite of the meal in your mouth and swallow. Then, cough to empty any remains of saliva or meals which may have gone down past your vocal lines. Lastly, exhale. During your first few tries at the activity, accomplish not use meals. Once you have adequate training with this activity, you can attempt it with a tiny bite of a meal in your mouth.
Super Supraglottic Swallow Maneuver
Purpose: Enhances your capability to swallow food and boosts swallowing muscles
This activity is the exact as the previous one but is a little more extreme. This time, you should take down while assuming a deep breath and then swallow difficult.
Surgery
Possibilities to manage an ischemic stroke are:
The embolectomy line is passed via blood to remove a clot or produce a drug to break it up
Vertebrobasilar angioplasty and stenting a main artery to the brain is enlarged and a mesh line is left in position to assist to maintain it open
How to Prevent Brainstem Stroke?
An evaluated 80 percent of strokes are preventable. A patient can decrease their risk of stroke by making the subsequent lifestyle modifications:
- observing lipid and cholesterol levels
- regulating blood pressure with drug and behavioral modifications
- controlling medical needs, like diabetes
- quitting smoking
- eating low-fat, low-sodium diets
- confirming that the diet includes an abundance of fresh fruits and vegetables
- hiring in moderate-intensity aerobic activity for at least 150 minutes a week or vigorous-intensity aerobic activity for at least 75 minutes a week
Complications of brain stem stroke
A brain stem stroke can induce you to lose your feeling of smell and taste.
Additional rare complications contain coma and locked-in syndrome. Locked-in syndrome is a disease in which your entire body, except for the eye muscles, is paralyzed. Patients can think and communicate via eye motions, like blinking.
Recovery
A brain stem stroke can outcome in extreme long-term difficulties. Drug and behavioral modifications can assist to decrease the risk of future strokes.
Physical therapy can enhance coordination, and muscle strength, and ultimately allow a patient to recover lost motor skills.
Occupational and speech and language treatment can assist patients to enhance their cognitive abilities, like problem-solving, memory, and judgment.
Some patients who have had a brain stem stroke and have extreme disabilities may need psychological counseling to assist them to adjust.
FAQ
What is the survival pace for brain stem stroke?
It is hard to give an exact figure for the survival rate of brain stem stroke as a full. This is because it relies so largely on where in the brainstem the stroke takes location, whether the stroke is hemorrhagic or ischemic, and several further factors.
For instance, in an analysis of people at a New England medical center, the prevalence involved by posterior circulation stroke survived. Nevertheless, another analysis displays that an ischemic stroke in the basilar artery, which provides the pons region of the brain stem, takes a high mortality risk.
Can someone recover from a brain stem stroke?
The brain stem is simply a one-half inch in diameter. Due to its tiny size, most brain stem strokes are fairly small, but the results can be effective. Fortunately, intensive rehabilitation frequently assists people to regain function.
How long can you survive after a brain stem stroke?
Of the stroke persons, about 30% die within the first year, 20% die in the early era, and about one-third of the survivors evolve dependent on others for their daily living exercises
How serious is a brainstem stroke?
A brain stem stroke is a life-threatening medical crisis. If you have symptoms that suggest a stroke, your doctor or physician will probably order imaging tests like a CT scan, MRI scan, Doppler ultrasound, or angiogram. Heart function testing may contain an electrocardiogram and echocardiogram.
Can a person become normal after a brain stroke?
Healing time after a stroke varies for everyone and can bring weeks, months, or even years. Some patients heal completely, but further have long-term or lifelong disabilities.