Type 1 Diabetes
What is Type 1 Diabetes?
Type 1 diabetes is an autoimmune condition in which your body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in your pancreas.
The pancreas produces little or no insulin when this disease is present. The hormone insulin is what the body uses to let glucose, or sugar, into cells so those cells can make energy.
Type 1 diabetes can be caused by a number of variables, including some viruses and genetics. Type 1 diabetes may occur in adults even though it typically develops first in young adulthood.
There is still no cure for type 1 diabetes, after much research. In order to avoid problems, treatment involves controlling blood sugar levels using insulin, food, and lifestyle changes
Epidemiology
While it can start at any age, Type 1 Diabetes is one of the most common chronic illnesses in children. Adult-onset type 1 diabetes is more common than juvenile-onset type 1 diabetes and may be mistakenly diagnosed as type 2 diabetes.
The incidence and prevalence of type 1 diabetes, which accounts for 5% to 10% of all cases of diabetes, have been gradually rising. 9.5% of persons globally have type 1 diabetes, with an incidence of 15 cases per 100,000, according to a systematic review and meta-analysis.
Causes of Type 1 Diabetes
Diabetes type 1 may develop at any age. The most common age groups for diagnosis are young adults, teenagers, and children.
The hormone insulin is made in the pancreas by unique cells known as beta cells. The stomach is behind and under the pancreas. To transfer blood sugar, or glucose, into cells, insulin is required. Glucose is stored inside the cells and used as fuel later on. Diabetes type 1 causes little or no insulin production from beta cells.
When there is low insulin, glucose collects in the circulation in place of entering the cells. We refer to this storage of glucose in the blood as hyperglycemia. The glucose cannot be used by the body as an energy source. The symptoms of type 1 diabetes arise from this.
What specifically causes type 1 diabetes is unknown. It’s an immune system condition. This illness develops when the immune system unintentionally targets and kills healthy body tissue. When a person has type 1 diabetes, their body mistakenly targets the beta cells in their pancreas, which are responsible for producing insulin, due to an infection or other trigger. You may acquire the capacity to develop autoimmune disorders, such as type 1 diabetes, from your parents.
Symptoms of Type 1 Diabetes
High Blood Sugar
The symptoms listed below could indicate type 1 diabetes initially. Or, they could happen if your blood sugar is higher.
- Being extremely thirsty
- constantly feeling of eating food
- constantly feeling tired
- Having unclear vision
- having tingling or numbness in your feet
- Reducing body weight
- An increase in hunger
- More frequent urination (including nighttime urination or bed wetting in kids who had previously stayed dry overnight)
Low sugar blood
Hypoglycemia, or low blood sugar, can strike insulin-using diabetics very quickly. When blood sugar levels drop below 70 milligrams per deciliter (mg/dL), or 3.9 mmol/L, symptoms typically manifest.
The following symptoms are:
- Headache
- feeling of hunger
- Anxiety and irritation
- palpitations (fast heartbeat)
- trembling
- sweat
- illness
Type 1 Diabetes vs Type Diabetes 2
| Feature | Type 1 Diabetes | Type Diabetes 2 |
| Cause | Attack by the immune system on cells that produce insulin | Insufficiency or resistance to insulin |
| Onset | usually during youth or childhood | Most commonly in adulthood, but it can happen at any age |
| Symptoms | Frequently rapid and severe | Early on, it’s frequently minimal or nonexistent. |
| risk factor | It is still unclear what specifically causes type 1 diabetes. A family history of type 1 diabetes may marginally raise your risk because the disease is associated with several genes. | Risk factors for type 2 diabetes include age, race, family history, waist circumference, and being obese or overweight. |
| Possible cure | While there isn’t a solution at this moment, lifetime medication can control symptoms. Research is evaluating pancreatic islet transplantation Trusted Source, gene therapy, and stem cell-based regenerative medicine as viable therapeutic approaches. | Although there isn’t a treatment at this time, there are ways to control symptoms and delay the progression. Those with extreme obesity may experience less symptoms after a gastric bypass. |
| Prevention | Type 1 diabetes cannot currently be prevented. | Maintain a healthy diet along with regular exercise, avoid from or give up smoking, and heed medical advice if prior to diabetes is diagnosed. |
Diagnosis
The blood tests listed below are used to detect diabetes.
- Fasting blood glucose level: If it is 126 mg/dL (7 mmol/L) or more high twice, diabetes is diagnosed.
- Blood glucose level at random (non-fasting): If it is 200 mg/dL (11.1 mmol/L) or above and you experience increased thirst, urination, and tiredness, you may have diabetes. ( A fasting test needs to be performed to verify this)
- Oral glucose tolerance test: Two hours after taking a special sugar drink, a glucose level of 200 mg/dL (11.1 mmol/L) or above is indicative of diabetes.
- Hemoglobin A1C (A1C) test: If the test’s result is 6.5% or higher.
Sometimes, ketone testing is also performed. Either blood or urine is used for the ketone test. To find out if a person with type 1 diabetes has experienced ketoacidosis ketone testing may be performed. Typically, testing is carried out: - In cases where the blood sugar level is above 240 mg/dL (13.3 mmol/L),
- When suffering from a disease like pneumonia, heart attack, or stroke
When vomiting and nausea happen when you’re pregnant - The examinations and tests listed below will assist you and your healthcare practitioner in keeping an eye on your diabetes and preventing complications related to it:
- Examine your legs and feet’s skin and bones.
Inspect for diabetic nerve damage if you notice numbness in your feet. - Measure your blood pressure at least once a year.
To make sure your kidneys are functioning properly, have tests once a year. Serum creatinine and urine albumin levels are measured as part of these examinations. - After you have had type 1 diabetes for five years, see your eye doctor at least once a year, or more frequently if you show symptoms of diabetic eye disease.
- Visit the dentist for a comprehensive cleaning and examination every six months. Ensure that your dental hygienist and dentist are aware that you have diabetes.
Treatment of Type 1 Diabetes
- Those who have recently been diagnosed with type 1 diabetes may need to stay in the hospital because the disease can develop rapidly and have severe symptoms.
- If you were just diagnosed with type 1 diabetes, you might need to see a doctor once a week until your blood sugar is well under control. The outcomes of your urine test and at-home blood sugar monitoring will be discussed with your healthcare professional. Your record of meals, snacks, and insulin shots will also be examined by your healthcare professional. A few weeks may pass before the insulin dosages are adjusted to fit your food and exercise plans.
- You will need fewer follow-up appointments as your diabetes stabilizes. You must see your provider to keep an eye on any long-term complications resulting from diabetes.
- A meeting with a nutritionist, clinical pharmacist, and certified diabetes care and education specialist will probably be requested by your provider. These professionals will assist you in controlling your diabetes as well.
- Still, you are the one who has to manage your diabetes the most. The fundamentals of managing diabetes should be familiar to you. These include:
- How hypoglycemia, or low blood sugar, is diagnosed and treated
- How to identify and manage hyperglycemia (high blood sugar)
- How to organize meals, including the calculation of carbohydrates
- How insulin is administered
- How to measure urine ketones and blood sugar
- Adjusting insulin and diet during physical activity
- How to manage days off for illness
Where to get supplies for diabetes and how to store them
Insulin
By allowing glucose to enter cells instead of the bloodstream, insulin reduces blood sugar. For those who have type 1 diabetes, insulin must be taken daily.
Insulin is often delivered through the skin using an insulin pump, pen, or syringe. Inhaled insulin is another kind of drug. Because insulin is destroyed by stomach acid, it cannot be given orally.
The duration and rate of activity of different insulin types change. The most suitable kind of insulin for you will be selected by your doctor, who will also advise you on when to take it. For the best blood glucose management, some insulin types may be combined in an injection. Insulin of different kinds should never be combined.
The majority of persons with type 1 diabetes require two different forms of insulin. Long-acting basal insulin regulates the amount of sugar your body produces when you’re not eating. Every mealtime insulin shot, also known as bolus insulin, has a quick onset of action.
Its duration is limited to assisting in the transfer of meal-absorbed sugar into muscle and fat cells for future storage.
You will learn how to inject insulin from your healthcare professional or a diabetes educator. A parent or other adult may initially administer an injection to a youngster. Most kids can administer their injections by the time they are 14 years old.
Insulin that is inhaled is a powder that is breathed in. It works quickly and is taken right before meals. If you are suitable for this form of insulin, your supplier can advise you.
Individuals with diabetes must understand how to adjust their insulin dosage:
- When they exercise
- When they’re ill
- When will they consume more or fewer calories and food?
- When they’re on the road
You can find out which foods and activities most effectively raise or lower your blood sugar by doing a blood sugar test. It helps regulate your insulin dosage in response to particular meals or activities so that your blood sugar doesn’t rise or fall too much.
Healthy foods and activities
Plans for preparing nutritious, well-balanced meals can be found at the American Diabetes Association and the Academy of Nutrition and Dietetics. Speaking with a certified nutritionist or nutrition counselor is also beneficial.
Frequent physical activity benefits blood sugar regulation. It is also helpful in the burning of extra fat and calories to achieve and maintain a healthy weight.
Before starting any exercise, talk with your Physician or Physical Therapist. Individuals who have type 1 diabetes need to take extra precautions before, during, and following exercise or physical activity.
Managing your blood sugar
You can find out how effectively you are controlling your diabetes by measuring your blood sugar yourself and recording the findings. For how often to check, speak with your diabetes educator and provider.
A glucose meter is a tool used to measure blood sugar levels. Typically, a lancet—a tiny needle—is used to pierce your finger to gather a tiny drop of blood. You fill a test strip with blood, then insert the strip into the meter. The meter provides you with a reading that indicates your blood sugar level.
Your blood sugar level is measured by a continuous glucose monitor using a fluid that is under your skin. While many individuals of these monitors also use insulin pumps to manage their diabetes, those who do not use an insulin pump can find them to be useful as well. Most monitors don’t need you to prick your finger.
Both you and your medical team should have a record of your blood sugar levels. Using a website made specifically for this reason can frequently make this process the easiest. If you are having trouble controlling your diabetes, these data will be helpful. Your blood sugar level should have a target goal that you and your healthcare professional agree upon at different times of the day.
Discuss your goal for the A1C test with your healthcare physician. Your average blood sugar level over the last three months is displayed by this lab test. It indicates how effectively you are managing your diabetes. The A1C goal for the majority of individuals with type 1 diabetes should be 7% or less.
We refer to low blood sugar as hypoglycemia. It is dangerous to have blood sugar levels below 70 mg/dL (3.9 mmol/L). If the blood sugar is less than 54 mg/dL (3.0 mmol/L), prompt action is required. Low blood sugar can be avoided with proper blood sugar management. If you have any questions relating to the signs and causes of low blood sugar, see your healthcare professional.
Foot care
Foot problems are more common in those with diabetes than in those without the disease. Nerve damage is caused by diabetes. Your feet may become less sensitive to pressure, discomfort, heat, and cold as a result. A foot injury could go unnoticed until there is significant harm to the skin and tissue just below or until you develop a serious infection.
Blood vessels can also be harmed by diabetes. Deeper skin sores (ulcers) can develop from minor skin fractures or sores. If these skin ulcers do not heal or if they get deeper, bigger, or infected, the affected limb could have to be amputated.
To avoid foot issues:
- If you use tobacco, give it up.
- Boost your blood sugar regulation.
- Find out if you have nerve damage by having your feet examined by your physician at least twice a year.
- Request that your healthcare professional examine your feet for issues like calluses, hammertoes, or bunions. Treating them is necessary to stop skin damage and ulceration.
- Examine and take care of your feet each day.
If you already have foot issues or damage to your blood vessels or nerves, this is important. - Athlete’s foot and other mild infections should be treated promptly.
- Taking good care of your nails is essential. You should have your nails cut by a podiatrist or other healthcare professional who is aware of your diabetes if your nails are extremely thick and hard.
On dry skin, use a lotion moisturizer. - Make sure you’re wearing suitable shoes. Find out from your provider which type is best for you.
Complications
To lower your risk of experiencing typical diabetic problems, your doctor may recommend the following medications or other treatments:
- eye conditions
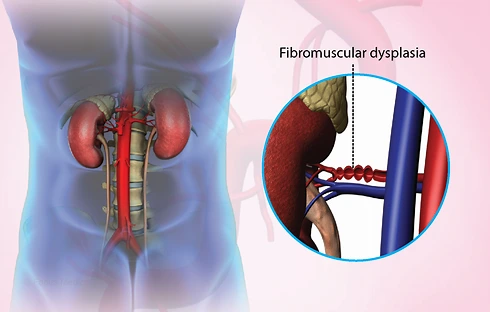
- renal illness
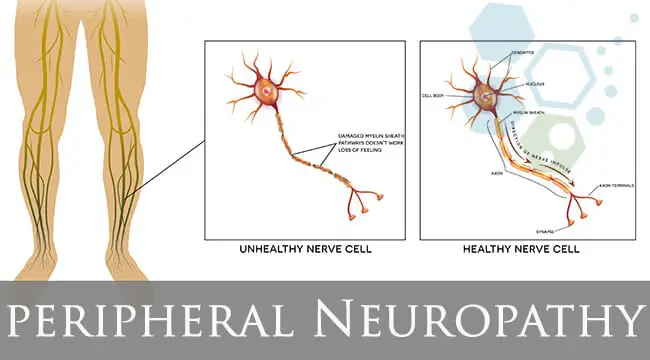
- Damage to peripheral nerves
- Heart problems and strokes
- You run the risk of getting type 1 diabetes along with other diseases like gum disease, bone disease, hearing loss, and yeast infections in women. You can help avoid these symptoms by maintaining adequate blood sugar management.
- Persons who have diabetes should make sure they receive their vaccinations on time.
Differential Diagnosis
- Type 2 diabetes mellitus
- Diabetes in the pancreas
- False sickness
- Diabetes caused by steroids
- Glycosuria renal
- psychological polydipsia
- Insipidus diabetes
Prognosis
Improved management of blood pressure, glucose, lipids, and foot care has reduced the morbidity and death related to type 1 diabetes. There are fewer major complications associated with diabetes; if they do exist, many have postponed their beginning. Death rates are down even though those with type 1 diabetes have a 2- to 5-fold higher mortality than those without diabetes.
Patients education
Preventing problems largely depends on patient medication compliance and follow-up with educators and specialists. The pharmacist, nurse, and other healthcare professionals should stress the importance of managing long-term problems, controlling blood glucose, and setting goals for management at every patient visit.
Encouragement to alter lifestyle should be given to the patient to lower the chance of problems. In addition, it is important to educate all diabetic patients about the warning signs and symptoms of hypoglycemia as well as how to treat it. Patients must be informed about the resources that are out there as well as the advantages of joining support groups. The patient should be taught by a nurse how to check their blood sugar at home and by a dietician about foods they can eat.
Results of Healthcare Teams
The major burden of self-managing type 1 diabetes involves numerous daily insulin administration, glucose monitoring, and daily attention to dietary and physical exercise. While people’s glycemic control has improved thanks to modern technologies, these systems are expensive, and complicated, and call for training and education.
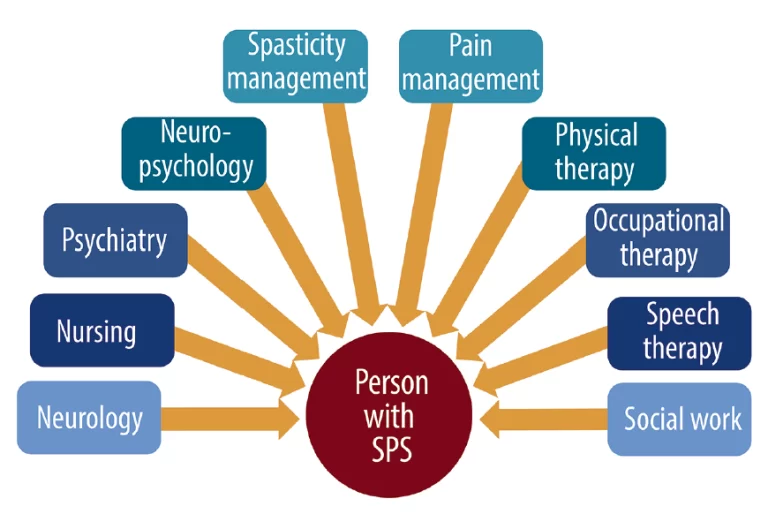
Many diabetics worry about hypo- or hyperglycemia, complications, and the potential for eating disorders, anxiety, and depression. An interprofessional team comprising clinicians (MDs, DOs, NPs, and PAs), nurses (including diabetes nurse educators), pharmacists, dieticians, mental health professionals, social workers, podiatrists, and the use of community resources are best suited to address the medical, educational, training, psychological, and social challenges that people with type 1 diabetes face daily customized methods and results of treatment.
The interprofessional care model will result in the best possible patient outcome, and individualized treatment options are required to reduce the burden and further improve outcomes.
All interprofessional team members must coordinate their activities and interventions with the rest of the team and utilize open communication channels to ensure everyone involved in patient care, as well get access to the same precise, up-to-date patient data as the patient. In addition to participating in patient monitoring, teaching, and assessment, nurses are frequently essential in arranging the efforts of other medical experts involved in the case.
It is recommended that pharmacists collaborate closely with diabetes educators to guarantee appropriate insulin doses and take part in patient medication reconciliation and education. Better patient outcomes will result from these interprofessional care instances.
FAQ
What is type 1 diabetes caused by?
It is believed that an autoimmune reaction—in which the body unknowingly goals itself—is the origin of type 1 diabetes. The beta cells in the pancreas, which produce insulin, are destroyed by this process. It may take months or even years for any symptoms to show up during this process.
Can type 1 diabetes live a normal life?
Type 1 diabetes currently has no known treatment. Even so, research is producing significant improvements, new technology and medications are being created, and our understanding of the illness is continually changing. People with type 1 diabetes are currently living full, strong lives across all age groups.
When does type 1 diabetes start?
Type 1 diabetes may occur to anyone at any age, even though it’s frequently found in children. If your sibling, sister, father, or mother has type 1 diabetes, then your risk of developing the disease is somewhat increased. The primary treatment for type 1 diabetes is insulin. Insulin pumps and injections are necessary for survival.
Does type 1 diabetes require insulin?
Those with type 1 diabetes have very little or no insulin produced by the pancreas. Because of this, insulin is necessary for all individuals with type 1 diabetes. An injection of insulin or a continuous insulin pump administration takes place under the skin.
Is diabetes type 1 permanent?
While type 1 diabetes is a lifelong condition, you may manage and live with it. Communicating with your medical team is essential for maintaining your health while you have diabetes. At least every three to six months, have your doctor check your A1c levels and test your blood sugar at home.
How is type 1 diabetes being treated these days?
The Food and Drug Administration (FDA) authorized Lantidra, the first allogeneic pancreatic islet cellular therapy produced from deceased donor pancreatic cells, in June 2023 as a novel treatment for type 1 diabetes.
References
- Type 1 diabetes: MedlinePlus Medical Encyclopedia. (n.d.). https://medlineplus.gov/ency/article/000305.htm
- Lucier, J. (2023, March 3). Type 1 Diabetes. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK507713/
- G. J. (n.d.). Differences between type 1 and type 2 diabetes. Diabetes UK. https://www.diabetes.org.uk/diabetes-the-basics/differences-between-type-1-and-type-2-diabetes
- Nichols, H. (2023, December 18). What are the differences between type 1 and type 2 diabetes? https://www.medicalnewstoday.com/articles/7504
- Type 1 diabetes – Symptoms and causes – Mayo Clinic. (2023, September 15). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/type-1-diabetes/symptoms-causes/syc-20353011



9 Comments