Quadriceps Contusion & Physiotherapy management
- A quadriceps contusion happens when someone gets hit very hard in the thigh. The force makes the muscle tear and bleed. It also can tear the sheath that covers the quadriceps muscles.
- A quadriceps contusion is a traumatic blow, a deep bruise to the anterior lateral or medial aspect of the thigh. If the examination confirms an area of swelling and tenderness with (terrible) pain on passive stretch and active contraction, the diagnosis is a Quadriceps contusion with resultant hematoma.
- A contusion is the most common acute thigh injury in contact sports such as football, rugby, and basketball. Contusions are caused by external forces like a direct blow from an opponent’s knee.
- Thus, muscle contusions are classified as acute direct muscle injuries. The most frequently injured muscles are the exposed rectus femoris and the intermediate vastus, lying next to the bone, with limited space for movement when exposed to a direct blunt blow.
- Localized bleeding may increase tissue pressure and tissue damage. The bleeding can be intramuscular or intermuscular. The intramuscular hematoma is more painful and restrictive of range of motion than the intermuscular hematoma.
Anatomy related to Quadriceps contusion
- The Quadriceps femoris muscle is a hip flexor and a knee extensor. It’s located in the anterior compartment of the thigh. This muscle is composed of 4 sub-components:
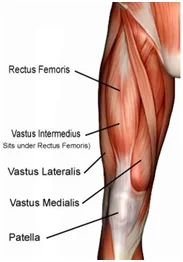
- Rectus femoris
- Vastus medialis
- Vastus lateralis
- Vastus intermedius
- Origin: Rectus femoris: anterior inferior iliac spine, the superior margin of the acetabulum of the hip bone
- Vastus medialis: intertrochanteric line of femur
- Vastus lateralis: Linea Aspera, greater trochanter of femur
- Vastus intermedius: anterior surface of shaft of the femur
- Insertion: Tuberosity of the tibia (via the patellar ligament) (medial and lateral condyles of femur (vastus medialis and lateralis)
- Innervation: Femoral nerve (L2-L4)
- Actions: Hip joint: Thigh flexion (rectus femoris only), Knee joint: Leg extension.
Pathophysiology of a Quadriceps contusion
- Several physiological responses may occur after a deep thigh contusion including:
- Broken blood vessels resulting in bleeding (hematoma) into the injured area
- Crushed muscle tissue resulting in hip and knee dysfunction
- If there is major untreated and/or unresolved bleeding deep in the muscle tissue, a serious condition known as myositis ossificans can occur.
- Contusion injury can lead to either diffuse or circumscribed bleeding that displaces or compresses muscle fibers causing pain and loss of motion.
- It happens that muscle fibers are torn off by the impact, but typically muscle fibers are not torn by longitudinal distraction. Therefore, contusions are not necessarily accompanied by structural damage to muscle tissue.
- For this reason, athletes, even with more severe contusions, can often continue playing for a long time, whereas even a smaller indirect structural injury forces the player often to stop at once.
Risk factors
- Contact sports and sports that require quick starts, i.e. running races and other track events.
- Warm-up and cool-down habits.
- Off-season/preseason/season training habits.
- Poor muscle conditioning.
- Playing position.
- Level of competition.
- Protective equipment use.
- Playing experience.
- Injury history, especially to the thigh, hip, and/or knee.
- Medical history of any bleeding disorder.
- Age.
- Poor nutrition.
- Smoking history.
- Obesity
Clinical features of a Quadriceps contusion
- A massive blunt force mostly to the anterior or lateral thigh causes a rupture in the muscle fibers.
- In the beginning, there are negligible symptoms, but after 24 hours this will lead to hematoma formation within the muscle causing: pain, swelling, stiffness, and impairment of functional quadriceps excursion.
classification
- Mild : >90 degrees ROM
- Moderate: 45-90 degrees ROM
- Severe : <45 degrees
Presentation of a Quadriceps contusion
- History
- collision or direct blow to the thigh during competition
- Symptoms
- pain
- worsening severity over the first 24-48 hours
- worse with dynamic movements and knee flexion
- Physical examination
- Palpation along with the injured muscle: to localize the pain and exact site of muscle damage and also to determine if there is any associated injury.
- The palpation test involved systematic digital probing from the lateral border of the vastus lateralis to the medial side of the thigh with the patient in long sitting, after which the physiotherapist subjectively noted, then recorded, the muscles injured and the area of injury (distal third, middle third or a proximal third of the thigh).
- Muscle firmness testing was performed with fingertip palpation, with the muscle firmness at the site of the injury compared with the firmness of the same site on the uninjured leg, and rated on an 11-point scale from -5 (comparatively decreased muscle firmness) to +5 (comparatively increased muscle firmness).
- A zero-rating was applied if the muscle firmness of the injury site was similar to the muscle firmness of the non-injured thigh
- Circumference measures were taken at the suprapatellar border, and at 10 and 20 centimeters proximal to this site on both thighs, using a purpose-made device that was designed to ensure that the distances above the suprapatellar border were constant for all subjects.
- The bottom of the Velcro strap was positioned in line with the suprapatellar border and the tape measures applied such that they were just in contact with the skin surface of the thigh. Measurements were recorded to the nearest millimeter
- Passive knee range of motion testing was performed with the subject in a prone, with the hip in neutral, and the foot and distal third of the shank over the edge of the plinth to enable positioning of the Baseline digital inclinometer Prior to performing a joint angle measure, the tester passively flexed both knees three times until the available end of the range was reached as determined by the first onset of pain on the injured leg, and restriction on the non-injured leg.
- This was done as a control for any preconditioning effect. The inclinometer was set to zero on the horizontal surface of the plinth and placed on the distal end of the tibia to measure the joint angle as the tester flexed the knee Subsequently, the difference in flexion range between knees and the relative percentage of knee range retained was determined.
- The brush-swipe and tap tests were performed with the patient in long sitting. In the first of these, the examiner was required to stroke the medial side of the patella, proximally towards the hip joint, two or three times followed by a stroke down the lateral side of the patella. A positive test was registered when a visible wave of fluid was evident on the medial side of the knee joint and below the patella border.
- The tap test was performed by applying a slight tap or pressure over the patella. A positive test was present when a large amount of intracapsular swelling produced a floating patella so that, on tapping, a downward movement of the patella could be felt by the tester.
- Strength testing of the quadriceps: that contains resisting knee extension and hip flexion, compared to the uninjured side. This will help in assessing the severity of the injury.
- Measurement of knee flexion is used as a prognostic indicator in quadriceps contusions. Based on this, thigh contusions can be graded into 3 groups that are based on the severity of the injury. distal neurovascular exam to evaluate for thigh compartment syndrome.
Imaging
- Radiographs
- indications
- only necessary acutely in severe injuries with high suspicion of underlying fracture
- findings
- myositis ossificans
- occasionally seen in chronic cases
- MRI
- indications
- concern for extensor mechanism disruption
- best to demonstrate the degree of soft tissue involvement and extensor mechanism integrity
- finding
- will find edema with muscles.
Medical Management of Quadriceps contusion
- NSAIDs can be useful short-term for decreasing pain, but their long-term effect on muscle healing is not known. Long-term use of NSAIDs for contusions is usually not necessary and is discouraged. However, NSAIDs have been promoted for the prevention of myositis ossificans after severe quadriceps contusions.
- Evidence for this use is inferred from studies showing a decrease in heterotopic bone formation after total hip replacement in those patients given indomethacin for at least 7 days. Similar to quadriceps muscle strains, corticosteroids are not recommended in the treatment of contusion injuries.
- After three to four weeks, if the patient still moves with pain and isn’t able to perform a painless, full range of motion, radiographic imaging should be performed. This is to detect whether myositis ossificans is present. Myositis ossificans results in lasting pain and limited knee flexion. Surgical excision is then recommended.
- An MRI should also be considered to check for the presence of intramuscular hematoma or seroma. An MRI can also determine osteomyelitis of the femur. In that case, the solution is a resection of the infected bone and antibiotics.
Physiotherapy management of Quadriceps contusion
- For patients with a quadriceps muscle contusion, there are several treatments from which a physical therapist can choose. The first option is cryokinetics.
- It is a revalidation technique that consists of ice application followed by progressive, active exercises. Once the affected thigh is getting numbed, you can begin by passively stretching the leg. A second aspect of the treatment program can be soft tissue massage around the periphery of the contusion.
- This leads to a better fluid resolution. A third option is electrotherapy in order to reduce the pain. Very important is that the patient avoids activities that excessively load the quadriceps during physiotherapy.
- The principles of treatment for quadriceps contusions are essentially the same as for quadriceps strains, with one major exception. It is recommended the injured leg be placed in a position of flexion for the first 24 h post-injury to limit hematoma formation.
- Practically, this can be done by placing the patient in a hinged knee brace at 120° of knee flexion or using elastic compression wrap to maintain this position of flexion. This needs to be done as soon as possible after the injury.
- The main goals of therapy with a patient with a quadriceps muscle contusion are relieving the pain and improving the ROM. The treatment is mostly non-operative and exists out of three phases:
- Rest, ice, compression. Compression is important in order to limit the hemorrhage for the first 24 to 48 hours. If the patient rests with his knee flexed, it helps to avoid muscle stiffness.
- Active and passive quadriceps muscle stretching with an emphasis on knee flexion. After 24 h, the brace or wrap should be removed and a gentle, active, pain-free range of motion at the knee should be instituted along with stretching and isometric quadriceps strengthening.
- The active phase of treatment, including functional rehabilitation, can begin when pain-free, active knee flexion of at least 120° is attained.
- Improve the functionality and return to sport when full motion and strength are achieved.
- Rest,
- Ice treatment
- Compression
- Elevation
- Rest: Rest prevents the worsening of the initial injury. By placing the injured extremity to rest the first 3-7 days after the trauma, we can prevent further retraction of the ruptured muscle stumps (the formation of a large gap within the muscle), reduce the size of the hematoma, and subsequently, the size of the connective tissue scar.
- During the first few days after the injury, a short period of immobilization accelerates the formation of granulation tissue at the site of injury, but it should be noted that the duration of reduced activity (immobilization) ought to be limited only until the scar reaches sufficient strength to bear the muscle-contraction induced pulling forces without re-rupture.
- At this point, gradual mobilization should be started followed by a progressively intensified exercise program to optimize the healing by restoring the strength of the injured muscle, preventing muscle atrophy, the loss of strength, and the extensibility, all of which can follow prolonged immobilization.
- Ice or cold application: It is thought to lower intra-muscular temperature and decrease blood flow to the injured area. Regarding the use of cold on injured skeletal muscle, it has been shown that early use of cryotherapy is associated with a significantly smaller hematoma between the ruptured myofiber stumps, less inflammation, and tissue necrosis, and somewhat accelerated early regeneration. But according to the most recent data on the topic, icing of the injured skeletal muscle should continue for an extended period of time (6 hours) to obtain a substantial effect on limiting the hemorrhaging and tissue necrosis at the site of the injury.
- Compression: This may help decrease blood flow and accompanied by elevation will serve to decrease both blood flow and excess interstitial fluid accumulation. The goal is to prevent hematoma formation and interstitial edema, thus decreasing tissue ischemia.
- However, if the immobilization phase is prolonged, it will be detrimental to muscle regeneration. Cryotherapy, accompanied by compression, should be applied for 15–20 min at a time with 30–60 min between applications. During this time period, the quadriceps should be kept relatively immobile to allow for appropriate healing and prevent further injury.
- Elevation: The elevation of an injured extremity above the level of the heart results in a decrease in hydrostatic pressure, and subsequently, reduces the accumulation of interstitial fluid, so there is less swelling at the place of injury. But it needs to be stressed that there is not a single randomized, clinical trial to validate the effectiveness of the RICE principle in the treatment of soft tissue injury.
- Active Phase of Management
- The acute phase of treatment is subsequently followed by an active phase of management once the injured leg is recovering well. This phase usually begins approximately 3–5 days after the initial injury depending on its severity. Stretching, strengthening, range of motion, maintenance of aerobic fitness, proprioceptive exercises, and functional training are the primary components of this phase.
- Stretching: Stretching should be done carefully and always to the point of discomfort, but no pain. Various techniques can be utilized including passive, active-passive, dynamic, and proprioceptive neuromuscular facilitation stretching. Generally, ballistic stretching is discouraged due to the risk of re-tearing muscle fibers. If it is pain-free, stretch the quad muscles.
- Static quad stretch: This can be performed in either standing or laying on your front. Pull the foot of the injured leg towards your buttock until you can feel a gentle stretch on the front of the thigh. To increase the stretch, tilt your hips backward. Hold for 20-30 seconds and repeat 3 times. Do this at least 3 times a day.

- Hip flexor stretch: This stretch will focus on the rectus femoris and Iliopsoas muscles. Kneel with one knee on the floor and the other foot out in front with the knee bent. Push your hips forwards and keep the back upright. You should feel a stretch at the front of the hip and top of the thigh. Hold for 20-30 seconds, repeat 3 times, at least 3 times a day.
- 2. Strengthening exercises:
- The aim of strengthening exercises is to gradually increase the load that is put through a muscle. Strengthening exercises can start as early as day 5 as long as they are low-level and must be done pain-free. Isometric or static exercises are advised first and then progress to dynamic exercises with a resistance band and finish with sports-specific running and sprint drills. scientific evidence is lacking on the consensus of treatment principles of muscle injuries.
- Isometrics: Initial isometrics with quadriceps contractions done with the knee fully extended and in different positions at 20-degree increments as knee flexion improves May discontinue isometrics when the patient can sit comfortably.

- Straight leg raises: Sit flat on the floor with the legs straight out in front of you. Raise one leg off the floor keeping the knee straight. Hold for 3 to 5 seconds before lowering back to the ground. Repeat 10 to 20 times. This exercise can be done daily. Progress the exercise by increasing the length of hold and the number of reps.
- Isotonics: Once terminal knee extensions are done properly without extensor lag, free weights are added to the SLRs and terminal knee extensions. Begin with the lightest free weight that the patient can lift; three sets of 10 repetitions up to three times per day. Increase weight by no more than 2-3 pounds at any given time and increase no sooner than every two consecutive workdays.

- Wall squats: From your starting position, slowly lower your body down and hold for a time. As you improve, lengthen the amount of time you hold the wall squat. Be sure to keep your pelvis, back, and head against the wall. Keep the movement pain-free.
- (A variation to increase activation of the VMO would be to squeeze a ball between your knees as you perform the exercise. Typically the ball would be about 12 inches in diameter.)Perform 3 sets of 15-20 seconds holds once per day.
- Step-ups: Start with a box height that is comfortable for you to step upon. Be sure to keep your knee in alignment with your second toe. Step up and keep your pelvis level and your knee in alignment. Be sure to engage the buttocks muscles and fully lock out the knee. Return slowly back down to the ground. The focus should be on the slow eccentric (lowering) back to the ground for 1 second up and 3 seconds down. Perform 2 sets of 15-20 repetitions once per day.







One Comment