Popliteal Artery Entrapment Syndrome
What is a Popliteal Artery Entrapment Syndrome?
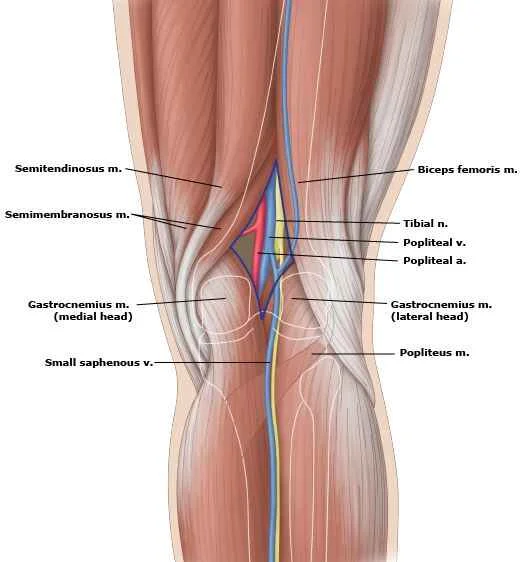
In certain young athletes, leg discomfort might be caused by a rare disorder called popliteal artery entrapment syndrome (PAES). Your popliteal artery, which passes through and behind your knee, is squeezed by your calf muscles.
This reduces the amount of blood that gets to your lower leg during exercise. Four to six weeks are needed for recovery after surgery, which has a high success rate.
Introduction
The major artery behind the knee can become entrapped in the popliteal artery, a rare disease known as PAES. The popliteal artery is the name of that artery. The calf muscle is either enlarged or positioned incorrectly in this disease. The artery is compressed by the muscle. Blood flow to the lower leg and foot is impeded when an artery becomes trapped. Athletes are especially likely to experience popliteal artery entrapment syndrome.
According to Stuart’s 1879 description, popliteal artery entrapment syndrome (PAES) is a rare vascular condition that poses a threat to limbs and affects 0.17–3.5% of the US general population.
An abnormal connection between the popliteal artery and the surrounding popliteal fossa myofascial structures is the primary cause of this developmental defect in the embryo. It’s surprising to learn that young, masculine, active individuals without a history of cardiovascular risk factors are primarily affected by PAES.
Furthermore, constant pain in the calves and feet that typically happens after exercise and goes away at rest is the main complaint made by people with PAES. Additionally, advances in radiological imaging have improved sensitivity and allowed for better delineation when it comes to identifying PAES. It has been reported that one of the most effective diagnostic methods for PAES is to combine magnetic resonance imaging (MRI) and arteriography.
In addition, surgical exploration with the addition of fasciotomy, myotomy, or popliteal artery release through sectioning fibrous bands is typically part of the management of uncomplicated PAES. Similar to how popliteal artery thrombosis (PAT), distal arterial thromboembolism (DAT), and popliteal artery stenosis (PAS) can all result from untreated PAES.
The underlying pathophysiology of PAES is covered in the current article, along with the importance of a thorough history and physical examination in assisting with the diagnosis of PAES and outlining the details needed for determining high-risk patients who require immediate surgical intervention.
What is Popliteal Artery Entrapment Syndrome (PAES)?
A rare vascular condition called popliteal artery entrapment syndrome (PAES) affects the legs of some young athletes. The popliteal artery, which is the main artery that connects your thigh to your calf, is compressed by the muscle behind your knee when you have this syndrome.
Compression is caused by where your gastrocnemius muscle attaches to your thigh bone. Your gastrocnemius muscle compresses your artery when it contracts during plantar flexion, the downward motion of the foot.
Arterial spasms during exercise are caused by repetitive compression. This decreases blood flow. This decrease in blood flow causes lactic acid and carbon dioxide to accumulate in your muscles and nerves, causing your calf and foot to feel heavy, achy, exhausted, and occasionally numb.
Usually, three to five minutes after the exercise is stopped, the symptoms get better. The spasm tends to happen more quickly and last longer if treatment is not received. A shorter distance causes symptoms to appear, and recovery takes longer.
Why does Popliteal Artery Entrapment Syndrome occur?
Individuals given PAES from birth have a modified popliteal artery path. During fetal development, when limbs mature, the aberrant transit of the calf muscle around the vascular bundle is thought to be the key event that leads to PAES.
When many young people participate in sports and weight resistance training, such as PAES is not uncommon to develop later in their teens and 20s; the condition is exacerbated by the expansion of the calf muscles. Moreover, men are more likely to experience this issue than women. This might be caused by the sudden increases in muscular mass that accompany male puberty.
Who does Popliteal Artery Entrapment Syndrome affect?
In athletes, especially those who participate in running-related activities and sports, PAES most frequently affects individuals between the ages of 15 and 25. These involve:
- Track.
- Cross country.
- Soccer.
- Lacrosse.
- Field hockey.
How common is Popliteal Artery Entrapment Syndrome?
Less than 1% of people are thought to have PAES. Determining the exact population with this condition is challenging.
Do any other medical conditions resemble the symptoms of Popliteal Artery Entrapment Syndrome?
Another more prevalent condition that is brought on by exercise is called chronic exertional compartment syndrome (CECS), which affects the muscles and nerves. It results in soreness, edema, and occasionally paralysis in the afflicted limbs. Though it can affect anyone, young adult runners and athletes who engage in repetitive impact sports are more likely to develop the condition.
Chronic exertional compartment syndrome is a condition that some people with popliteal artery entrapment syndrome may also have. Approximately 5% of patients who do not respond to PAES treatment may also have CECS. It is feasible to have both of these circumstances at once.
Popliteal artery entrapment syndrome (PAES) vs. chronic exertional compartment syndrome (CECS)
Your healthcare practitioner will take your leg blood pressure when you’re at rest and look for a decline while you exercise to check for PAES. They will take a reading in each of your leg’s four compartments before and after the activity to check for CECS. With CECS, there is an unusual increase in the pressure inside your calf compartments.
What are the causes of Popliteal Artery Entrapment Syndrome?
The development of PAES has been linked to both acquired and congenital mechanisms. A comprehensive comprehension of the several phases of human embryonic development has effectively elucidated the exact cause of congenital PAES.
The popliteal artery and the gastrocnemius muscle’s medial head mature at about the same period. A major role in the formation of the popliteal artery comes from both the femoral and sciatic arteries. It starts at the proximal extension of the femoral artery and the distal extension of the sciatic artery. Furthermore, the sciatic artery has a role in the tibial arteries’ development. The femoral artery takes over as the primary source of contribution to the growth of the popliteal artery when the sciatic artery recedes with time.
The congenital PAES is largely influenced by the plantaris muscle embryological stages. Plantar flexion of the ankle joint is facilitated by the plantaris muscle, which is an important part of the superficial group of the posterior crural muscular tissues. Though nearly gone this muscle is thought to function in conjunction with the gastrocnemius. Moreover, it has also been reported to be abnormal in roughly 10% of the cases. This muscle can trap the popliteal artery if it develops abnormally, which would cause claudication signs and symptoms.
In addition, different abnormalities in the popliteal artery, popliteus muscles, and medial head of the gastrocnemius (MHG) determine the different kinds of PAES. Moreover, a muscle’s misalignment concerning surrounding arteries may arise from the abnormal migration of the medial head during embryonic development.
Unexpectedly, the majority of those born with this congenital defect do not exhibit any symptoms, indicating that the sickness is likely to progress through a complex process. The condition is inherited, but it manifests later.
This is probably because the gastrocnemius muscle is used differently during exercises like jogging or marching, which leads to muscle hypertrophy and external compression, affecting the popliteal artery by the medial head.
What are the epidemiology of popliteal artery entrapment syndrome?
The development of PAES, an unusual anomaly, has increased over the last few decades, even though it is still a major source of vascular impairment. According to a recent case report on this particular clinical entity, Wady et al. found that the general population’s total incidence of PAES ranges from 3.5% to 0.17%.
Furthermore, men represent 85% of those afflicted by this ailment, and young athletes in their third decade of life account for nearly 60% of cases. Furthermore, the condition presents as bilateral symptoms in roughly 30% of cases.
What is the pathophysiology of popliteal artery entrapment syndrome?
Fewer patients have been reported to have acquired (fibrous band) causes of PAES, although the majority of cases are often caused by embryological abnormalities. The relationship between the popliteal artery and the medial head of the gastrocnemius muscle further divides the PAES into six categories.
- Type I: an abnormal popliteal artery path around a typically positioned MHG.
- Type II: The popliteal artery moves medially and inferiorly as a result of MHG’s aberrant and more laterally positioned attachment to the thigh.
- Type III: The popliteal artery is surrounded by an abnormal fibrous band or auxiliary muscle that originates from the medial or lateral condyle.
- Type IV: The popliteus muscle or fibrous bands obstruct the popliteal artery, which is situated in the fossa in its primitive deep or axial position.
- Type V: the popliteal artery and vein become trapped as a result of any of the previously listed reasons.
- Type VI: The popliteal artery and vein are functionally compressed as a result of the hypertrophy of the muscles.
Another subtype of the condition unrelated to hereditary anatomic defects is described by the functional PAES (Type VI or F). It has been suggested that recurrent microtrauma causes the smooth muscles to be damaged, connective tissue to proliferate, the internal elastic lamina to be destroyed, and scarring and fibrosis to develop. The injury that follows causes embolization, aneurysmal degeneration, and thrombosis.
Heidelberg et al. also proposed a simpler and more useful classification scheme for the PAES. The PAES is divided into the following three primary categories based on this classification:
- Type 1: The popliteal artery is where the issue is located.
- Type 2: The insertion of the muscle is not normal.
- Type 3: There are the two prerequisites listed above.
History and Physical
Since patients with PAES may experience severe physical disability, a high level of clinical suspicion is necessary. The symptoms are moderate at first and typically appear in the second or third decade of life. Usually, younger athletes without a history of cardiovascular risk factors have been the impacted patients. Patients usually complain of leg and foot claudication, which can be quite severe and incapacitating.
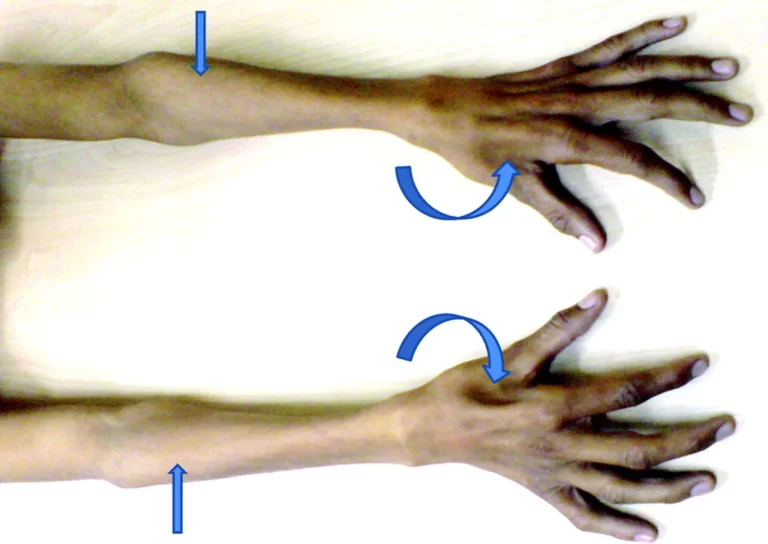
Furthermore, the patient may experience pallor, discoloration, numbness in the lower extremities, paresthesia, and coldness. Furthermore, the physical examinations typically show calf muscle enlargement. Additionally, the ankle-brachial index (ABI) will tilt towards the lower limit as the disease progresses, and the dorsiflexion/plantar flexion of the foot may elicit reduced, uneven, or even missing pulses. According to research by Tercan et al., PAES is characterized by the absence of meal pulses during active plantar flexion and passive dorsiflexion of the foot.
Evaluation
The correct interpretation of both clinical and radiological elements of this uncommon clinical entity is necessary for the diagnosis of PAES, which presents a significant clinical challenge. When it comes to radiology, a combination of tests that describe not only the popliteal artery’s functional and anatomical status but also the structural characteristics of the popliteal fossa is preferred to attain a higher sensitivity in detecting PAES.Willimas et al. found that a combination of duplex ultrasonography (DU) and magnetic resonance imaging (MRI) is significantly more effective in detecting PAES in a recent study investigating the optimal diagnostic modality for the condition.
Furthermore, provocative maneuvers (positioning the leg or foot in neutral first, then in resisted plantar flexion) during duplex arterial ultrasonography (DAU) offer a rapid, low-cost, and non-invasive initial screening examination. Prominent collaterals in the fossa or findings of vascular compromise point to PAES as the cause of the condition.
Furthermore, the angiography can be carried out using provocative maneuvers. Typically, it shows a distal popliteal artery aneurysm, post-stenotic dilatation of the proximal popliteal artery, and a medially deviated proximal popliteal artery. Provocative testing is not possible with computed tomography (CT) angiography or magnetic resonance angiography (MRA), but these tests can confirm the diagnosis when the artery is obstructed.
What is a syndrome of popliteal artery entrapment syndrome?
The primary sign of popliteal artery entrapment syndrome, or PAES, is lower leg pain or cramping in the back. The term “calf” refers to the rear of the lower leg. Exercise causes the ache, which goes away when you rest. Other symptoms may involve:
- Cold feet following physical activity.
- In your calf, tingling or burning.
- Numbness around the calf.
You may have the following conditions if the calf muscle also traps the popliteal vein, a neighboring vein:
- Feeling as though my leg is heavy.
- Cramps in the lower leg during the night.
- Swelling around the calf.
- Skin color variations near the calf muscle.
- A lower limb blood clot is known as deep vein thrombosis.
Young, generally healthy adults under 40 are usually affected.
What causes popliteal artery entrapment syndrome?
An asymmetrical calf muscle, typically the gastrocnemius muscle, is the source of popliteal artery entrapment syndrome.
Either from birth or later in life, the sickness may manifest itself. The baby’s calf muscle or surrounding artery originates in the incorrect location during pregnancy when it is present at birth. Later-life patients with the disease have larger-than-normal calves.
The major artery behind the knee is pressed upon by the alterations in the calf muscle. Blood flow to the lower leg is decreased as a result. During periods of physical activity, the lower leg’s back experiences pain and cramping due to insufficient blood supply.
The two primary kinds of compression are as follows:
- Anatomic compression: About 10% of cases involve this kind of compression, which appears to be more prevalent in individuals who were assigned male at birth. About 70% of cases only involve one leg.
- Non-anatomic compression, functional or physiologic compression: People who are assigned as female at birth are more likely to experience this kind of compression. More than 90% of the time, it affects both legs.
Anatomic compression
This occurs as a result of a segment of your gastrocnemius muscle passing over or through an artery. An artery can be harmed by a tendinous band in your muscle. This results in:
- An ulcer or sore in your artery.
- Accumulation of a clot.
- your artery or arteries downstream may eventually get blocked or shut.
There are four possible ways to locate the muscle concerning your artery.
Non-anatomic compression, functional or physiologic compression
Though they usually insert higher up the thigh bone or on the inside notch at the knee, your muscles are all in their normal locations. This compresses your muscle against your artery by pulling it inward through plantar flexion.
The popliteus muscle, which is situated beneath your artery, serves as an additional point of compression. Researchers have not found any link between physiologic compression and artery damage.
How is popliteal artery entrapment syndrome diagnosed?
The most qualified medical professional to diagnose PAES is a vascular specialist. They will perform a physical examination, which will include monitoring your popliteal artery and your foot pulse. When you push your foot up and down against resistance, they might also watch how your pulse changes.
If popliteal artery entrapment syndrome is present, your doctor:
- May detect your heartbeats when you’re asleep.
- May have trouble feeling your pulses when you exercise flex or stretch your foot.
Radiographic features
Ultrasound
It might demonstrate vascular compression brought on by dorsiflexion and plantar flexion. Doppler can show a rise in the maximum speed.
CT Scan
Diastasis between the popliteal artery and vein, an insertion anomaly, and an arterial deviation can all be detected with CT angiography. Axial images are the most effective means of evaluating aberrant muscle and fibrous attachments, which might vary in nearly every situation.
MRI
The most useful imaging modality for identifying the underlying anatomic kind of entrapment—which informs surgical management—is magnetic resonance imaging (MRI). The popliteal artery may be compressed due to a medial slip of the gastrocnemius’s medial head.
Angiography (DSA)
When the ankle is planted, lower limb angiography typically shows medial deviation or compression of the popliteal artery. The acute presentation demonstrates thrombus-induced artery blockage. Collateral vessels are typically found. A vessel’s even the slightest abnormality may point to some degree of entrapment.
Popliteal artery entrapment syndrome: how is it tested?
Diagnostic tests measure blood flow in your leg, knee, and foot. Imaging can demonstrate:
- Normal artery.
- Your artery is becoming ulcerated.
- Blood clots.
- An artery aneurysm is defined as a blood vessel dilatation that is greater than 50% of its normal size.
- Muscle compressing your artery.
Tests may involve:
- Ankle-brachial index with exercise: The blood pressure in your arms and legs is measured both before and after exercise in this test. Your blood pressure normally rises with exercise and is the same in your legs and arms. Leg blood pressure after exercise decreases to less than 90% of arm blood pressure when running causing an artery spasm.
- Duplex ultrasound of the popliteal artery with plantar flexion: Using sound waves, this test measures blood flow by imaging your artery. With plantar flexion and at rest, it enables your healthcare provider to examine your leg arteries and detect any muscle compression.
- Computed tomographic angiography (CTA) with plantar flexion: With plantar flexion and rest, the leg arteries are examined using dye in this particular type of CT scan to detect muscle compression.
- Magnetic resonance angiography (MRA) with plantar flexion: This test looks at your leg arteries at rest and plantar flexion to detect muscle compression using a magnetic field and radio wave pulses.
What does PAES feel like?
During exercise, you may experience the following symptoms of popliteal artery entrapment syndrome in your foot or calf:
- Aching pain.
- Tiredness.
- Heaviness.
- Cramping.
- Numbness.
- Burning.
After three to five minutes of rest, most symptoms go away. Without treatment, the symptoms usually become more localized and take longer to disappear over time.
What are the risk factors of popliteal artery entrapment syndrome?
PAES, or popliteal artery entrapment syndrome, is rare. The following factors raise the condition’s risk.
- Younger age: Those in their late teens or early 20s are more likely to have the illness. Diagnoses for those over 40 are uncommon.
- Being male: Although everyone can get PAES, young men are far more likely to experience it.
- Strenuous athletic activity: Athletes, cyclists, and runners who use high-intensity circuit training or weight training regimens to gain muscle quickly run the most danger.
What is a complication of popliteal artery entrapment syndrome?
The popliteal artery may narrow as a result of sustained pressure. It’s known as artery stenosis. Walking is a mild activity that might result in soreness and cramping.
The muscles and nerves in the leg could sustain injury in extreme circumstances or if the condition is undiagnosed. Lower limb blood clots can happen. It’s important to have an artery ballooning or bulging examined if older athletes exhibit signs of popliteal artery entrapment syndrome. We refer to this as a popliteal aneurysm. Older males tend to have it.
Due to the potentially fatal nature of PAES, prompt clinical diagnosis and intervention are necessary. PAES can cause the following if it is left untreated:
- Popliteal artery stenosis (PAS).
- Popliteal artery thrombosis (PAT).
- Distal arterial thromboembolism (DAT).
- Limb amputation.
How is PAES treated?
A small portion of your gastrocnemius and popliteus muscles may be surgically removed by your healthcare provider. Your artery will no longer be compressed, restoring normal blood flow to your leg.
An hour is needed for the popliteal artery entrapment syndrome procedure. You will be given general anesthesia to keep you unconscious during the procedure.
When anatomic popliteal entrapment progresses and the popliteal artery becomes damaged and blocked, your surgeon may need to perform a bypass around the blocked section of the artery to restore blood flow.
Popliteal artery entrapment syndrome is best treated surgically because most patients have excellent outcomes. After the procedure, the symptoms of over 90% of patients significantly improve.
For the functional form of PAES, injections of botulinum toxin A are the only non-surgical treatment available.
Your provider injects Dysport® or Botox® into the muscle causing the compression under the guidance of a CT scan or ultrasound. To cause the symptomatic muscle to shrink permanently, this momentarily paralyzes it.
But this is only a three- to six-month-long effect. The symptoms will return if the muscle doesn’t shrink. Less than 60% of patients report success with this one year into treatment.
What is the treatment of popliteal artery entrapment syndrome?
The PAES is managed differently depending on whether symptoms are present or not. The majority of asymptomatic patients with incidental indications of popliteal artery entrapment never suffer symptoms, therefore therapy is usually expected in these cases. Surgical correction is the preferred course of treatment if, on the other hand, muscle insertion anomalies are the origin of the PAEs, even in a patient exhibiting no symptoms.
Additionally, surgical resection has been the preferred course of treatment for PAES individuals who exhibit symptoms. Surgery with popliteal artery release allows for the definitive reestablishment of normal architecture and often portends great results. The musculotendinous band, also known as the MHG, can be separated using a posterior or medial approach. After that, the patency of the artery can be assessed by palpation to see if a bypass is necessary. Since this is well tolerated and does not cause functional limitations, reconstruction of the nearby muscles is not necessary.
Furthermore, open surgical methods provide the greatest outcomes when addressing PAES and evaluating the artery for possible bypass or repair. Using an autogenous vein via a posterior route or medial bypass to extend farther down the below-knee popliteal artery has been recommended in cases when there is severe arterial wall damage, blockage, or aneurysm development after interposition bypass grafting. For the treatment of Type I and II, a posterior approach would be more appropriate, whereas a medial approach might be better for Type III and IV.
Furthermore, although some have had success with gastrocnemius debulking, the management of functional PAES remains contentious. Furthermore, yearly surveillance utilizing arterial duplex imaging is carried out following surgery at 1, 3, 6, and 12 months.
Can stents treat popliteal artery entrapment syndrome?
When treating vascular illness brought on by atherosclerosis, metallic stents are frequently utilized (hardening of the arteries). Patients with PAES typically have normal arteries, and stent implantation is neither successful nor long-lasting. Stent implantation can, in fact, considerably impede healing, therefore it’s best to avoid it.
What is the duration of recovery following this treatment?
Following surgery, recovery from popliteal artery entrapment syndrome takes four to six months. After your procedure, you will have to spend the night in the hospital. To aid in your recovery, you may then participate in physical therapy (which includes stretches and flexibility exercises) for the first two weeks as an outpatient. You’ll perform strength and conditioning exercises until you’ve fully recovered after two weeks.
How is popliteal artery entrapment syndrome surgically treated?
There are two ways to do surgery to treat aberrant arterial compression. A 4- to 6-inch incision behind the knee may be able to give the required exposure in certain cases of PAES to alleviate the popliteal artery. In other types of PAES, full relief necessitates a 4- to 6-inch incision along the inner side of the leg.
If I have popliteal artery entrapment syndrome, what can I anticipate?
You can reduce your exercise routine if you have functional popliteal entrapment and your leg pain symptoms don’t bother you. Your medical professional can keep an eye on your health.
More than 90% of patients, however, recover from surgery, and it is unlikely that they will experience symptoms once more. After surgery, most athletes resume their regular activities.
Providers advise surgically removing the abnormal muscle slips in cases of anatomic entrapment to stop potential arterial damage.
You may be at risk of experiencing constant pain in your legs when you walk if you wait to seek treatment until anatomic PAES has damaged your popliteal artery. A leg amputation may be required. But this is extremely uncommon.
How long is the usual recovery after surgery?
Most people remain in the hospital for one or two nights. Walking will start in the hospital immediately. Post-discharge physical therapy regimens consisting of stretching and exercise are also implemented for patients.
Is surgery successful for popliteal artery entrapment syndrome?
The great majority of our patients have a quick return to normal leg blood flow following their operation and full recovery. Four to six weeks following surgery, we will use ultrasonography to evaluate the blood supply once more.
When should I see my healthcare provider?
You will require follow-up appointments with your surgeon following surgery:
- In one month.
- In six months.
- In 12 months.
Your office appointments will involve:
- ultrasound of the artery that was repaired.
- Check the blood pressure in your feet.
- You won’t require any more follow-up appointments if your artery has returned to normal unless your symptoms reappear or you require an artery bypass.
Differential Diagnosis
It is more difficult to diagnose this potentially fatal limb-threatening illness since many surgical and non-surgical disorders resemble the PAES. Among the differential diagnoses for the PAES are, but are not restricted to:
- Chronic exertional compartment syndrome.
- Medial tibial stress syndrome.
- Fibular stress fractures.
- Tibial stress fractures.
- Abnormalities of the face.
- Nerve entrapment syndrome.
- Pain from a herniated lumbar disc that was referred.
Prognosis
The PAES’s detection time is the sole factor that determines its prognosis. In general, the prognosis for PAES is favorable provided it is identified and treated early in the disease’s progression.
The patient may suffer from persistent claudication or possibly limb loss if the PAES is discovered after significant arterial damage has already occurred. Nevertheless, even in cases of significant disease, limb loss in PAES patients remains exceedingly rare due to the slow nature of arterial occlusion.
Deterrence and Patient Education
The following actions ought to be covered in the patient education for PAES.
- The patient is required to be informed as much information as possible regarding the cause of the PAES.
- People are required to be informed that the best course of action is early surgical surgery, which is the only method to stop the disease’s progression.
- Patients are required to be informed about the symptoms and indicators of compartment syndrome after surgery.
Summary
There are several symptoms associated with the rare condition known as popliteal artery entrapment syndrome. Based on the imaging results, customizing the examination for diagnosis confirmation and surgical planning is crucial.
To diagnose popliteal artery entrapment syndrome, the aberrant anatomic structures causing the entrapment must be identified in addition to the vascular alterations. Both conventional angiography and sonography can detect artery compression, but they are unable to identify the underlying anatomic abnormalities. The aberrant muscle or fibrous attachment as well as the vascular findings required for diagnosis and surgical planning can be seen using tailored MRI and MR angiograms.
FAQs
How do you fix popliteal entrapment syndrome?
Restoring the calf muscle and freeing the trapped artery requires surgery. Surgery is carried out in a hospital or other medical facility under general anesthesia. When performing surgery, the inner calf is incised either in the rear of the knee or directly below it. By doing this, the calf muscle is released, allowing the artery to expand.
How do you test for popliteal entrapment syndrome?
Magnetic resonance angiography (MRI) and computed tomography (CT) angiography tests can confirm the diagnosis when an artery is occluded, but they do not allow provocative testing.
What does popliteal artery entrapment syndrome feel like?
Exercise-related symptoms are commonly experienced by patients with PAES, and these symptoms can include: Aching discomfort (claudication), numbness, or cramping in one or both calves after intense exercise; these symptoms typically disappear in five to ten minutes.
What happens if the popliteal artery is blocked?
When the popliteal artery, the primary artery supplying the lower body, is compressed by muscles located behind the knee, blood flow to the legs is restricted. Popliteal artery entrapment syndrome is the term used to describe this illness. People with this illness experience pain when walking or when they exercise vigorously.
How long does popliteus take to heal?
In most cases, these wounds heal without any issues or complications.It may take three to sixteen weeks for the patient to fully recover, and following the completion of a functional assessment, they can return to full physical activity without any limitations.
What is the recovery time for popliteal entrapment syndrome?
Following surgery, healing from popliteal artery entrapment syndrome takes four to six months. Following your procedure, you will need to spend the night in the hospital. To aid in your recovery, you may then participate in physical therapy (which includes stretches and flexibility exercises) for the first two weeks as an outpatient.
What are the symptoms of popliteal artery disease?
Should the calf muscle also ensnarl the adjacent vein, known as the popliteal vein, you could have:
A heavy feeling in the leg.
Lower leg cramping at night.
Swelling in the calf area.
Changes in skin pigmentation around the calf muscle.
Lower leg blood clot caused by deep vein thrombosis.
What are the different types of popliteal entrapment?
Types 1 and 2 feature medial deviation of the popliteal artery relative to the medial head of the gastrocnemius muscle. Types 3 and 4 are caused by compression of a normal popliteal artery by either fibrous bands from the popliteus muscle or slips of the gastrocnemius. Type 5 refers to an aberrant popliteal vein placement.
How do you identify a popliteal artery?
The popliteal arteries are situated behind the knee pit and the knee. The anterior tibial artery and the tibioperoneal (or tibiofibular)trunk split the arteries below your knee joint. Your fibula and the rear of your calf receive blood flow from this trunk, which splits into smaller branches.
What is Type 4 popliteal artery entrapment syndrome?
Type IV: This condition arises when the popliteal artery crosses the popliteus muscle. Type V entails compression of both the popliteal vein and artery. Type VI — involves other variations.
What is the most common cause of a popliteal artery injury?
High-energy injuries, such as knee dislocation and complicated tibial plateau fractures or supracondylar femur fractures, are primarily linked to popliteal artery injury. When this limb-threatening injury is diagnosed too late, it is the main cause of amputation.
What is the success rate of popliteal artery entrapment syndrome surgery?
At one and five years, the total rates of primary graft and native popliteal artery patency were 91.9% and 96.3%, respectively. In conclusion, myotomy and selective revascularization are effective short- and long-term treatments for PAES.
Is popliteal artery entrapment serious?
Secondary consequence: Over time, repeated trauma to the artery along its aberrant route may physically harm the arterial wall, leading to a progressive constriction of the artery known as stenosis. In the worst situations, there may be irreversible damage to the leg’s muscles and nerves.
What is a differential diagnosis for popliteal entrapment syndrome?
Varied and nonvascular aetiologies are included in the differential diagnosis. Vascular aetiologies include peripheral arterial disease, cystic adventitial disease, and arterial endofibrosis.
What is the first line of treatment for popliteal entrapment syndrome?
An exact diagnosis requires early diagnosis using a multimodal method that includes angiography, computerized tomography, duplex ultrasonography, and a thorough physical examination and history collection. The surgical restoration of normal anatomy within the popliteal fossa is the preferred course of treatment.
What is the best treatment plan for popliteal artery entrapment syndrome?
Surgery is the only way to release the trapped artery and heal the calf muscle. You are put under general anesthesia and have surgery at a hospital or medical facility. When performing surgery, the inner calf is incised either in the rear of the knee or directly below it. This gives the artery more space by releasing the calf muscle.
How do you test for popliteal entrapment?
For diagnosis, noninvasive imaging methods like magnetic resonance imaging (MRI), magnetic resonance angiogram (MRA), CT, CTA, and DU may be utilized.
References
- “Popliteal Artery Entrapment Syndrome – Symptoms and Causes – Mayo Clinic.” Mayo Clinic, 13 Sept. 2023, www.mayoclinic.org/diseases-conditions/popliteal-artery-entrapment/symptoms-causes/syc-20465211#:~:text=Po.
- Davis, Donald D. “Entrapment of the Popliteal Artery” NCBI Bookshelf: StatPearls, Aug. 28, 2023, www.ncbi.nlm.nih.gov/books/NBK441965.
- Professional, Cleveland Clinic Medical. “PAES, short for popliteal artery entrapment syndrome.” The Cleveland Clinic, my.clevelandclinic.org/health/diseases/popliteal-artery-entrapment-syndrome-paes.
- El-Feky, Mostafa, and Andrew Dixon. “Popliteal Artery Entrapment Syndrome.” Radiopaedia.org, 15 Apr. 2010, https://doi.org/10.53347/rid-9410.
- “Popliteal Artery Entrapment Syndrome (PAES).” Johns Hopkins Medicine, 22 Sept. 2021, www.hopkinsmedicine.org/health/conditions-and-diseases/popliteal-artery-entrapment-syndrome-paes.