Understanding Cancer Treatment Options
Introduction
There is a vast array of cancer therapies available for the many forms of cancer, with a unique therapy needed for each type of cancer.
Surgery, chemotherapy, radiation therapy, hormone therapy, targeted therapy (using monoclonal antibodies or small-molecule pharmaceuticals), and PARP inhibitors (like olaparib) are some of the available treatment options.
Stem-cell therapy, photodynamic therapy, immunotherapy, and hyperthermia are other treatments. The most typical course of cancer treatment involves many distinct medicines, such as chemotherapy, followed by surgery.
Occasionally, angiogenesis inhibitors are employed to augment the outcomes of immunotherapies. The location, grade, and stage of the tumor, together with the patient’s overall health, all influence the therapeutic option.
The most effective treatment for a certain cancer type can be identified with the use of biomarker testing. Numerous cancer experimental therapies are always being developed.
One in five individuals will receive a cancer diagnosis at some point in their lives, according to estimates made in 2023. The main objectives of cancer treatment are to either significantly extend the patient’s life or cure the cancer by eliminating it entirely.
When the cancer is considered terminal and the prognosis is bad, palliative care becomes necessary. Cancer comes in a variety of forms, and if caught in time, many of them may be effectively treated.
Types of Treatments
As our knowledge of the underlying biological processes has grown, so too have the approaches to treating cancer. Surgery to remove tumors was used as early as ancient Egypt, and in the late 1800s, radiation and hormone treatment were established.
The 20th century gave rise to modern targeted medicines, immunotherapy, and chemotherapy. Treatments will be created and adjusted in response to new insights into the biology of cancer in order to improve efficacy, precision, survival, and quality of life.
Surgery
Surgery can heal malignant tumors if they are completely eliminated. However, it is typically not possible to completely remove the cancer surgically if it has already spread (metastasized) to other locations.
According to the Halstedian model, cancer begins locally, progresses to the lymph nodes, and finally spreads throughout the body.
Due to this, locally only therapies like surgery for tiny malignancies have become more and more common. It is becoming more well-acknowledged that even little localized cancers have the ability to spread.
A prostatectomy for prostate cancer, a mastectomy and lumpectomy for breast cancer, and lung cancer surgery for non-small cell lung cancer are a few examples of surgical operations for cancer.
Surgery may be performed with the intention of removing the tumor in its entirety, the organ in part, or both. The process of a single cancer cell growing into a new tumor is known as recurrence, even though it is undetectable to the unaided eye.
To reduce the possibility that the patient still has tiny cancer cells, the pathologist will review the surgical material to see if a margin of healthy tissue is there.
Surgery is frequently required for staging, which includes removing the main tumor and figuring out whether the illness has spread to nearby lymph nodes. A significant factor in determining prognosis and the necessity of adjuvant treatment is staging.
Sometimes symptoms like spinal cord compression or intestinal blockage require surgery to manage. We call this kind of care palliative care. Surgery can be done either before or after receiving other medical care.
Neoadjuvant therapy is frequently used to denote preoperative care. individuals with breast cancer who get neoadjuvant chemotherapy have a survival rate that is comparable to that of individuals receiving treatment after surgery.
Chemotherapy administered early enables cancer doctors to assess the therapeutic efficacy and may facilitate tumor resection. Less is known about the benefits of neoadjuvant therapy for lung cancer survival.
Radiation Therapy
Ionizing radiation is used in radiation treatment, also known as radiotherapy, to cause cellular death in cancer cells and reduce tumor size by destroying their DNA.
Radiation therapy has two possible effects on DNA: it can directly damage DNA or produce free radicals, which are charged particles that enter cells and destroy DNA. Brachytherapy is an inside method of administering radiation therapy, external beam radiotherapy is another option.
Radiation treatment has localized effects that are limited to the area being medicated. While radiation harms both healthy cells and cancerous cells, most healthy cells are able to overcome the effects of radiation and resume their regular functions.
Radiation therapy aims to destroy as many cancer cells as possible while causing the least amount of damage to adjacent healthy tissue.
Because of this, it is administered in many portions, enabling healthy tissue to regenerate in between. Almost all solid tumor types may be treated with radiation treatment, which can also be used to treat lymphoma and leukemia.
The radiosensitivity of each form of cancer and the presence of surrounding tissues and organs that might be harmed by radiation are two important considerations that determine the radiation dose to each location.
Radiation therapy has adverse effects, just like any other type of treatment. Due to radiation exposure to the salivary glands, radiation treatment may cause dry mouth, which lowers saliva production.
Salivary gland function will usually return after therapy, but not always in the same way. Radiation-induced dry mouth might become a lifelong issue.
If the tumor was discovered in an inaccessible area or at a late stage, radiation may not be the best course of action because of the increased risk of organ damage from radiation at therapeutic dosages.
Furthermore, radiation therapy for kids less than 14 years old may result in very serious long-term adverse effects that affect their lifestyle, such as blindness and hearing loss.
Children who have had cranial radiation therapy are considered to be more vulnerable to both cognitive delay and scholastic failure.
Chemotherapy
Chemotherapy is the use of medications (sometimes known as “anticancer drugs”) to treat cancer and kill cancer cells. Chemotherapy can be administered via injection into the vein, artery, muscle, or skin. It can also be taken orally.
Nowadays, unlike targeted therapy, the word “chemotherapy” mainly refers to cytotoxic chemicals that generally attack rapidly proliferating cells.
Chemotherapy medication can obstruct cell division in a number of ways, such as by preventing DNA duplication or chromosomal separation.
Although some degree of selectivity may exist, the majority of chemotherapy treatments target all rapidly dividing cells and are not only directed toward cancer cells. originate from the fact that normal cells can usually repair DNA damage, while many cancer cells cannot.
Chemotherapy thus has the potential to damage healthy tissue, particularly the gut lining and other tissues with a rapid rate of renewal.
After chemotherapy, these cells often heal themselves. Drugs that interact better with one another than they do separately are sometimes administered in combination.
“Combination chemotherapy” is what this is known as; most chemotherapy regimens are administered in combination.
Chemotherapy can have a wide range of adverse effects since it affects every part of the body. Due to the fact that the medications used to treat cancer also target the cells in the hair roots, patients frequently experience hair loss.
Depending on the patient, this potent medication may also cause vomiting, lethargy, and exhaustion.
Some leukemias and lymphomas require total body irradiation (TBI) and high-dose chemotherapy for treatment.
The bone marrow is ablated by this therapy, which impairs the body’s capacity to heal and replenish its blood supply.
To allow for “rescue” following the administration of medication, bone marrow or peripheral blood stem cell collection is done prior to the ablative phase of the therapy. We call this autologous.
Targeted Therapies
Since its introduction in the late 1990s, targeted therapy has significantly improved the prognosis for several cancers and is still an active field of study. This is the application of drugs that are particular to the dysregulated proteins seen in cancerous cells.
Targeted treatment medications known as small molecules often function as enzymatic domain inhibitors on proteins that are mutant, overexpressed, or otherwise essential to the cancer cell.
The tyrosine kinase inhibitors gefitinib (Iressa) and imatinib (Gleevec/Glivec) are two notable examples.
Another tactic is monoclonal antibody treatment, in which an antibody is used as the therapeutic agent and it attaches precisely to a protein on the surface of cancer cells.
Examples include the anti-CD20 antibody rituximab, which is used in a range of B-cell malignancies, and the anti-HER2/neu antibody trastuzumab (Herceptin), which is used in breast cancer.
Small peptides known as “homing devices” in targeted treatment may potentially attach to cell surface receptors or the extracellular matrix around the tumor.
If radionuclides that are linked to these peptides (such as RGDs) decay close to the cancer cell, the cancer cell will finally perish. These binding motifs are particularly interesting as oligo- or multimers as they may increase tumor avidity and selectivity.
A ternary cancer treatment called photodynamic therapy (PDT) combines light, tissue oxygen, and a photosensitizer.
PDT is a viable therapy option for lung cancer and basal cell carcinoma (BCC). It can also be employed to eliminate any remaining malignant tissue following the surgical excision of large tumors.
Medical researchers revealed in February 2019 that iridium might bind to albumin to form a photosensitized protein that can enter cancer cells and, when exposed to light, kill the cancer cells.
Compared to conventional target cancer therapy, high-energy therapeutic ultrasound may enhance the higher-density anti-cancer medication load and nanomedicines to target tumor locations by a factor of 20.
As potential cancer treatments, targeted therapies under pre-clinical development include NF-κB inhibitors in chemotherapy-resistant models.
Multitargeted kinase inhibitors inhibit PI3K along with other pathways like MEK and PIM, and morpholino splice switching oligonucleotides that induce ERG exon skipping in prostate cancer models.
Immunotherapy
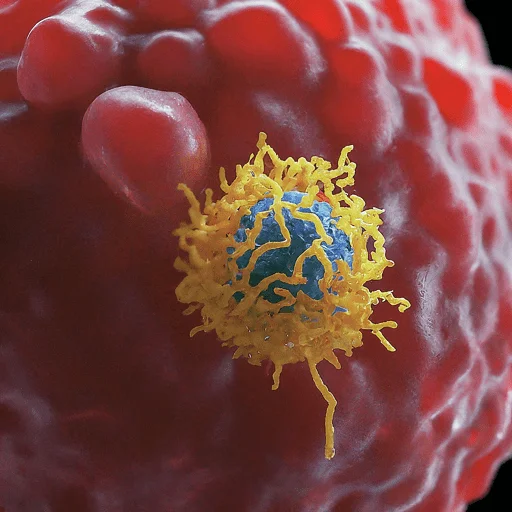
The term “cancer immunotherapy” describes a broad range of treatment approaches intended to activate the patient’s immune system against the tumor.
Intravesical BCG immunotherapy for superficial bladder cancer and the use of interferons and other cytokines to stimulate an immune response in patients with renal cell carcinoma and melanoma are examples of modern strategies for mounting an immune response against cancers.
Extensive research is being conducted on cancer vaccines to elicit particular immune responses against various malignancies, including renal cell carcinoma and malignant melanoma.
In order to trigger a particular immune response against prostate-derived cells, prostatic acid phosphatase peptides are loaded onto the patient’s dendritic cells as part of the Sipuleucel-T prostate cancer vaccination approach.
In 2010, the FDA approved it. Immunotherapy can be used for allogeneic hematopoietic stem cell transplantation (typically from bone marrow) from a genetically different donor since the donor’s immune cells frequently target the tumor in a process known as the graft-versus-tumor effect.
Because of this, allogeneic hematopoietic stem cell therapy (HSCT) has a better cure rate for many cancer types than autologous transplantation; nevertheless, the adverse effects are also more severe.
In Japan, patients’ own natural killer cells (NKs) and cytotoxic T cells are employed in cell-based immunotherapy, which has been around since 1990. The main agents that destroy cancer cells at the onset of development are NK cells and TCs.
This therapy is known as autologous immune enhancement therapy (AIET) and is administered in addition to other forms of treatment such as radiation, chemotherapy, or surgery.
The two immunological checkpoint proteins that are the focus of immune checkpoint treatment are programmed cell death protein 1 (PD-1) and cytotoxic T-lymphocyte-associated protein 4 (CTLA-4).
Checkpoint proteins function as negative feedback mechanisms that the immune system uses to help the body return to equilibrium once infections have been eliminated.
Cancer cells are able to take control of this physiological regulatory mechanism in a tumor microenvironment in order to “put a brake” on the immune response against cancer and avoid immune surveillance.
Dr. James Allison of the University of Texas MD Anderson Cancer Center in the United States and Dr. Tasuku Honjo of Kyoto University in Japan have been awarded the 2018 Nobel Prize in Medicine for their contributions to the development of PD-1 and CTLA-4 immune checkpoint treatment.
Hormonal Therapy
Certain hormones can be supplied or blocked to slow the growth of various tumors. Certain forms of prostate and breast cancer are frequent instances of hormone-sensitive malignancies. Blocking testosterone or estrogen is frequently a crucial adjunctive therapy.
Hormone agonists, including progestogens, can be used therapeutically for certain malignancies. Patients may get adverse effects such as hot flashes, nausea, and weariness after hormone treatment, however, these vary depending on the kind.
Angiogenesis Inhibitors
Angiogenesis inhibitors stop the massive blood vessel expansion (angiogenesis) that cancers require to proliferate and endure. As a cell grows, it can invade nearby tissues and spread to distant areas through metastasis.
Angiogenesis inhibitors with multiple approvals include cabozantinib, axitinib, and bevacizumab. Although none of the flavonoids have been tested in human clinical trials, it has been demonstrated that they inhibit the angiogenic activation of VEGF and Hypoxia-inducible factor (HIF).
Exercise Prescription
Based on research showing that exercise (as opposed to no exercise) is related to lower recurrence rates, improved mortality outcomes, and a decrease in adverse effects from conventional cancer therapies, exercise prescription is increasingly being used as an adjuvant treatment for cancer.
The benefit-risk ratio of including exercise in cancer treatment is high, despite the uncertainty surrounding the correlation or causation of improved outcomes with exercise.
Exercise has additional benefits (such as cardiovascular and mental health) without major risks, though there is a small risk of overuse injury if added too aggressively.
When it comes to prescribing exercise for cancer patients, exercise physiologists and exercise medicine experts can help oncologists and primary care physicians.
Synthetic Lethality
Cell death results from a combination of deficits in the expression of two or more genes, but not from a deficiency in any one of these genes alone. We call this phenomenon “synthetic lethality.”
Deficits may result from one or both of the genes being inhibited, from mutations, or from epigenetic changes. A DNA repair gene is commonly lacking in cancer cells (also see DNA repair deficit in cancer).
Either a mutation or, more frequently, epigenetic silencing may be the cause of this DNA repair deficiency.
Synthetic lethality may be used to kill tumor cells if the DNA repair deficiency is in one of the seven DNA repair routes (see DNA repair pathways) and a compensatory DNA repair pathway is suppressed. Non-tumorous cells can live as long as the original route is unbroken.
Ovarian Cancer
DNA repair gene PARP1 (which is involved in base excision repair and microhomology-mediated end-joining pathways of DNA repair) is synthetically deadly when mutated in BRCA1 or BRCA2 (active in homologous recombinational repair).
About 18% of women with ovarian malignancies have a mutational defect in BRCA1 (13% have germline mutations and 5% have somatic mutations; see BRCA1).
The US FDA authorized olaparib, a PARP inhibitor, in 2014 for the treatment of ovarian cancer linked to BRCA that has undergone chemotherapy before.
In 2016, the FDA authorized rucaparib, a PARP inhibitor, for the treatment of advanced ovarian cancer in women with a BRCA1 or BRCA2 gene mutation and who have received at least two rounds of chemotherapy.
Colon Cancer
When TOP1 is deactivated in colon cancer, epigenetic abnormalities in the WRN gene seem to be synthetically fatal. Specifically, in patients with colon cancer, irinotecan inactivation of TOP1 was synthetically fatal with reduced expression of the DNA repair WRN gene.
In a 2006 research, WRN protein expression was high in 45 patients colonic cancers with hypermethylated WRN gene promoters, which suppressed WRN expression. Whereas WRN protein expression was high in 43 patients’ tumors with unmethylated WRN gene promoters.
Compared to patients with unmethylated WRN promoters (20.7 months survival), those with hypermethylated WRN promoters (39.4 months survival) benefited better from irinotecan. About 38% of colorectal tumors had hypermethylated WRN gene promoters.
Colon cancer can occur in five phases, each of which has a treatment plan:
- According to the American Cancer Society, stage 0 refers to the need for surgery to remove the polyp.
- In Stage 1, the patient has surgery similar to that of Stage 0, depending on where the cancer is located in the colon and lymph nodes.
- Patients in stage 2 have surrounding lymph nodes removed, but if the cancer is more likely to return, the patient may also need to receive chemotherapy following surgery, depending on the doctor’s advice.
- In stage three, the cancer has completely taken over the lymph nodes but has not yet reached any other organs or body parts. Once the colon and lymph nodes reach this stage, the doctor performs surgery and prescribes chemotherapy (FOLFOX or CapeOx) to treat the colon cancer where it is needed (American Cancer Society). Stage 4 is the last that a patient may receive.
- Surgery is only performed on stage 4 individuals in order to relieve their discomfort and avoid malignancy. The doctor may suggest radiation therapy if none of these two remedies relieve the discomfort. Because of how aggressively the cancer spreads at this stage, not just to the colon but also to the lymph nodes, chemotherapy is the primary therapeutic approach.
Symptom Control and Palliative Care
Controlling cancer symptoms is crucial for improving the quality of life for individuals with the disease and for determining whether they may receive additional therapies, even though it is not commonly considered a cancer treatment.
Physicians are often skilled in treating discomfort, including nausea and vomiting brought on by chemotherapy, diarrhea, bleeding, and other frequent issues that affect cancer patients.
Palliative care is a multidisciplinary specialty that has grown in response to the demands of various patient categories with regard to symptom control. Painkillers that inhibit nausea and vomiting include morphine, oxycodone, and antiemetics.
Patients with symptoms associated with cancer frequently utilize them. More effective antiemetics like aprepitant and its analogs, ondansetron, have greatly increased the viability of aggressive therapies for cancer patients.
Pain from cancer may be linked to ongoing tissue damage brought on by the illness itself or by treatments (such as radiation, chemotherapy, or surgery).
Environmental influences and emotional disorders can always play a part in the development of pain behaviors, although they are often not the main causative elements in cancer patients’ pain.
Palliative therapy should always be employed to manage pain, even in circumstances when patients with severe cancer-related pain are reaching the end of their lives.
Concerns include things like health care utilization and the social stigma associated with taking opioids. It might need to be taken care of in order for the patient to feel comfortable taking the drugs needed to manage their symptoms.
Getting the patient as comfortable as possible with the fewest amount of pharmaceuticals is the usual approach to managing pain in cancer patients, even if it involves the use of opioids, surgery, and physical measures.
In the past, doctors were hesitant to administer opioids to patients with terminal cancer because of the risk of addiction and suppression of respiratory function.
Preemptive pain management for cancer patients is now more widely supported because of the palliative care movement, a more recent offshoot of the hospice movement.
The World Health Organization also identified unmanaged cancer pain as a global issue and developed a “ladder” to provide guidelines for healthcare professionals on how to manage cancer patients’ pain.
One of the most prevalent symptoms of cancer is weariness associated with the disease, and several strategies have been proposed to address this.
Mental Struggles/Pain
Mental strain is one of the numerous challenges faced by cancer sufferers. Cancer patients frequently experience anxiety, overwhelm, uncertainty, and even depression. Chemotherapy is an extremely aggressive treatment that kills bodily cells.
Such physical side effects not only hurt the patients but also wear them out emotionally and make them want to quit.
Hospitals provide a variety of therapeutic options and mental health services for several reasons, Among them are spiritual concepts, yoga, meditation, and counseling. All of these are intended to ease mental tension and provide hope to patients who might be feeling depleted.
Insomnia
People who have survived cancer treatments frequently suffer from sleeplessness. Insomnia affects around 60% of cancer survivors, and if left untreated, it can have long-term consequences for one’s physical and physiological well-being.
Dissatisfaction with the length or quality of sleep combined with trouble falling asleep or staying asleep is known as insomnia. Lack of sleep may significantly lower one’s quality of life. For cancer survivors, cognitive behavioral therapy has been shown to lessen sadness and sleeplessness.
Muscle Strength
One major adverse effect of several cancer therapies is decreased muscular strength. Exercise is therefore crucial, particularly during the first year following medication. Research has demonstrated that yoga, pilates, and water exercise can enhance the mental health and overall well-being of those who have survived breast cancer.
Hospice care
Hospice care offers palliative care for a person with an advanced disease that is considered terminal, either at home or at a facility specifically designed for hospice care.
When cancer is left untreated, it can become fatal, and people may decide to forgo therapy and all of its horrible side effects in favor of hospice care. Support for a patient’s medical, emotional, social, practical, psychological, and spiritual needs is the goal of hospice care.
When a person nears the end of their life, advance care planning (ACP) can assist them in making decisions about their own future medical care.
ACP assists individuals in whatever state of health to make decisions about their medical treatment choices and future desires, ideally after first discussing them with family members or caregivers.
Research
Research studies, often known as clinical trials, evaluate novel therapies for cancer patients. Developing more effective cancer treatments and supporting cancer patients is the aim of this study.
Numerous therapeutic modalities, including novel medications, innovative surgical or radiation therapy techniques, novel treatment combinations, and novel gene therapy techniques, are tested in clinical trials.
One of the last phases of a protracted and meticulous cancer research procedure is a clinical study. Scientists initially create and test novel ideas in the laboratory, where the quest for new medicines starts.
The next stage, if a strategy looks viable, may be to test medication on animals to observe how it affects cancer in a living organism and whether it has any negative consequences. Naturally, therapies that are effective in a lab or on animals may not necessarily be effective in humans.
Research involving cancer patients is conducted to determine the safety and efficacy of potential therapies. Participating patients may benefit directly from the care they get.
They receive the most effective standard cancer therapy or a novel treatment that is currently undergoing testing, and they receive cutting-edge care from cancer specialists.
However, research participants who get a novel therapy may be among the first to benefit if it turns out to be as successful as or more effective than normal care. On the other hand, new medicines may also come with unknown hazards.
There is ensure that a traditional treatment or a novel treatment under testing will yield positive outcomes.
An analysis of trial participation in children with cancer revealed that, on average, trial participants did not do any better or worse than those receiving normal care.
This finding supports the idea that it is impossible to anticipate whether an experimental treatment would be successful or not.
Exosome Research
Exosomes are lipid-coated microvesicles that are secreted into physiological fluids like urine and blood by solid tumors. Currently, studies are being conducted in an effort to employ exosomes as a means of cancer monitoring and diagnosis.
The goal is to identify particular exosomes in the blood or urine in order to diagnose cancer with high sensitivity and specificity. It is also possible to more precisely track a patient’s progress during therapy by using the same procedure.
It has been demonstrated that the enzyme-linked lectin-specific assay, or ELLSA Archived on 13 July 2011 at the Wayback Machine, can directly identify exosomes produced by melanoma from fluid samples.
In the past, the total protein content of purified samples and indirect immunomodulatory effects were used to quantify exosomes.
ELLSA has the ability to quantify exosome particles in complicated solutions directly and has been discovered to be able to identify exosomes from ovarian cancer and macrophages infected with TB, among other sources.
Exosomes are thought to be released by tumors and are implicated in the development of angiogenesis, metastasis spread, and immune cell programmed cell death.
They are also thought to disrupt T-cell signaling, which is necessary for mounting an immune response, and prevent the synthesis of anti-cancer cytokines.
“Lectin affinity plasmapheresis” (LAP) is a blood filtering technique that targets tumor-based exosomes specifically and removes them from circulation.
LAP is currently being studied. Reducing the amount of exosomes released by the tumor in the patient’s circulation is thought to both boost the patient’s immune system and reduce the cancer’s growth.
Complementary and Alternative
The broad category of medical and healthcare systems, procedures, and goods that are not a part of traditional medicine and have not been proven to be successful is known as complementary and alternative medicine (CAM).
“Alternative medicine” refers to substances used in place of traditional medicine, whereas “complementary medicine” refers to techniques and medications used in addition to it.
People who have cancer frequently utilize complementary and alternative medicine (CAM); according to a 2000 survey, 69% of cancer patients had used at least one CAM therapy throughout their cancer treatment.
The majority of complementary and alternative cancer treatments have not undergone extensive research or testing. Certain complementary therapies that have been studied and shown to be ineffectual are still being sold and advertised.
Special Circumstances
In Pregnancy
The average age of expectant women has increased the risk of cancer linked to pregnancy. Cancers may also be unintentionally discovered while screening mothers.
The choice of cancer therapy must take into account the least amount of damage to the patient’s embryo or fetus. A therapeutic abortion could be advised in specific circumstances.
Chemotherapy always carries the danger of miscarriage and congenital abnormalities, and radiation therapy is not an option.
Medication side effects on children are not well understood. Certain cancer types can damage the placenta and cause the medicine to cross it even if it has been shown in testing to not cross it to reach the kid.
Certain types of skin cancer can also spread to other parts of the child’s body. The fact that computed tomography is unfeasible due to its large radiation exposure further complicates diagnosis. Magnetic resonance imaging continues to function correctly.
Contrast materials, however, cannot be employed since they pass through the placenta, due to the challenges in accurately diagnosing and treating cancer during pregnancy.
The other options are to either perform an abortion in order to treat cancer if it is sufficiently malignant that the mother is unlikely to be able to wait that long or perform a Cesarean section when the child is viable in order to start more aggressive cancer treatment.
In utero
Sometimes prenatal diagnosis is made for fetal tumors. The most prevalent kind of prenatal tumor is teratoma, which is often benign. Sometimes, while the fetus is still within the uterus, they are surgically addressed.
Society and Culture
Racial and Social Disparities
One major problem that the globe is facing is cancer. By the end of 2018, it is anticipated that there will be 609,640 cancer-related fatalities and 1,735,350 new cases in the United States.
Many cancer fatalities may be avoided with adequate therapy, but high mortality rates are mostly due to racial and social inequities in treatment. White patients are more likely to obtain effective treatments on schedule, whereas minority patients are more likely to receive subpar care.
Receiving appropriate care in a timely manner can improve a patient’s chances of survival. It has been demonstrated that white patients had far higher survival rates than African American patients.
Between 1992 and 2000, there were 27 and 18.5 deaths on average per 100,000 white patients and 35.4 and 25.3 deaths per 100,000 black patients from colorectal cancer.
Conflicting results were reported in a publication that examined many research examining racial differences in colorectal cancer treatment.
There was insufficient data, according to the Veterans Administration and an adjuvant study, to justify treating colorectal cancer differently based on race.
Nonetheless, compared to white patients, two investigations revealed that African American patients received less pleasant and subpar care. The Center for Intramural Research expressly provided funding for one of these projects.
In comparison to white patients, they discovered that black patients had a 41% lower chance of receiving colorectal therapy and a higher likelihood of being admitted to a teaching hospital with fewer board-certified specialists.
In addition, black individuals had a higher likelihood of receiving a diagnosis of oncologic sequelae—a serious condition brought on by maltreated cancer.
Finally, there were 95.6 fatalities among White patients and 137.4 deaths among Black patients for every 1,000 patients in the hospital. The differences in breast cancer therapies in the Appalachian Mountains were examined in a scientific paper on the disease.
It was discovered that African American women had two times the mortality risk as white women and three times the risk as Asian women. This study indicates that African American women had a worse chance of surviving than women of other races.
In addition, black women are more likely than white women to forego surgery or counseling, which can result in less effective care.
In addition, a panel from the National Cancer Institute concluded that the breast cancer therapies provided to African American women were insufficient and unsuitable in comparison to those provided to Caucasian women.
Based on these investigations, scientists have concluded that there are differences in cancer therapy, particularly in terms of who can afford and obtain the finest care. Eventually, this causes differences in the number of cancer patients dying and the number of survivors.
African Americans often have lower access to cancer facilities, insurance, and medical coverage than other racial groups, which is the root cause of these discrepancies.
For instance, compared to patients of other races, black patients with breast cancer and colorectal cancer were shown to have a higher likelihood of receiving Medicaid or having no insurance.
The fact that African Americans receive less treatment than other racial groups can also be attributed to the location of the medical institution.
However, according to some research, African Americans don’t always seek the necessary assistance because they don’t trust doctors, which is why The number of African Americans obtaining treatment has decreased.
Some claim that because African Americans don’t have as many resources as white people, they ask for even more care than white people. In this instance, examining this research will reveal the treatment inequalities and attempt to prevent them by figuring out what could be causing them.
Public Perception
Even if there have been advances in results, people may find it difficult to manage their visceral fear of the illness. Patients with lung cancer frequently experience prejudice, social exclusion, embarrassment, and stigma.
It is occasionally said to these sufferers that their smoking caused their cancer. These patients could also feel guilty about having cancer. The main causes of stigma surrounding cervical cancer were self-blame, shame, and fear of social rejection.
Gender and social norms also had a significant negative impact on the stigma surrounding cervical cancer, as both human papillomavirus infection and cervical cancer were associated with the belief that they are the result of risky behavior, such as having multiple sexual partners.
partners or failing to do the screening. One effective defense against stigmatization could be resilience.
In the context of cancer therapy, resilience refers to the ability of the patient to successfully adapt, recuperate, and continue to perform at their best despite medical obstacles on a physiological and psychological level.
It includes the capacity to deal with hardship, come out on top of it, preserve emotional stability, and advance general well-being and recovery.
FAQ
Can cancer be cured?
The kind and stage of a person’s cancer, the kind of treatment they may get, and other variables all affect their chances of being cured. There is a difference in the likelihood of curing some tumors. However, the course of treatment for each malignancy must vary.
Can Stage 4 cancer be cured?
While there is typically no cure for stage 4 cancer, therapy can increase overall survival and quality of life. The type of cancer, how well it reacts to treatment, the patient’s general health, and a number of other factors all have a significant role in treatment choices and survival rates for stage 4 cancer.
Is Stage 1 cancer Curable?
It is also possible to cure stage 1 cancer, particularly if detected early on. Your chances of treating cancer before it becomes worse increase with early detection. Cancer is a cruel illness that causes alterations in the body’s normal, healthy cells.
Can cancer be 100% cured?
It is said by doctors to be in remission. On the other hand, cancer can recur years after going into remission. To cure cancer would be to eradicate it entirely and ensure that it does not recur. There is presently no known cure for cancer, despite the fact that this may occur for certain individuals.
Which cancer is not curable?
Cancer that is incurable and finally ends in death is referred to as terminal cancer. It may be referred to as end-stage cancer by others. When a physician declares a patient’s cancer to be terminal, it typically indicates that the disease has progressed to the point that available treatments are intended to manage rather than cure the illness.
Which cancer kills the fastest?
Why it’s critical to treat pancreatic cancer more quickly. Pancreatic cancer has continued to be the least curable and fastest-killing malignancy for far too long. Within a month, 1 in 4 pancreatic cancer patients pass away; this number quickly rises to 3 in 4 deaths within a year. This can be the result of delayed medical attention.
Is cancer Genetic?
This explains why cancer seems to run in families at times. Hereditary genetic alterations may be the cause of up to 10% of all cancer cases. It is not a guarantee that you will develop cancer if you inherit a gene linked to cancer. It implies that you have a higher chance of developing cancer.





6 Comments