Submucosal Plexus (Meissner Plexus)
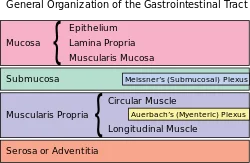
A local circuitry of neurons and ganglia that is located within the gut wall (from the esophagus to the rectum) is known as the submucosal plexus (also known as the Meissner plexus). The gut’s smooth muscle is innervated by it, which is located within the submucosa. The enteric nervous system is made up of the submucosal plexus in conjunction with the myenteric plexus, another plexus of nerves.
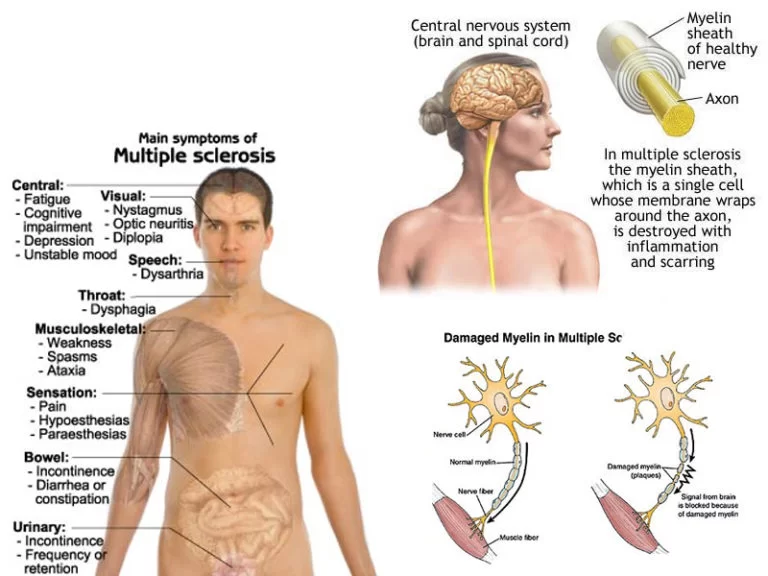
The enteric nervous system aids in controlling the vasculature, secretions, and peristalsis of the gut. Although it is capable of acting independently from the central nervous system, autonomic pre-ganglionic parasympathetic neurons from the anterior and posterior vagal trunks are primarily responsible for controlling its activity. The postganglionic parasympathetic neurons of the myenteric and submucosal plexuses in the gut wall form synapse with these neurons. The vagal discharge causes the gut’s peristalsis and secretions to increase. Numerous disorders, including Hirschprung disease, achalasia, and gastroparesis, can result from enteric nervous system dysfunction.
Structure of Submucosal Plexus
The parasympathetic terminal ganglia, which are formed of unmyelinated preganglionic and postganglionic parasympathetic neurons, control the motility of the mucosa and the secretory activities of the accompanying mucosal glands, are the main components of the submucosal nerve plexus. In addition to the aforementioned, the muscular coat, submucosa, and lamina propria all contain neurons and enteric glial cells (EGCs), a feature of the enteric nervous system. The main function of enteric glial cells is to support gut homeostasis and the integrity of the epithelial barrier.
The myenteric (Auerbach) plexus branches that pass through the muscular layer and into the submucosa are crucial for the development of the nerve meshwork there.
The submucosal plexus is made up of two levels structurally:
motor neurons that project to the circular smooth muscle layer are found in the outer layer. The outer submucosal plexus, also known as the Schabadasch plexus, is this less well-known part.
An inner layer surrounds the muscularis mucosae and innervates both of those structures. This is frequently regarded as the “real” submucosal plexus (Meissner).
Interestingly, the submucosa and submucosal plexus at the junction of the submucosal connective tissue and the innermost circular muscle layer also include a variety of interstitial cells (of Cajal, also known as enteric pacemaker cells). The myenteric and submucosal plexuses can operate independently thanks to these cells, which function as the gut’s electric pacemakers. An inner layer surrounds the muscularis mucosae and innervates both of those structures. This is frequently regarded as the “real” submucosal plexus (Meissner).
Interestingly, the submucosa and submucosal plexus at the junction of the submucosal connective tissue and the innermost circular muscle layer also include a variety of interstitial cells (of Cajal, also known as enteric pacemaker cells). The myenteric and submucosal plexuses can operate independently thanks to these cells, which function as the gut’s electric pacemakers.
Histology
The part of the submucosal plexus that is typically the simplest to recognize in histological sections is the ganglion cells. They have big, circular euchromatic nuclei with a single, outwardly protruding nucleolus, and massive, basophilic-staining cell bodies. As a result, they stand out amid the spindle-shaped fibroblast nuclei in the vicinity.
Function of Submucosal Plexus
The following are some of the duties of the submucosal plexus:
- controls peristaltic action through muscularis mucosae innervation.
- changes the blood flow (vasomotor supply to the submucosal blood vessels)
- increases water and electrolyte release from the stomach tract
- and provides submucosal glands with secretomotor innervation in order to lubricate and shield the mucosal lining from gastric acid.
- aids in nutrition mixing and absorption
Clinical Interactions
intestinal swelling
Inflammatory bowel disease (IBD) and inflammatory bowel syndrome (IBS) refer to a collection of ailments that result in persistent inflammation of the lining of the digestive tract. Major intestine functions like motility, secretion, and feeling can all be severely affected by inflammation. One of the most prevalent signs of IBD and IBS is diarrhea, which is characterized by loose or watery bowel movements and frequently results from overactive secretomotor neurons.
The enteric nerve system’s (myenteric and submucosal plexuses) dysfunction can cause intestinal inflammation, indicating a strong relationship between the neural plexuses and enteric immune cells.
FAQ
The submucosal plexus of the digestive tract serves what purpose?
The submucosal plexus, which is a component of the inner wall, regulates the contraction, absorption, and secretion of local muscle and intestinal tissue.
How does the submucosal plexus control certain things?
The submucosal plexus, also known as the Meissner plexus, is a neuron’s enteric nervous system. It also manages glandular secretions, modifies the transit of electrolytes and water, and controls local blood flow. This plexus governs the luminal surface’s shape.
What makes the submucosal plexus and myenteric plexus different?
The myenteric plexus speeds up and intensifies contractions while increasing the speed and tone of the gut. Local circumstances and the regulation of local secretion, absorption, and muscular movements are handled by the submucosal plexus.
What is the submucosa’s primary purpose?
The submucosa is a connective tissue layer that supports and underlies the mucosa. As an illustration, the submucosa is made up of regular, loose connective tissue. The mucosa can move freely during peristalsis thanks to it.
Where does the submucosal plexus come from?
Wikipedia: Submucosal Plexus
The submucosa of the intestinal wall contains the submucosal plexus, also known as the Meissner plexus, plexus of the submucosa, or plexus submucosus. The myenteric plexus, which in turn derives from the parasympathetic nerve plexuses surrounding the superior mesenteric artery, is where this plexus’ nerves originate.
What causes the submucosal plexus to contract?
Conclusions: Cholecystokinin stimulates the dorsal vagal complex of the hindbrain and inhibits food intake in addition to activating the submucosal plexus at the CCK(1) receptor.
What plexus governs gastrointestinal motility?
The myenteric plexus is a continuous network that connects the internal anal sphincter to the upper esophagus. It predominantly affects smooth muscle function, which controls GI motility via influencing motor control.
What do the digestive system’s two plexuses look like?
The myenteric plexus (Auerbach’s plexus) and the submucous plexus (Meissner’s plexus) are two significant nerve centers that are implicated. In the lower esophagus, stomach, and intestines, the myenteric plexus is between the circular muscle layer and the longitudinal muscle layer.