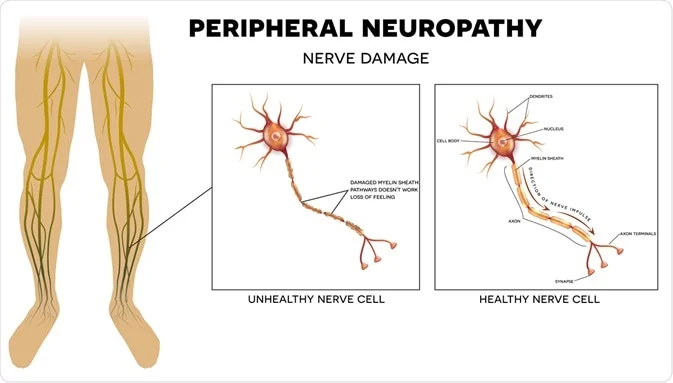
Peripheral nerve injury
- The peripheral nervous system is a network of 43 pairs of motor & sensory nerves that connect the brain & spinal cord (the central nervous system) to the entire human body.
- These nerves control the functions of sensation, motion, and motor coordination. They are more fragile and can be damaged easily.
- When one of these nerves suffers serious injury or trauma, surgical treatment may be called for Peripheral Nerve Injury.
What You Need to Know Peripheral nerve injuries include:
- Brachial plexus injury
- Peroneal nerve injury (foot drop)
- Spinal accessory nerve injury
- Peripheral nerve injuries can be mild or serious, & can be graded on the Sunderland scale, which defines five degrees of severity.
- Injuries may be treated with surgical or nonsurgical therapy.
Causes of peripheral nerve injury:
- Peripheral nerves can be damaged in such ways:
- Generalized diseases: obesity, high blood pressure, age (usually above 40), diabetes, etc.
- Injury from an accident, a sport, or a fall, can compress, stretch, crush or cut nerves
- Medical conditions, such as diabetes, Guillain-Barre syndrome, & carpal tunnel syndrome
- Autoimmune diseases including lupus, Sjogren’s syndrome & rheumatoid arthritis
- Other causes include narrowing of the arteries, hormonal imbalances & tumors.
- Chronic diseases
- Chronic Kidney disorders, hypothyroidism, deficiencies of vitamins like (E, B1, B6, and B12), chronic inflammation damaging connective tissues surrounding nerves.
Peripheral nerve injury symptoms:
- People with traumatic nerve damage can experience severe, unbearable pain, tingling, burning sensation, or total loss of sensation in the part of the body caused by the damaged nerve.
- Numbness
- Loss of sensation in the legs and arms
- A burning sensation in the hands & feet
- people with chronic polyneuropathy often lose their ability to sense temperature & pain, they can burn themselves & develop open sores as the result of injury or prolonged time of pressure.
- If the nerves supplying the organs are involved, diarrhea or constipation may result, as well as loss of bladder or bowel control.
- Sexual dysfunction& abnormally low blood pressure also can occur.
- Every nerve in your peripheral system has its function, so symptoms depend on the type of nerves affected.
- Nerves are classified into:
- Sensory nerves that receive sensation, such as temperature, pain, vibration & touch, from the skin
- Motor nerves that control muscle movement
- Autonomic nerves that control functions such as blood pressure, perspiration, heart rate, digestion & bladder function
- Gradual onset of numbness, prickling, or tingling in your feet or hands, which can spread upward into your legs & arms
- Sharp, jabbing, throbbing, or burning pain
- Extreme sensitivity to touch
- Pain during such activities that shouldn’t cause pain, such as pain in your feet when putting weight on them or when they’re under a blanket
- Lack of coordination & falling
- Muscle weakness
- Paralysis if motor nerves are affected
- If autonomic nerves are affected, Heat intolerance , Not being able to sweat, or excessive sweating
- Bowel, bladder, or digestive problems
- Drops in blood pressure lead to dizziness or lightheadedness
- Numbness, tingling (pins and needles), burning
- Stabbing or shooting pain
- Sensitivity to touch
- Coldness in the area
- Decreased or total loss of movement
- Balance difficulties or falls
- Twitching or muscle cramps
Peripheral Nerve Injury Classification:
- A classification system called the Sunderland classification system defines 5 different degrees of peripheral nerve injury:
- First degree: A reversible local conduction inhibit at the site of the injury. This injury does not require surgical intervention & usually will recover within a matter of hours to a week.
- Second degree: There is a loss of flow of the axons (the “electrical wires”) within the nerve. If this type of injury can be confirmed through pre-operative nerve testing, surgical intervention is mostly not necessary.
- Third degree: There is damage to the axons & their supporting structures within the nerve. Nerve conduction studies performed during surgery are often able to help indicate the outcome & need for simple cleaning of the nerve (neurolysis) or a more repair with grafting.
- Fourth degree: In this case, there is damage to the axons and the surrounding tissues sufficient to create scarring that prevents nerve regeneration. Electrical testing performed during surgery saw that no electrical energy can be passed along the neural pathways in this injured nerve. Surgical intervention with nerve grafting is required to repair the injury.
- Fifth degree: These injuries are mostly found in lacerations or severe stretch injuries. The nerve is divided into two. The only way to repair a 5th-degree injury is through surgery.
- Seddon Classification:
- Neurapraxia
same as Sunderland first degree, “focal nerve compression”
nerve stretch or contusion leading to reversible conduction block without Wallerian degeneration
pathophysiology
usually caused by local ischemia
histopathology reveals focal temporary - Demyelination of the axons (axon remains intact)
Endoneurium remains intact
Electrophysiologic studies
Nerve conduction velocity - Decreases or a complete conduction block
No fibrillation potentials
Prognosis
The recovery prognosis is excellent - Axonotmesis
Same as Sunderland 2nd-4th degree in complete nerve injury more severe than neurapraxia
pathophysiology
Axon & myelin sheath disruption causes focal conduction block with Wallerian degeneration
Variable degree of connective tissue disruption
Electrophysiologic studies
Fibrillations & positive sharp waves on EMG
Prognosis
Unpredictable recovery - Neurotmesis
Encompasses Sunderland 5th degree
Complete nerve division with disruption of endoneurium
Pathophysiology
All connective tissues disrupted
Focal conduction block with Wallerian degeneration
Electrophysiologic studies
Fibrillations and positive - Sharp waves on EMG
prognosis
No recovery unless surgical repair performed
Neuroma formation at the proximal nerve end causes chronic pain
Diagnosis of Peripheral Nerve injury:
- Injury to fully determine the extent of the damage to the nerve, the doctor may use an electrical conduction test to determine the passage of electrical currents through the nerves.
- Two of these tests are electromyography &nerve conduction velocity. These tests are sometimes performed during actual surgery while the patient is sedated.
- The doctor may also suggest any of the following imaging techniques:
- CT scan
- MRI
- Nerve conduction studies
- Electromyography (EMG)
- Nerve conduction velocity (NCV)
- EMG: assesses function at the neuromuscular junction often the only objective evidence of a compressive neuropathy
- Characteristic findings:
- Denervation of muscle
- Fibrillations
- Positive sharp waves (PSW)
- Fasciculations
- Neurogenic lesions
- Myokymic potentials
- Myopathies
- Complex repetitive discharges
- Myotonic discharges
- NCV: assesses large myelinated fibers
- Focal compression & demyelination leads to increase latencies (slowing) of NCV
- Distal sensory latency of > 3.2 ms is abnormal for the CTS
- Motor latencies > 4.3 ms are abnormal for the CTS
- Decreased conduction velocities less specific that latencies
- The velocity of < 52 m/sec is abnormal motor action potential (MAP) decreases in amplitude sensory nerve action potential (SNAP)
- Decreases in amplitude
Differential Diagnosis of peripheral nerve injury:
- Acute Inflammatory Demyelinating Polyradiculoneuropathy
- Diabetic Neuropathy
- Cervical Spondylosis
- Femoral Mononeuropathy
- HIV-Associated Distal Painful Sensorimotor Polyneuropathy
- HIV-Associated Multiple Mononeuropathies
- Leptomeningeal Carcinomatosis (Metastasis)
- Neuromuscular and Myopathic Complications of HIV
- Pediatric Guillain-Barre Syndrome
- Peroneal Mononeuropathy
- Polyarteritis Nodosa
- Radial Mononeuropathy
- Spinal Cord Hemorrhage
- Spinal Cord Infarction
- Spinal Metastasis
- Syringomyelia
- Vasculitic Neuropathy
Treatment of peripheral nerve injury:
- Nonoperative
- Observation with sequential EMG
- Indications
- Neuropraxia (1st degree)
- Axonotmesis (2nd degree)
- Gunshot wounds affecting brachial plexus
- Assess the extent of recovery over 3 months
- Operative
- Direct muscular neurotization
- Indications
- A transected unrepairable nerve ending at risk of becoming neuroma
- Plan for integrated prosthesis
- Outcomes
- The degree of functional recovery varies
- Decreases neuroma formation
- Promising results with targeted
- Muscle reinnervation (TMR) for amputation
- Surgical repair
- Indications
- Neurotmesis (3rd-5th degree)
- Early surgical exploration: iatrogenic injury, penetrating trauma, vascular injury, progressive deficits an exception like gunshot wounds affecting brachial plexus may be observed one to three weeks after gunshot injury with confirmed neurotmesis
provide time for the zone of injury to be declared - Nerve grafting
- Indications
- Gaps that prevent tension-free direct repair
- Nerve transfer
- Indications
- Proximal nerve injury
- Goal to deliver new axons & stimulus before degeneration of motor endplates & irreversible muscle damage
priority is to regain shoulder abduction, external rotation, elbow flexion, & finger function - Loss of shoulder abduction & external rotation
- Spinal accessory nerve (Cranial nerve XI) to suprascapular nerve
- Loss of shoulder abduction & flexion
- Tendon transfer
- Indications
- Return of function through nerve regeneration is not happening complications of tendon transfer potentially increased scarring & damage to the blood supply.
Complications of peripheral nerve injury:
- Adhesions
- Poor tendon gliding
- Neuroma formation
- Pain & Hypersensitivity
- Significant pain can happen with peripheral nerve injury, particularly with nerve root avulsions, causing neuropathic pain.
Severe pain can also mainly lead to complex regional pain syndrome, all of which can impact rehabilitation. - Adequate pain control for rehabilitation is of main importance.
- Altered Sensation
- Peripheral nerve injury is often combined with significant changes in sensation, with numbness, tingling, burning sensation, or total
- loss of sensation in the part of the body affected by the damaged nerve, which can increase the risk of further secondary injuries as a result of this altered reduced sensation such as pressure ulcers, burns, & lacerations.
- Pressure Ulcers
- Pressure sore in a patient with foot drop
- Patients with lost or decreased sensation as a result of a peripheral nerve injury are at increased risk of developing pressure ulcers, which can be difficult to see on dark skin.
- A pressure ulcer is a localized injury to the skin & tissue usually over a bony prominence, as a result of pressure, or pressure in combination with the shear.
- A pressure sore can occur in a few hours, but the results can last for many months& can cause significant loss of function &impairment.
- Tissue injury is related to both intrinsic & extrinsic factors.
- Extrinsic factors include pressure, shear, friction, immobility & moisture.
- Intrinsic factors related to the condition of the patient such as local infection, decreased autonomic control, sepsis, altered level of consciousness, increased age, vascular occlusive disease, anemia, malnutrition, sensory loss, & contracture.
- Keeping the skin dry, regular position changes ®ular skin checks (use a mirror if necessary) will help.
- Burns & Lacerations:
- Burns & skin lacerations as a result of contact with hot surfaces or water, sharp surfaces or not using protective clothing, e.g. shoes are common with altered or decrease sensation following peripheral nerve injury.
- Test water with the opposite, or sensate limb and always wear covered supportive shoes if foot sensation is reduced and gloves in hand.
- Delayed Healing:
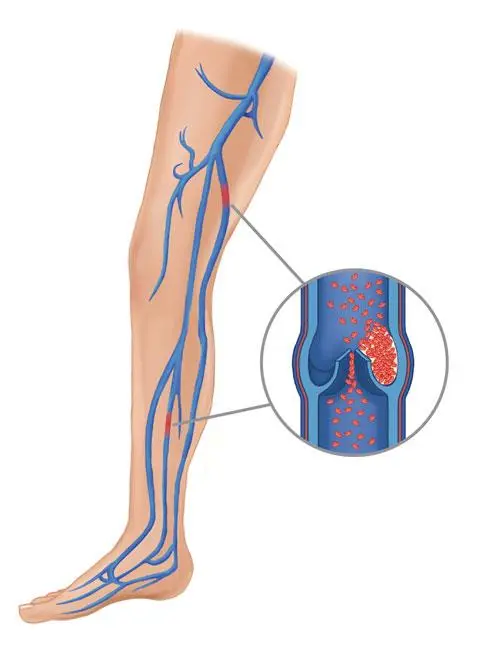
- Peripheral nerve injury can have an impact on healing, & slow down the healing mechanisms of soft tissue. This can be further exacerbated by muscle weakness, which can impact the circulation of blood in distal limbs causing swelling & thus poor healing.
- Other factors that may impair the healing process include; Smoking significantly reduces blood flow to the injured nerve & soft tissue
Diabetes, Nutrition can delay healing if inadequate protein & nutritional intake. - Swelling: As peripheral nerve injury leads to motor impairment in extremities, it affects the muscle pump from the distal aspect of limbs, particularly in a sciatic nerve injury, which may cause blood pooling in distal limbs when limbs are in a gravity-dependent position. This may lead to further neuropraxia as a result of increased compression of the nerve and increased pain.
Limb elevation & range of movement (passive, active-assisted, or active) can encourage the movement of fluid & help with swelling. - Contracture & Deformity: Contractures result from a loss in the extensibility of the soft tissue structures-skin, ligaments, muscles, & joint capsules crossing joints, leading to restriction in joint mobility, causing joint stiffness, & later on the deformity. Contractures reduce joint mobility & restrict activities of daily living. They are also associated with pain, spasticity, sleep disturbances & skin breakdown. Most often contractures affect the joints important to daily living: hips, knees, ankles, wrists, & shoulder, causing problems with dressing, eating, transferring, sleeping comfortably, using a wheelchair, or doing any tasks that require full joint motion. Problems in any of these areas can reduce a person’s independence. If the joints of the affected muscles are not moved passively daily, the muscles shorten & joints can become stiff causing contracture and deformities. Positions or postures in which the patient stays most of each day in bed or wheelchair increase the chances of contracture, as can pain, which increases the chances of contracture as a result of increased chances to contract the non-paralyzed muscles, which increases the time soft tissues spend in shortened positions. Stretching, range of motion& strengthening exercise, splinting, serial casting& positioning should all be used to prevent & manage contractures.
- Neuroma:
- A neuroma is a common complication of a peripheral nerve injury or amputation, & it can cause tremendous pain that is often resistant to most analgesics. Neuromas are a non-cancerous thickening of nerve fibers made up of non-conducting tissue that stops the signal from being sent along the nerve. Neuromas are formed when nerve regeneration is blocked by scar tissue, preventing further regeneration. Neuromas are a potential, limiting complication of nerve recovery which can lead to pain or hypersensitivity; they usually do not develop until at least 6 weeks post-injury. The motion of adjacent tissues or direct application of pressure on neuromas often leads to pain by stimulating the nerve enclosed by the neuroma.
- Muscle Weakness:
Involvement of motor nerve leads to weakness of muscles supplied by that nerve. A consequence of denervation is muscle atrophy & functional deficits. A healthy neuromuscular junction is required for the nervous control of muscles. TENS has been seen in numerous studies to have a positive effect on maintaining neuromuscular junction health & preventing muscle atrophy.
Muscle care is most important to prevent damage to muscle units, in particular, preventing: heat or cold trauma; overstretching by gravity or incorrect lifting/transfer techniques; contractures of muscles. When muscle strengthening exercises can add it is important not to damage the healing nervous tissue: if pins & needles, numbness or increased pain occurs if the exercise is too hard & progressed too quickly & can harm healing. - Psychological Stress:
- Muscle weakness, contractures, deformity, & pain can affect mental health following peripheral nerve injury.
- Chronic neuropathic pain has a life-debilitating effect causing emotional stress & reduced quality of life, and increased risk of posttraumatic stress disorder, depression, or anxiety. The goal is not simply to reduce pain but to achieve an improved quality of life, which can only be achieved if depression, anxiety, & sleep disorders are also addressed.
Risk factors of Peripheral nerve injury:
- Diabetes, especially if your sugar levels are not controlled
- Alcohol misuse
- Vitamin deficiencies, particularly B vitamins
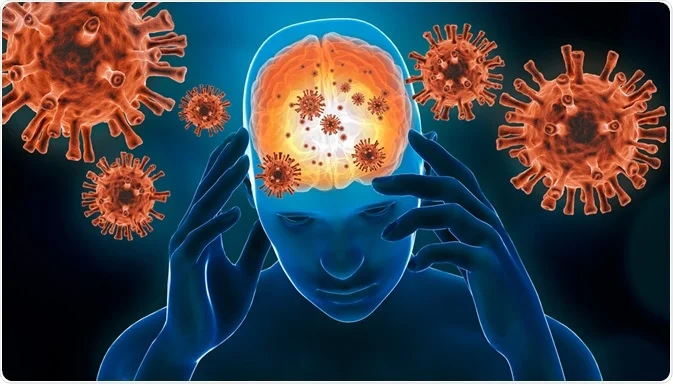
- Infections, such as Lyme disease, shingles, Epstein-Barr virus, hepatitis B & C, & HIV
- Autoimmune diseases, such as rheumatoid arthritis & lupus, in which your immune system attacks your tissues Kidney, liver, or thyroid disorders
- Exposure to toxins
- Repetitive movements, such as those performed during jobs
- Family history of neuropathy
- Prognosis with treatment
- Variable on several factors including injury location, age of the patient, & type of injury
neurapraxia resolves with conservative measures axonotmesis and neurotmesis may improve with repair, tendon transfers, & nerve transfers the endoneurium must be intact for full recovery of an injured peripheral nerve leading to chronic neuropathic pain. - Peripheral Nerve Injury Treatment:
- Depending on the peripheral nerve injury treatment can range from surgical repair to conservative methods such as physiotherapy.
- With surgery, the damaged part of the nerve is removed, & the surgeon attempts to reconnect the healthy nerve ends (nerve repair); or in such cases, a nerve from another part of the body will be implanted (nerve graft). Many peripheral nerve injuries are managed with physiotherapy.
Physiotherapy management is also suggested after surgical management for this condition.
Management begins with detailed history & assessment of how the injury is affecting the patient.
Physiotherapy treatment for peripheral nerve injury:
- Pain management – Acupuncture, TENS, and massage can help decrease the pain associated with these injuries.
- Muscle weakness – Appropriate & graded muscle strengthening exercises are incorporated dependent on the level, timing & nature of injury. This may add isometric, electrical stimulation, active assisted & supported slings to help with the strengthening process.
- Splinting&Bracing – Use of a splint or brace necessary to help avoid overstretching or contractures while supporting the joint.
- Sensory retraining – Techniques are used to stimulate the different types of sensory systems
- Proprioception exercises – Using exercise &various aids to promote joint sense and balance in the limbs
- Neuropathic pain affects the quality of life & is a common consequence of nerve damage.
- Pain control is of paramount importance.
- Complete relief is rarely obtained and 40-60 % find means to obtain partial relief.
- Anticonvulsants & tricyclic anti-depressants are the medications most commonly used for neuropathic pain.
- A Physiotherapist can use other modalities that are useful for pain relief. These include Massage eg. aromatherapy massage to help manage neuropathic pain.
- Transcutaneous Electrical Nerve Stimulation (TENS). The application of TENS gives benefits in pain reduction in neuropathic pain. It was found to be of benefit if used at 100hz in constant mode.
- Low-Level Laser Therapy (LLLT). Studies have found this to be of benefit in pain relief & acceleration of healing in the treatment of neuropathic pain & neurological deficits as adjuvant therapy.
- Relaxation Techniques
- Acupuncture
- Muscle Weakness:A consequence of denervation is muscle atrophy & functional deficits. A healthy neuromuscular junction (NMJ) is required for the nervous control of muscles. TENS has been seen in numerous studies to have a positive effect on maintaining NMJ health & the prevention of muscle atrophy.
- Muscle care is of most importance to prevent damage to muscle units, in particular, preventing: heat or cold trauma; overstretching by gravity or incorrect lifting & transfer techniques; contractures of muscles. Techniques used by physiotherapists to achieve the above goals are massage, US, hydrotherapy, splints, passive ROM stretches & correct transfer skill education.
- When muscle strengthening exercises can commence it is important not to damage the healing nervous tissue: if pins& needles, numbness, or intense pain occurs the exercise is too hard and can harm healing.
- Muscle strengthening exercises are introduced as appropriate, eg isometric, graded weight progression, open-close chain, & Use of support slings may be employed to assist the movement & take the weight of the limb. In addition, splinting techniques, frequently have a place in the management of peripheral nerve injuries, including postoperative splinting &casting, as well as splints to prevent deformities from developing, or even to overcome established contractures & improve function, & in this way aid the patient’s recovery.
- Static & dynamic splints can help to rest paralyzed muscles in optimum positioning to avoid overstretching & or contractures. They also help unaffected muscles to operate from correct positions.
- Moderate intensity exercise- It helps to improve strength & physical function.
- Nerve gliding activities- Includes exercises shown by a physiotherapist who will help you move & glide your nerves.
- Balance & coordination activities – Your physiotherapist works on strategies to improve your balance & coordination. Improving balance & coordination helps to decrease your risk of falling & injuries that arise due to it. Balance exercises are a main part of the recovery of peripheral neuropathy. Balance training is important in overcoming the feeling of stiffness & unsteadiness, especially among elderly people.
- Education – Your physiotherapist guides you on how to safely manage peripheral neuropathy. It mainly focuses on improving your safety, preventing further complications, & finding alternative ways to perform certain tasks.
- Kinetic therapy in peripheral nerve injuries- It should not be started until the last stage of nerve regeneration when progressive strength return can be seen. After an injury to the nerve, physiotherapeutic methods are used to eliminate paresis & restore normal the function of muscles and also to improve circulation.
- Electrostimulation – It provides an important role in the treatment of various neuromuscular dysfunctions.
- Magnetotherapy- It is applied where a pulsed low-frequency magnetic field is applied. It has well-known effects on increasing
- enzymatic activity, oxy-reductive processes & proper blood circulation resulting in better oxidation & conduction characteristics of
- regenerating peripheral nerves. It increases the regeneration of nerve fibers.
- Bio-laser stimulation- where low-energy biostimulation lasers are required in a palatial, continuous manner. Laser radiation can help to used to rejoin the nerve stumps.
- Functional deficits & sensory deficits In the relearning of functional tasks, the brain is utilized to regain
- Vision-tactile & audio-tactile interaction. In the upper arms, the focus is on fine motor skill learning. In the lower limb balance and coordination are areas of focus.
- Sensory reeducation aids in the recovery of sensibility. In sensory stimulation pinching & tapping, brushing & icing are regularly used.
- Proprioception deficits can be improved by using eg balance pads for WB activities, exercise balls, juggling balls for upper limbs,
- yoga,
- Tai-chi.
- Joint Stiffness:
The soft tissues of the region & adjacent regions supplied by the damaged nerve are at risk of contractures if left in shortened positions. Passive range of motion exercises daily is useful to prevent these problems and protective removable static splints can also be useful in contracture prevention. For joints that have become stiff ultrasound & laser, therapies have been found to be effective. - Emotional Stress:
Chronic neuropathic pain has a life-debilitating effect causing emotional stress & reduced quality of life. To properly treat a patient with neuropathic pain must be respected. The ultimate goal is not simply to decrease pain but to achieve a better quality of life. This can only be achieved if depression, anxiety, & sleep disorders are also addressed. - Ergonomic casts or splints:
Ergonomic casts & splints can help you if your neuropathy affects your muscles. Splints can help with muscle weakness.
These casts give support to the part of your body that’s uncomfortable. This can relieve pain. For example, a splint or cast that holds your wrists in a proper position, while you sleep, can relieve the discomfort of carpal tunnel syndrome. - Self-care:
In addition to pain relievers, many people have found relief for peripheral neuropathy through having a foot bath with nettle leaves or chamomile for at least 25 minutes using a heating pad or electric socks applying an ice pack to affected areas for 15 minutes twice daily in the morning & the evening trying acupuncture undergoing biofeedback use different types of holistic therapy such as reflexology, tai chi, or reiki massaging affected areas to increase circulation avoiding pressure on the affected area, like not crossing legs or leaning on elbows seeking social support & activities with others setting priorities daily & not doing more than you feel you are capable of avoiding caffeine & developing a regular bedtime routine to promote sleep. - Moderate, regular exercise can also help to decrease discomfort.
- If you drink alcohol or smoke, consider stopping or cutting back.
- Both alcohol & tobacco aggravate nerve pain & can cause nerve damage when used for long periods.
Take precautions at home :
- If you have peripheral neuropathy, you’re potentially at more risk for accidents in the home.
- To increase safety:
- Use safety guards & other tools for sharp objects like scissors & knives.
- Use thermometers to measure the temperature of tap water & bath.
- Use potholders & gloves when handling hot items.
- Use a walker & cane for added stability.
- Put nightlights to avoid tripping in the dark.
- Carefully wrap your hands & feet when it’s cold out.
FAQ
Does massage help nerve regeneration?
A massage helps to decrease the effects of injury by relieving the compression of nerves and encouraging repair of damaged nervous tissues to increase. Relief of compressed nerves & healing of damaged nervous tissues reduces negative sensations such as pins & needles & numbness to improve sensation.




2 Comments