The Difference Between Trigger point and Tender point
What are trigger points and tender points?
Trigger points are defined as areas of the muscle that are painful to palpation and are characterized by the presence of taut bands and a generation of a referral pattern of pain. Tender points are areas of tenderness occurring in the muscle, muscle-tendon junction, bursa, or fat pad. When tender points occur in a widespread manner, they are generally considered characteristic of fibromyalgia. Trigger points, which generally occur in a more restricted regional pattern, are indicative of myofascial pain syndrome. In a few patients, the two phenomena may coexist, and overlap syndromes can occur. Although experienced examiners can typically identify the same tender points, inter rater reliability of trigger points has been low in most studies. There is continued controversy regarding the defining characteristics and homogeneity of myofascial pain because of the variability of examination findings. In appropriately selected patients, it appears that myofascial trigger point injections can help reduce pain and improve the range of motion in conjunction with a comprehensive exercise and rehabilitation program.
Introduction of Tender Points
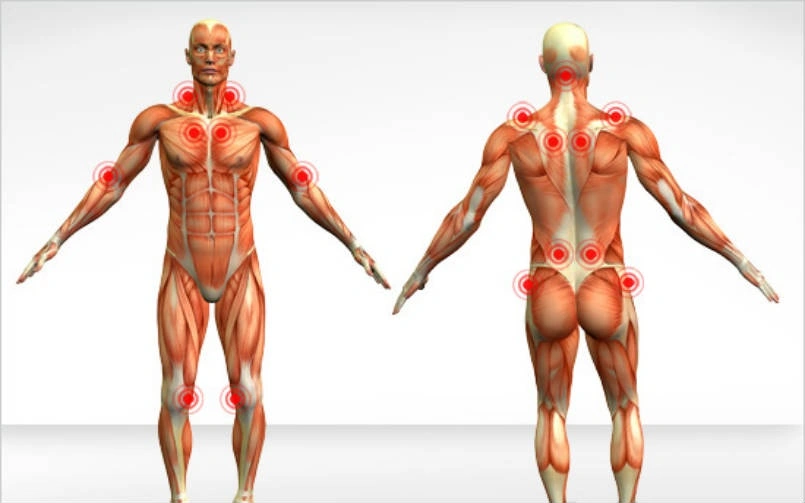
Tender points are used to help diagnose fibromyalgia. They are extremely sensitive spots on the body that elicit pain when 4 kilograms or about ten lbs. of pressure are applied. There are eighteen specific tender points located at nine bilateral locations.
Tender points are eighteen specific places on your body that were previously the sole manual diagnostic criteria for fibromyalgia. If you had a history of widespread body pain for more than 3 months, and if your rheumatologist determined you were tender in at least 11 of these 18 places, you had fibromyalgia. If you had fewer than eleven tender points, you did not it was as simple as that.
Over time, although, it became apparent that tender points come and go. A Few days a patient might have only nine or 10; at other times, a patient might have 15, or even all 18. Then other issues such as non-refreshing sleep, cognitive difficulties, jaw pain, irritable bowel syndrome, headaches, anxiety, and depression became recognized as fibromyalgia symptoms. The current diagnostic method for fibromyalgia is more comprehensive than before, and the tender point exam is one of many factors considered.
Introduction of Trigger Points
The trigger points are a place on the body that, when pressure is applied, refers (or “triggers”) pain to another part of a body. A point itself may or may not be sensitive. Trigger points typically involve taut, ropy bands of muscle fibers. There may also be hard lumps or nodules in an area.
Trigger points are formed when acute trauma or repetitive microtrauma causes the development of stress on the muscle fibers. However anyone can have trigger points, they are frequently associated with a form of chronic muscle pain called myofascial pain syndrome. It is not unusual for someone with fibromyalgia to also have myofascial pain syndrome, which may be one of the reasons trigger points and tender points are often confused.
Trigger points are different from tender points. You may have many of them, and they can be located in any of the 600 muscles of The body. the person who has myofascial pain syndrome can have multiple trigger points throughout her body.
Each trigger point is a hard, sore spot within the skeletal muscle. Its distinguishing feature is referred pain; that is, pain is felt in a remote location as well as locally. For eg, my recent bout of occipital neuralgia involved two trigger points just beneath the right side of my skull. It was acutely painful in those two places and equally painful on the top of the head.
Trauma or repetitive motion is often responsible for stress on muscle fibers and the activation of the trigger points. People who frequently experience stress and anxiety may be more likely to develop the trigger points in their muscles. It is thought that clenching of a muscle is a form of repeated strain that leaves muscles susceptible to the formation of trigger points. In my case, it was likely to lead to by too many hours spent sitting at the computer with perfect posture.
Activated trigger points are extremely painful. Common treatments are physical therapy, ice packs, heat, anti-inflammatory medications, massage, acupuncture, and injection. Sometimes the treatments will be effective and fast. At another time, healing is slow, and the pain can persist. Once treated, the trigger point may subside to a latent form, and be painful only when pressure is applied. Although, it doesn’t vanish. Another trauma or additional repetitive motion may lead to it erupting into an active, painful state again.
Trigger points are those tender lumps in a muscle that your therapists find. They begin small, and you only know they are there when your therapist gently presses them upon them. and over time they can grow to where they are quite substantial but still not leading to pain, but will eventually begin shooting pain when they are aggravated.
A trigger point is a sore point in the muscle when you push on it or what most people would be called the knot. You know that bit of muscle when you are rubbing the tight shoulders that just does not feel right and hurts? When a trigger point is very sensitive it can cause pain without being pressed on and this is a major lead to muscular pain that most people suffer from. A trigger point(TrPs) is a “hypersensitive nodule within a taut band of tissue that can be referred to as pain”.
A Few of the ideas suggested that the referral pain you experience is happening in the brain. It is such as “crosstalk”. and you obtain electrical cables that are close to each other. This can happen in the brain sensation areas in the brain. and that are close to each other. an example, if the trigger point is in the gluteus muscles and refers down the leg area of the leg is close to the area in a brain and that is why you feel it there. A few simple ideas are that the muscle may be attached to the area you feel the referral, which is common and might be transmitted through a fascia or nerves.
Referred pain also called reflective pain, is pain perceived at a location other than a site of a painful stimulus. Pain is reproducible and does not follow dermatomes and myotomes, or nerve roots. There are no specific joint swelling or neurological deficits. Pain from a myofascial Trigger Point is a distinct, discrete, and constant pattern or map of pain with no gender or racial differences able to reproduce symptoms – referred pain map. Radiating pain is slightly various from the referred pain. for eg, the pain related to a myocardial infarction could either be referred to as radiating pain from the chest. Referred pain is when the pain is located away from and/or adjacent to an organ involved. for instance, when a person has pain only in his or her left arm or jaw but not in the chest.
Trigger points are focal, discrete, and hyperirritable spots located in a taut band of the skeletal muscle. They produce local pain in a referred pattern and frequently accompany chronic musculoskeletal disorders. Repetitive microtrauma or acute trauma may lead to the development of stress on muscle fibers and the formation of trigger points. Patients might have regional, persistent pain resulting in a decreased range of motion or movement in their affected muscles. These include muscles that help to maintain body posture, like those in the neck, shoulder, and pelvic girdle.
Trigger points may also manifest as tension headache, tinnitus, temporomandibular joint pain, reduce or diminished range of motion in the legs, and low back pain. Palpation of the hypersensitive bundle or nodule of fiber of muscle harder than normal consistency is the physical finding normally associated with a trigger point. A Palpation of a trigger point will raise pain directly over the affected area and/or lead to radiating of pain toward a zone of reference and the local twitch response.
other treatments and many modalities, such as the Spray and Stretch technique, ultrasonography, Transcutaneous electrical nerve stimulation(TENS), manipulative therapy, and injection, are used to inactivate trigger points. The trigger-point injection treatment is one of the most effective treatment modalities to inactivate trigger points and provide prompt relief of a symptom.
Trigger points radiate pain to the affected area when pressure on sensitive points in a muscle is applied to them and sometimes spontaneously with no pressure. and sometimes in seemingly unrelated or not related body parts. This is called referred pain.
Types of trigger points
There are types of trigger points an active trigger point, a latent trigger point, a secondary trigger point, and a satellite trigger point.
An active trigger Point
- An active trigger point is defined as leading to pain when no pressure is placed on them. and this means that is painful even if you are not massaging that. This is only one of the most common leads to Myofascial pain and it can be experienced in any area of the body. Common eg, an active trigger point is back pain including knee pain, sciatica, neck pain, headaches, and so on. when you gently press on the affected area, the red areas are the referral pain pattern. This helps to diagnose where the trigger points that are. On palpation, An active Trigger point is any point that leads to tenderness and referral pain pattern. Almost always central. some satellite Trigger points are also active but not necessarily all of that and trigger points are active. These trigger points commonly lie within a muscle and pressure on it results in local or regional pain. These active trigger points are an area of severe tenderness that typically lies within the skeletal muscle and is associated with local or regional pain. An active trigger point is nodules within a taut band of muscle. They are generally the source of muscle pain. They are very tender. and produce a twitch in a muscle when touched.
A latent Trigger Points
- A latent trigger point is a point you gently press on that leads to pain and often refers pain to in another area. This type of trigger point is seen as the precursor to the type of active trigger point. If you have this type of trigger point that gets worse through further strain then they can become active trigger points and that is when you typically feel pain and/or that need anyone to assist you to get out of the pain. Inactive trigger points or Latent Trigger points can develop anywhere and under fingertips feel like lumps, but they are not painful. It can aggravate the stiffness of the muscles. It has the potential to be active but is dormant(potential ). these trigger points are the dormant (inactive) area that has the potential to act like trigger point. It may cause weakness of a muscle or a restricted or limited range of movement. This nodule does not lead to pain when touched. They can remain inactive for years and become active when there is stress or/and trauma.
A secondary trigger point:
- This is located in the muscle other than the one that holds the active trigger point. It can be disturbed at the same time as the active trigger point. This is a painful point in a muscle that becomes active when you stress other muscles.
A satellite Trigger Points
- A satellite trigger points are the area where the pain is referred to. For example, if you get pain in the shoulder or you found that the trigger point was in the shoulder referring to an elbow, an elbow point would be this type of trigger point. And so you would be also working on the elbow trigger points as they would be consistent as well. Central or Primary Trigger Points are those that cause severe pain locally at the pressure with irradiation according to referred pain map. often they are based around the center of a muscle belly. Secondary trigger points or Satellite Trigger Points arise in response to existing central trigger points around muscles. They normally spontaneously withdraw when the central Trigger point is healed. It can be present in a cluster form. The trigger points become inactive because it overlaps with the region of other trigger points. The painful spot becomes active because it’s situated near other trigger points.
Active and Passive Trigger Points
- That are mainly two types of trigger points that your physical therapists treat: active trigger points and passive trigger points. A passive trigger point is simply hurt at its exact location. If you have a painful muscle knot in the muscles and someone presses on it, the pain will be felt right where the pressure is on the knot.
- The active trigger point refers to pain in another part of the body. eg, If someone presses on an active trigger point in the posterior of the leg or calf. you might feel pain in your leg along with symptoms in your foot.
- Regardless of the type of trigger point you have or the fact that we do not fully understand what is occurring when trigger points are formed. And you might benefit from physical therapy to assist manage your problem.
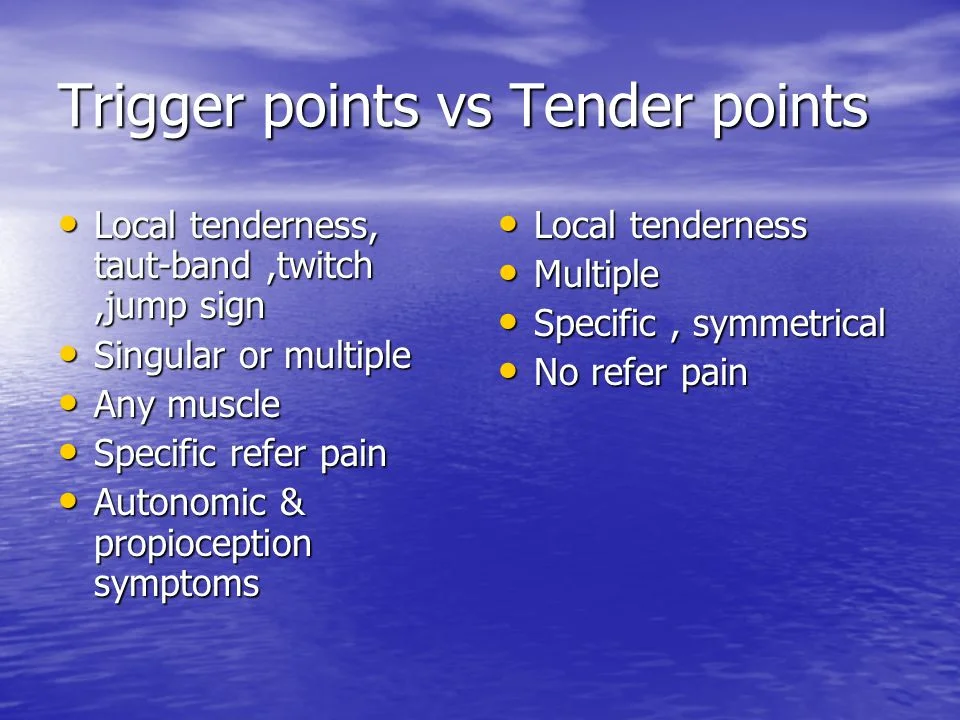
Trigger point vs Tender point Comparison
| comparison | Trigger Point | Tender Point |
| Definition | Trigger points are defined as areas of the muscle that are painful to palpation and are characterized by the presence of taut bands and a generation of a referral pattern of pain. | Tender points are areas of tenderness occurring in the muscle, muscle-tendon junction, bursa, or fat pad. |
| Pain Pattern | Trigger points refer pain to in other areas. | Tender points do not cause referred pain. |
| Location | located in a taut band of the skeletal muscle | The tender points associated with fibromyalgia occur in symmetrical pairs from the back of your head to your inner knees. |
| Points | There may be a single point or several points. | There are always multiple points. |
| Treatment | inhibitory soft tissue deep massage coolant spray with myofascial stretch Ischemic Compression Technique Trigger point release therapy Myofascial release therapy Kinesiology taping Acupuncture therapies and relaxation therapies | Pain relieving medicine Ultrasound Therapy Hot Pack Cold Pack |
The Differences Between Tender Points and Trigger Points
- The specific point is tender.
- The point itself may and/or may not be tender.
- Tender points do not cause referred pain.
- Trigger points refer pain to in other areas.
- There are always multiple points.
- There may be a single point or several points.
- Points occur in specific symmetrical locations.
- Points may occur in any skeletal muscle.
Where are trigger points and tender points located?
Location of trigger points
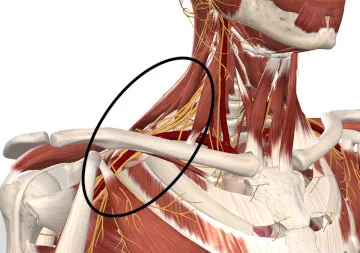
Trigger points and muscle knots can happen anywhere in a body. and Wherever that is muscle tissue, there may be a small area of tissue tension. it could be a trigger point. Areas in the body where trigger points are more frequently found may include:
- The Upper trapezius muscles on either side of your neck just above the shoulders
- The quadratus lumborum muscles of low the back
- Your hamstrings
- Your calf muscles
- Along your iliotibial band
- You can get trigger points everywhere in the body, and if they occur excessively, you may experience myofascial pain syndrome and chronic pain.
Trigger points
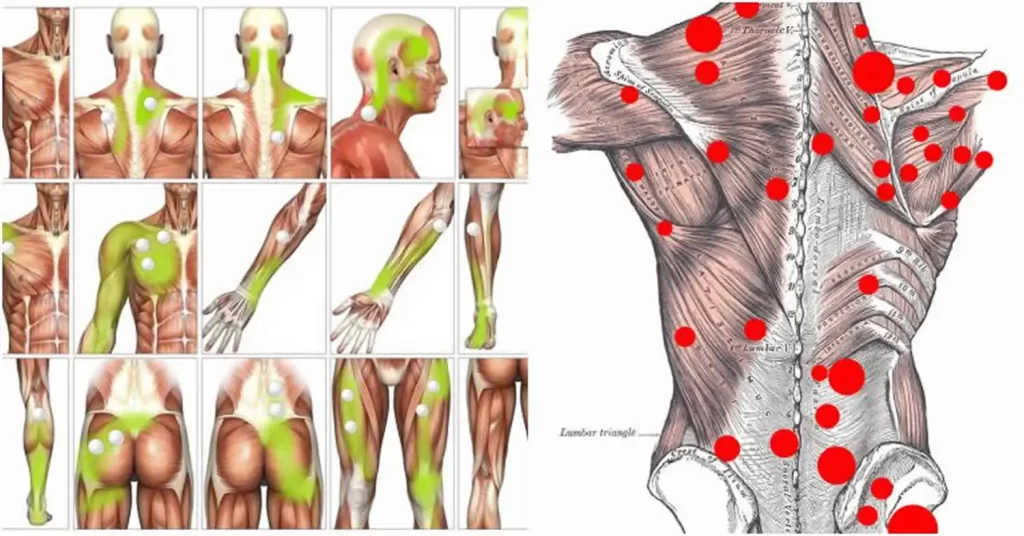
Location of tender points
- The tender points associated with fibromyalgia occur in symmetrical pairs from the back of your head to your inner knees.
Tender points
What are the causes of trigger points and tender points?
Causes of the trigger points
Some ideas have been seen to cause trigger points. inadequate nutrients in the tissue consist of oxygen. When the blood supply to parts of the muscle is reduced it can cause nodules in the tissue that then cause pain. Overuse or overactivity of a muscle through exercise, posture, and working at a computer every day without breaks can lead to the muscle fibers becoming chronically contracted which over time causes pain. An injury is such as strain on the muscle/fascia. and when this heals it might leave trigger points.
- Aging,
- Injury sustained by a fall, birth trauma, or/and stress.
- Lack of exercise: Generally in sedentary persons, of which 45% are men,
- Bad posture: upper crossed pattern and lower crossed pattern, swayback posture, telephone posture, and cross-legged sitting.
- Muscle overuse and respective micro-trauma, weightlifting,
- Chronic stress conditions such as anxiety, depression, psychological stress, and trauma.
- Vitamin deficiencies: vitamin D,vitamin C,vitamin B; folic acid, and iron.
- Sleep disturbance or poor sleep,
- Joint problems and hyper-mobility.
Causes of the Tender Points
- Doctors do not know what leads to these pressure points. But they know that their locations are not random. They happen in predictable places on a body. That means many people with fibromyalgia have the same symptoms with their tender points.
What are the symptoms of trigger points?
How do you know if it is the trigger point or not?: There are a few common symptoms you will get that can differentiate trigger points pain. the nodule or band you are pressing on is in the muscle and not on the nerve or bone. The point you gently press on referred to pain. This is not like nerve pain as when you gently press on the nerve it is like an electric shock or needles or pins. the trigger point referral is not like this. some are more of a dull aching pain that radiates pain. if have muscle pain that won’t go away and even gets worse when you exercise or move. You have chronic muscle pain.
- A patient commonly asks for help due to a chronic pain state eg: headaches, aches everywhere, morning stiffness, Temporomandibular joint syndrome, and tinnitus, which, in reality, is often physically away from the active trigger point.
- Weakness of a muscle or imbalance, altered motor recruitment, in either the affected muscle or in functionally related muscles.
- Changes in Range of Motion (ROM).
- Painful movement. and/or that movement a few times can exacerbate symptoms.
- Tension headaches, migraines, tinnitus, and temporomandibular joint problem. as accompanying symptoms.
- Postural abnormalities and compensations
- Pain is described as deep aching in a localized area of muscles, throbbing, tight, stiff, or vice-like.
- Pain that persists or worsens
- A tender knot in a muscle. Trigger points are small bump, nodule, or knot in the muscle that causes pain when touched and sometimes when it’s not touched.
- Muscle pain that is gets worsens when the affected or injured muscle is stretched or strained
- Sleep disturbances due to pain and disturbances in behavioral
- Reduced or decreased range of motion in your affected areas (for example., you may be unable to completely rotate your shoulder).
- Muscle stiffness
- Fatigue
- Headaches
- Dizziness
- Mood swings
- Muscles that are tender or sore.
- Weakness in the affected muscle(s).
- Pain that gets worsens in an affected muscle or does not improve with time
- Presence of painful knots in the muscles that when gently pressed produce intense localized or referred pain.Trigger points that activate a pain
- Abnormal posture or affected postures such as hunching, shoulder rounding, or forward head posture (not aligned with the spine).
Trigger points develop in the myofascial, mainly in the center of the muscle belly where the motor end plate enters (primary or central Trigger Points). Those are palpable nodules within a tight muscle at the size of 2 to 10 mm and can demonstrate at different places in any skeletal muscle of a body. We have many trigger points in our bodies. That can be present even in children. and but that presence does not necessarily result in the formation of pain syndrome. When it happens, Trigger Points are directly associated with myofascial pain syndrome, somatic dysfunction, restricted daily functioning, and psychological disturbance.
What Can Make Tender Point Pain Worse?
Several things can make fibromyalgia symptoms worse. They include:
- Anxiety
- Changes in the weather for eg, cold or humidity
- Depression
- Fatigue
- Hormonal changes, such as PMS
- Infections
- Lack of sleep or restless sleep
- Emotional stress
- Physical exhaustion
- Not moving around enough
Myofascial Pain Syndrome and Trigger Points
Myofascial pain, also known as trigger points hypersensitive areas of a muscle. Trigger points within a muscle can be chronic or develop over time due to repetitive stress on your muscle. This can occur during the activity or lack of muscle activity such as immobilization. latent trigger points and active trigger points are two types individuals may experience. Active trigger points are more common. If an individual has the active trigger point, they would present with extreme tenderness and pain over muscle. Whereas, some trigger points may lead to referred pain which symptoms may be felt in other areas of the body.
How are a trigger point and tender point diagnosed?
How is a trigger point diagnosed?
Analysis of a patient’s medical history is a significant step in diagnosing any medical condition. the patient’s family history of diseases shall be properly checked to look for any sign of fibromyalgia, as it is a significant factor in determining this type of condition. The patient’s routine of physical activities, demands of the occupation in the case of athletes, people with desk jobs, manual laborers, diet intake, stress patterns, sleep routine, and medications, etc. and also need to be examined in detail to reach a logical factual conclusion. a thorough examination of lumps or nodules found on a muscle should be done. if it should also be made sure whether the occurring pain is local pain or referred.
There are main 4 criteria to diagnose the trigger point.
- A taut band within a muscle fiber.
- An area that is sensitive to gentle pressure within that taut band of tissue.
- The point refers to pain or sensation in another area eg: your physician gently presses on a trapezius muscle and you feel it radiating pain or sensation into the head, causing a headache.
- A twitch response in a muscle is gently pressed on a dry needle.
The visual exam to look for abnormalities of posture.
Your Physicians may order a few tests to rule out other conditions and ask you questions about your pain, including:
- Where do you feel the pain?
- How would you describe your pain?
- How often do you experience pain?
- What makes your pain better?
- What makes your pain worse?
- Have you had any recent injuries?
- Do your symptoms get well at definite times during the day?
- What does the workday look like to look for your activities in which there is muscle strain/repetitive activities or recent injuries?
- Your Physicians may check how you walk (your gait) and your posture to see if there is a balance of muscle use and look for signs of weakness in a muscle. You may also be asked about many health problems that can contribute to this syndrome including how much and how well you sleep and if you feel stressed, anxious, or depressed.
Precaution:
Persons with infectious diseases, open sores, and/or recent injuries should wait until they have recovered before starting trigger point therapy. A person taking anticoagulant prescription drugs may experience bruising after a trigger point therapy.
Can Doctor Diagnose Fibromyalgia From the Tender Points?
Your doctor can test a painful tender point during the physical exam. But you also need to tell them about the exact pain you feel in that areas. Tell them about your another symptom of fibromyalgia, too, such as deep muscle pain, fatigue, and sleep disturbances. If you have been diagnosed with irritable bowel syndrome, let the doctor know. IBS sometimes coincides with fibromyalgia.
When the doctor tests tender points for pain, they will also check another non-tender place on the body called control points to make sure you do not react to these as well. To get an official diagnosis of fibromyalgia, you must feel widespread pain for at least three months.
How Do You Treat Trigger Points and tender points?
Treatment of trigger points
Ideally, when you treat the trigger point physician are gently pressing on it just hard enough but not too hard. and you sorta have to get the feel for that. This can few times be difficult to do for yourself. You can hold the trigger points, rub them in a circular motion in either direction or work a trigger point in a back-and-forth direction. One method may provide a better result than the another on a case-by-case basis. Apply gentle pressure or rub out a trigger point for at least 10 to 15 seconds. If the pain is improving as you treat that point then continue until there is no more relief. And a few times you can feel a trigger point “wash away” beneath your fingers and disappear.
A few practitioners some tools such as wooden or metal spoon-shaped devices and other hand-held appliances and use modalities, mechanical vibration, laser therapy, electro-stimulation, dry-needling, or injection to treat a trigger point. Although some of these can be beneficial, the preference is to use the hands as much as possible – it allows you to feel the area. and you are working on, and often the dissipation or release of the trigger point can be felt. Using a hands-on approach also diminished the chances of pressing too hard and creating further bruising or damage, as well as not pressing hard enough or long enough resulting in inadequate results. If the hands are not strong enough or you are not able to reach a suspected trigger point, then tools like the foam roller, tennis ball, golf ball, Thera Cane, and/or The Stick, may be beneficial.
Various people with different levels of injury require that particular treatment. Chronic conditions are may require intense treatment over a long time to see improvement. Training is given for the maintenance of a normal posture or good posture and balancing your body mechanisms while lifting heavy objects. Regular sessions of exercise are given by the therapist, along with the encouragement of stretching and remaining daily life physical activities as well. There are many techniques of massage, such as Deep Stroking Massage which is done rhythmically in only one direction. Such massaging over the tense of the muscle strengthens muscle flexibility and endurance, along with relieving the pain.
Conservative treatments are works for most myofascial pain or trigger points. Individuals experiencing myofascial pain may be recommended for physical therapy. A few of the therapy treatments for trigger points may include soft tissue mobilization or massage and stretching. For athletes, deep tissue massages, the use of a foam roller, and stretching daily will help treat and decrease the symptoms of a trigger point. and medical Massage also can be very useful as well as acupuncture.
Methods that employ a rhythmic contraction and relaxation of the muscles are Reciprocal Inhibition, Post-Isometric Relaxation, Contract-Relax and/or Hold-Relax, etc. These physical therapy treatments maintain the joint range and allow muscles to exert their maximum power without leading to fatigue. Other specific techniques are included Myotherapy, Muscle Energy Technique, Ultrasonography, and Neuromuscular Technique.
Medications
Milder forms of pain may be relieved by nonsteroidal anti-inflammatory drugs( NSAIDs) like aspirin, ibuprofen, and naproxen. Both Tylenol (acetaminophen) and NSAIDs relieve pain caused by pain in muscle and stiffness, and additionally, NSAIDs reduce inflammation (swelling and irritation).
Trigger Point Injection (TPI)
Trigger Point Injection is a procedure of inserting a small needle into the patient’s active Trigger point. Trigger Point injection consists of local anesthetic or saline. and may include a corticosteroid. And with the injection, the trigger point is made inactive and the pain is diminished. the detailed course of treatment will result in sustained relief. The injection is performed by a physician and typically takes a few minutes. Several sites might be injected in one visit. If the patient has an allergy to a certain drug, no medications can be used in a dry needling technique. trigger point injection is in which a numbing agent or steroid is injected into the muscle knot.
Physical Therapy Management
Physiotherapy treatments may include:
Physical therapists can treat trigger points in several ways, including heat, massage, electrical stimulation, and ultrasound. They may also cover a trigger point area in a cooling spray before performing targeted stretches to relax and relieve a muscle contract.
Physical therapy involving gentle stretching and exercise may help recover the full range of motion and motor coordination. Once the trigger points are gone, muscle-strengthening exercises can begin, supporting the long-term health of the local muscle system. A physical therapist can devise a plan to help ease your pain based on your signs and symptoms. If you have the trigger point in the calf muscles, treatment is going to be more successful if you see the healthcare provider early after symptoms develop before trigger points are established. In a few chronic cases of myofascial pain, combinations of physical therapy, myofascial release therapy, trigger point injections, or massage are needed. several treatments are available and the medical professional will likely use a mixture of the following to manage the pain and regain affected muscles. Physical therapy relaxes the muscles, stretches the muscles, and strengthens the muscles. Myofascial release(MFR) techniques and trigger point therapy may be helpful for the muscle knots and the trigger points. Myofascial release is thought to help properly align the fascia surrounding the muscles. This can help improve the circulation and the normal movement of your muscles.
Trigger point therapy is performed by having the Physical therapist gently press and hold on top of the trigger points in the muscles. That temporarily cuts off circulation to the tissue. This cutting off of circulation increases a chemical called “nitric oxide in the tissue”. Nitric oxide signals a body to open up micro capillaries, thus bringing in more blood flow and breaking the pain spasm pain cycle.
- If possible, everyday-life factors that arouse the emergence of the TrPs(Trigger Point) must be eliminated or diminished,
- Postural training and education about lifestyle and postures,
- Foam Roller stretching and passive stretching, sometimes a day,
- Self-massage a few times a day, especially Deep Stroking Massage, done rhythmically and in only one direction,
- Strengthening exercises: at the start only isometric exercises and then isotonic exercises,
- Ischemic Compression Technique: In which, the term has been used to describe treatment in which ischemia is induced in the Trigger point zone by applying sustained pressure. however, this principle is questionable since a nucleus of the Trigger point intrinsically presents important hypoxia.
- This technique aims to free the contracted sarcomeres within a Trigger Point. The pressure applied should be sufficient to produce gradual relaxation of the tension within a Trigger Point zone, without causing pain. Yet both techniques show imitate significant improvement in a range of movements after treatment.
If you seek out care from your physical therapist for trigger point therapy, do not go to remove your trigger points. Rather, focus on learning strategies to help to manage your painful trigger points. and physical therapy exercises for muscle knots can help manage your pain. and help determine the underlying body mechanics that might be making muscle knots painful.
Physiotherapy helps to relieve trigger points in muscles and may involve:
- Those are two various approaches to the treatment of myofascial trigger points. There are non-invasive techniques such as Therapeutic Ultrasound, Low-level laser therapy, and TENS(Transcutaneous Electrical Nerve Stimulation).
Pain management
Low-level light therapy / cold laser
- lasers are helped to stimulate a release of pain-relieving chemicals. low-level light therapy is also known as cold laser, in which trigger points are exposed to near-infrared light
Ultrasound therapy
- Ultrasound therapy uses sound waves to raise blood circulation and warmth, which may promote healing in soft tissues affected by the trigger point in the muscles. This modality transmits sound waves into the soft tissue through a sound-conducting gel applied to the skin. The sound waves can heat up and relax your muscles, improving blood flow, and removing scar tissue. The pain-relieving effects may be minimal. But, this treatment may reduce or decrease stiffness and increase mobility if done before stretching. Pulsed ultrasound is in which a sound wave is used to penetrate muscles or soft tissues. This therapy has been successfully used for pain associated with rheumatoid arthritis, so it might be worth discussing with the doctor.
TENS(Transcutaneous electrical nerve stimulation)
- Transcutaneous electrical nerve stimulation involves sending low-voltage electric signals from the small device to a painful area through electrodes attached to your skin
Massage therapy:
- Massage: This is one type of massage that may help relieve Trigger points and is known as a manual pressure release. This type of massage technique uses the tip of the therapist’s thumb or finger to apply gentle pressure to the trigger point. This is thought to lengthen your muscles and helps relieve pain and tightness. Another type of massage is ischemic compression. the professional therapist can apply gentle pressure to your trigger points using an instrument made of wood, plastic, and rubber. This will apply direct vertical pressure on your trigger points.
There are a few types of massage techniques that can relax myofascial trigger points. These include:
- passive rhythmic release
- active rhythmic release
- shiatsu (acupressure)
- trigger point pressure release
Massage techniques or therapy improve blood flow and warm up the muscles. This can help diminish or decrease stiffness and relieve pain. your therapist applied gentle pressure on the trigger points, which will increase the pain and then release the muscle tension. your therapist may massage your affected muscle to help relieve pain. your therapist might use long hand strokes along your muscle or place pressure on specific areas of your muscle to release the tension. this therapy using trigger-point release techniques can also be effective in short-term pain relief. massage may improve the condition.
Strengthening exercise: initially only isometric exercises and then isotonic exercises.
Ischemic Compression Technique
This technique of the term has been used to describe the treatment in which ischemia is induced in a trigger point zone by applying sustained pressure. however, this principle is questionable since a nucleus of the Trigger point intrinsically presents important hypoxia. Simons described the same treatment modality, however without the need to induce additional ischemia in a trigger point zone (Trigger point Pressure Release). This technique aims to free the contracted sarcomeres within a Trigger point. The amount of pressure applied should suffice to produce gradual relaxation of tension within the Trigger point zone, without leading to pain. Yet both techniques show imitate significant improvement in the range of motion after the treatment.
Myofascial release therapy
Myofascial release therapy involves gentle fascia manipulation. Most of the myofascial release therapy treatments take place over a massage therapy session. your therapist would start stretching and massaging the areas that feel rigid along with light manual pressure. the therapist then aids tissue and/or supportive sheath in releasing tightness and pressure. The process is repeated more times on the same trigger points and another trigger point until the therapist feels the tension is fully released.

The areas where the massage therapist is working might not be near where the pain originates or where you feel the pain most prominently. Myofascial release therapy works the broader network of the muscles that might be leading to the pain. It tries to reduce tension throughout the body by releasing trigger points across a broad section of the muscular system. Myofascial release therapy could also be done at your home using a tool such as a massage gun to apply pressure to the muscles and interconnective tissues or a foam roller. This form of myofascial release can be especially useful for athletes struggling with fascial tension as a result of repetitive muscle use.
Myofascial Release therapy is a hands-on treatment performed on the skin with no creams or oils. A gentle tension between a therapist’s hands and a patient’s skin is what allows access to the fascia in a way that the gliding effect of a traditional massage cannot achieve. The myofascial release incorporates more new types of body manipulation to improve movement and function.
Trigger point release therapy
There are a few ways you can release a trigger point. The most common way is using sustained pressure with a finger, thumb, elbow, or a massage ball or some tool. The dry needling techniques are also a form of trigger point therapy that is becoming more extensive as its effectiveness is being seen.

Trigger point therapy is a therapy designed to speed up recovery from relieving the pain and the injury. This technique involves applying pressure to areas of muscle tightness or ‘knots’. This helps to decrease muscle tension and promote healing. The pressure of trigger point therapy affects a few of the nerves and muscles (specifically the neuromuscular system) so pain decreases. This encourages muscles to return to their normal state and reduces pain and tightness. and the physical therapists are well experienced in using this alongside other management strategies to assist with a wide range of conditions.
Manual therapy for Trigger Points: this typically involves sustained pressure on a trigger point until it releases. If you find nodules within a taut band of tissue hold the pressure on it until the pressure starts to diminish. This may take from thirty seconds to some minutes. If the trigger point is chronic then it may take many sessions to release this pain. You can try this would a ball to help to release the trigger point. and this is also known as ischemic pressure.
Trigger point dry needling
A trigger point dry-needling technique is one of the fastest ways to the inactive trigger point. Dry needling, in which the doctor will insert the thin needle directly into and around the trigger point, move it around, and poke it in and out. the dry needling technique involves inserting a needle into many places in and around the trigger point. It can be quite painful and helps break up muscle tension, but it is one of the most effective ways to inactivate a trigger point and reduce the pain. Acupuncture also appears to be useful for a few people who have this trigger point. a few therapists use acupuncture needles, and these needles are less painful and smaller than hypodermic needles. There are a few key differences between dry needling and acupuncture. A pushing thin needle into a trigger point decreases tightness, increases blood flow, and relieves pain. Systematic reviews concluded that dry needling for the treatment of this pain syndrome in the lower back appeared to be a helpful adjunct to standard therapy, but that clear recommendation could not be made because published studies were small and of low quality.
Trigger Point dry needling is a procedure in which a sterile, disposable, solid filament needle is inserted into the skin and a muscle directly at the myofascial trigger point. a needle is inserted into a contracted painful knot in a muscle to create a local twitch reflex which is both diagnostic and therapeutic as it is the first step in breaking the pain cycle research shows will decrease muscle contraction, decrease chemical irritation, improve flexibility and decrease pain. myofascial trigger points consist of many contraction knots, which are related to the production and maintenance of the pain cycle.
Once the main leads are established, this of course can be altered. To treat the trigger point your physical therapist has a few options. They may try some myofascial release which would involve deep tissue palpation of the trigger points to desensitize them. And Another option is to treat the areas with what is called trigger point needling. This involves putting a fine needle commonly the acupuncture needle although it is not acupuncture into a muscle to deactivate the trigger point. And an acute spasm is felt in the muscle and the release of tension follows.
You would then be shown how to stretch your muscle and this will have to be carried out regularly. Trigger point needling may be very effective in one session or may take many sessions to fully resolve the pain depending on the severity of the problem.
Stretching techniques (e.g. spray and stretch)
A physical therapist may lead you through gentle stretching exercises to assist ease the pain in your affected muscle. If you feel trigger point pain when stretching, a physiotherapist may spray a numbing solution on your skin. Stretching assists many people with a trigger point in the muscle. A few physical therapists apply a cold, numbing spray to your muscle area before leading someone through stretches. These are also some gentle stretches and exercises. you can try at your home to diminish pain.
“Stretch and spray” technique: This technique involves spraying a muscle and trigger point with a coolant and then slowly, manually stretching a muscle.
Heat: Applying heat, via a hot pack or the hot shower, can assist relieve muscle tension and reduce or diminish pain.
Cold pack
Acupuncture therapies and relaxation therapies, including cognitive behavioral therapy and biofeedback also good for improving sleep and reducing anxiety.
Posture training
Which, Improving posture can help relieve myofascial pain, particularly in the muscle of the neck. Exercises that strengthen the muscles around the trigger point will help you prevent overworking of any one muscle.
Exercises help change the posture of the body and the way the body moves.
Kinesiology taping
Many physical therapies and manual therapy techniques such as:
- Post-isometric relaxation
- Active Release Techniques
- Trigger point pressure release
- Muscle energy techniques
Other treatment options include:
- Dietary changes to reduce or decrease inflammation and avoid ingredients that seem to trigger pain.
- Heat
- Behavior modification such as posture, exercise, workstation setup, yoga, meditation, sleep habits, etc.
- Physical therapy consists of steps to realign posture, as needed
Acupuncture: Acupuncture releases the trigger points by finding the most tender point and a tight band of your muscle and using an acupuncture needle to poke the muscle and get it to involuntarily contract. Releasing your trigger point gets the muscle out of the shortened state and generally, after some contractions, it softens and remains in a more elongated and relaxed state. As an acupuncturist, you can feel the resistance at the needle soften as the trigger point and muscle is released. A Few people describe the feeling as “melting away tension and tightness ” or “popping a tension bubble.”
Treatment of the Tender Points
There are more ways to manage the pain of tender points from fibromyalgia, consist both conventional and alternative therapies. It is not clear why, but low doses of antidepressants a few times seem to ease fibromyalgia pain and fatigue. Although, the treatment for fibromyalgia and tender points involves a mix of medications, daily stress management, exercise, rest, and water exercises called hydrotherapy.
What precautions should you take?
Keep in your mind that different therapies are approaches that fall outside traditional medical practices. Talk to your doctor about these methods before trying anything, as a few of this therapy may pose a risk to your health. Also, make sure you seek services from licensed professionals to ensure that you are receiving good quality care.
Takeaway
Pain in the shoulder, back, and neck may be caused by the Trigger point trapezius muscle. These types of conditions can be treated in more ways. For example, the doctor may recommend a combination of medications, lifestyle adjustments, and alternative treatments. Be sure to discuss any potential problems that may occur from Trigger point trapezius muscle treatment with the doctor.
Home advise for trigger points and tender points
Home advice for trigger points
One of the best things person can do for the trigger points is to learn to self-manage the condition. These may consist of performing self-massage therapy trigger point techniques. These Treatments are included:
- Use a Back-Nobber to press into a trigger points
- Rolling over the tennis ball to press into the trigger points
- Foam rolling over muscles to help smooth out fascial tissue
- One thing is for certain-engaging in an active treatment program of posture correction and exercise is superior to passive treatments for trigger points. Check in with the physical therapist for a complete assessment of your condition to learn about self-care strategies to manage the trigger points.
These Treatments are also you can do at your home follow:
- Heat as in a heating pad. Some people benefit from cold/ice packs.
- Exercise particular weight-bearing exercises to help strengthen muscles, stretching exercises to stretch muscles, and aerobic exercises to get more oxygen into the muscles.
- Over-the-counter(OTC) pain killers like acetaminophen or NSAIDs like ibuprofen or naproxen. Do not take these drugs if you are taking analgesics or NSAIDs prescribed by the doctor.
- Relaxation techniques comprise yoga to stretch, decrease stress and relax the muscle, breathing exercises, and meditation.
- changes in the diet avoid foods known to lead to inflammation.
- Soaking in warm water.
- Massages.
The duration of this pain syndrome varies in individual. With treatment, it may go away after some days or/and a few weeks, but it can take longer for some. How fast this pain reduces depends on some factors, including:
- Your general health.
- Diet.
- Amount and quality of sleep.
- Take care of yourself if you have this trigger point in your muscles. Self-care measures to maintain the body healthily may make it easier for you to concentrate on coping with your pain.
Try to:
- Exercise: Gentle exercise can assist you to cope and improve with the pain. When your pain allows, get moving. Ask the doctor or the physical therapist about proper exercises.
- Relax: If you are tense and stressed you may experience increased pain. Find ways to relax. Meditating, talking with friends, and writing in a journal can all be helpful.
- Take care of your body: Eat a healthy diet of vegetables or fruits. Get enough sleep so that you wake up and/or rest. Take care of the body so that you can put your energy toward coping with pain.
Prevention of trigger point
Many of the preventable recommendations to follow are also pain management strategies:
- Maintain proper sleep hygiene.
- Reduce your stress.
- Get exercise.
- Prevent muscle injury. (this is an example of preventing muscle injury if the shoulder bag and purse you carry are too heavy).
- Practice relaxation methods.
- Eat healthy foods, like the Mediterranean diet.
Some foods cause inflammation which increases myofascial pain. Some foods to avoid include:
- Fried foods (French fries, for example).
- Dairy (milk, cheese, yogurt).
- Refined carbohydrates and the foods with refined flour such as pizza, pasta, pastries, white bread, and breakfast cereals.
- Margarine (butter), vegetable oil.
- Sugary foods and beverages like soft drinks.
- Red meat (burgers, steaks).
- Artificial sweeteners or general additives (“no sugar added” products, zero-calorie “diet” soft drinks, and processed foods that include candy, ice cream, and fruit).
- Processed meat like hot dogs, and sausage.
Home Remedies for Tender Point Pain
How you handle the fibromyalgia pain at home is another important part of your overall treatment. therapeutic massage can manipulate the muscles or soft tissues of the body to help ease pain, muscle tension, spasms, and stress. Try putting moist heat on the muscles twice a day to ease deep muscle pain and/or stiffness. You can use a moist heating pad, a warm bath, and shower, or a heat “cozy” that you warm in the microwave. It’s also important to manage your schedule or control your stress levels. Be sure to block out time each day to rest or relax. prevent making too many commitments that can wear you out. You can also try relaxation exercises like guided imagery, deep-breathing exercises, and the relaxation response to manage how you deal with stress. Also, try to go to bed at a similar time every night. It allows your body to rest or repair itself, And get regular exercise. It will assist you to manage the pain and other symptoms of fibromyalgia.
DISCLAIMER:
This article is intended or purposeful for your general informational purposes only and does not address particular circumstances. it is not a substitute for professional advice(or guidance) or help( or assistance) and should not be relied on to make decisions of any kind. A few or any actions you take upon the information presented in this article are strictly at your own risk and responsibility.
FAQ
What is trigger point tenderness?
Sensitive areas of tight muscle fibers can form in the muscles after injuries and overuse. These sensitive areas are called trigger points. A trigger point in a muscle can lead to strain and pain throughout the muscle. When this pain is continuous or persists and worsens, doctors call it myofascial pain syndrome.
Are trigger points always tender?
Instead, they can manifest on any skeletal muscle. Causes specific referred pain: Trigger points refer pain in a specific pattern to other parts of the body, but do not contribute to overall tenderness.
What happens at the trigger point?
The Trigger Point (TrP) is a hyper-irritable spot, a palpable nodule in the taut bands of the skeletal muscles’ fascia. Direct compression or/and muscle contraction can elicit jump sign, local tenderness, local twitch response, or referred pain which usually responds with a pain pattern distant from the spot.
How do you reduce the pain of a trigger point?
Injecting a numbing agent or/and a steroid into a trigger point can help relieve pain. In a few people, just the act of inserting the needle into the trigger point helps break up the muscle tension. Called dry needling, this technique comprises inserting a needle into several places in and around the trigger point.
Do tender points refer to pain?
The Tender points, by comparison, are associated with pain at the site of palpation only, are not associated with referred pain, and occur in the insertion zone of muscles, not in taut bands in the muscle belly.
Do you have tender points with fibromyalgia?
What are tender points? The official diagnostic criteria for fibromyalgia no longer require the tender point examination. But the doctor might still check for 18 tender points associated with the disorder. Tender points feel painful when only a little amount of pressure is applied.