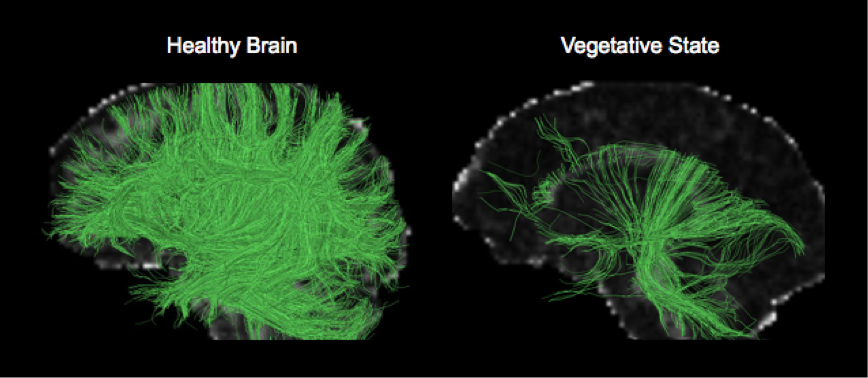
Vegetative State
What is Vegetative State?
The vegetative state is also called unresponsive wakefulness syndrome. This is separate from a coma, in which the person is fully unconscious. A vegetative state is a condition of consciousness or altered consciousness. A vegetative state happens when the cerebrum (the region of the brain that regulates thought and behavior) no longer roles, but the hypothalamus and brain stem (the regions of the brain that regulate vital functions, like body temperature, sleep cycles, and blood pressure, breathing, heart rate, and consciousness) continue to function. Therefore, patients open their eyes and seem awake but otherwise accomplish not react to stimulation in any meaningful manner.
Patient in a vegetative state can open their eyes, but they cannot say or do things that need review or conscious intention, and they have no awareness of themselves or their atmosphere. The vegetative state is irregular.
A vegetative state that stays for more than 1 month is considered a persistent vegetative state. Most patients with a persistent vegetative state do not heal any mental role or capability to interact with the atmosphere in a meaningful manner. Yet, a few patients with a persistent vegetative state enhances adequately that the diagnosis is altered to a minimally conscious condition. In a patient in a minimally conscious state, awareness is hard but not fully harmed.
When any recovery happens, the cause was generally brain injury due to a head injury (traumatic brain injury), not a disease that resulted in the brain is denied oxygen. Furthermore, healing is usually very little. For instance, a patient may come for any things or may utter the exact word over and over. Infrequently, patients in a persistent vegetative state due to head damage continue to gradually enhance over months to years.
How many patients are in a vegetative state is unfamiliar, but approximately 25,000 grown-ups and almost 10,000 kids in the United States are believed to have this disease
What can cause this state?
Acute brain damage due to disease or injury generates an unaware and unresponsive condition.
Nontraumatic brain injury
This kind of brain injury can happen when the brain is deprived of oxygen, or brain tissue is injured. Some causes for this contain:
- drug overdose
- encephalitis
- heart attack
- meningitis
- near drowning
- poisoning
- ruptured aneurysm
- smoke inhalation
- stroke
Traumatic brain injury (TBI)
This kind of brain injury is the outcome of injury you might obtain from a strong blow to the head due to a:
- car accident
- fall from a great height
- workplace or athletic accident
- assault
Progressive brain damage
This brain injury may be due to circumstances like:
- Alzheimer’s disease
- brain tumor
- Parkinsons disease
What are the symptoms?
A patient in an unaware and unresponsive condition has felt an injury to the brain. They have no cognitive role or capability to think. But since their brain stem is still working, the patient may:
- control breathing and heart rate without assistance
- open their eyes
- have a sleep-wake cycle
- have basic reflexes
- move their eyes, blink, or tear up
- moan, grunt, or appear to smile
They’re not able to:
- track things with their eyes
- respond to voices or verbal orders
- speak or communicate via blinking or gesturing
- move with goal
- interact with their surroundings
- show signs of emotion
- show signs of awareness
This unaware and unresponsive state varies from these matching states:
Minimally conscious state. The patient rotates between awareness and lack of awareness.
Coma. The patient is not awake or aware.
Brain death. Harm to the brain and brain stem is categorically irreversible.
Locked-in syndrome. The patient is aware and completely aware but completely paralyzed and incapable to speak.
Diagnosis of Vegetative State
A doctor’s evaluation
Tests like magnetic resonance imaging and electroencephalography
Doctors or physicians guess a vegetative state based on symptoms. Yet, before a vegetative state can be analyzed, the patient should be kept for some time and on more than one event. If patients are not kept long enough, proof of awareness may be skipped. Patients who have some awareness may be in a minimally aware state instead than a vegetative state.
An imaging test, like magnetic resonance imaging (MRI) or computed tomography (CT), is accomplished to inspect for diseases that may be causing the issue, particularly those that can be ministered. If the diagnosis is in doubt, doctors or physicians may accomplish further imaging examinations through positron emission tomography (PET) or single-photon emission computed tomography (SPECT). These examinations can show how well the brain is working.
Electroencephalography (EEG) may be accomplished to inspect for irregularities in the brain’s electrical movement that indicate seizures, which may damage consciousness.
Functional MRI (fMRI) may be accomplished to study brain movement and thus decide whether awareness is fully impaired. This examination can see when a patient replies to questions and commands, even when the reaction is not apparent that is when the patient does not speak or move in reaction (covert consciousness). EEG can also see this brain movement. The outcomes of these examinations can involve decisions regarding long-term care.
Treatment of Vegetative State
Preventive steps for issues due to immobilization
Good nutrition
Music treatment may have slight useful effects by stimulating a reaction in a patient in a vegetative state or other kinds of impaired consciousness. But the benefit of this treatment is as yet unclear.
There’s no real cure. Instead, the fixation is confirming care so the brain can recover. The patient will be carefully observed for modifications or signs of progress.
In addition, doctors or physicians will take actions to control potential complications, like:
infection
pneumonia
respiratory failure
Supportive care may include:
- a feeding tube to deliver nutrients
- changing positions regularly to avoid pressure sores
- physical treatment to gently exercise the joints
- skincare
- oral care
- management of bowel and bladder functions
Various experts may include family members in trying to encourage the senses and producing a response by:
speaking to them regarding things they’re familiar with
playing music, TV, or favorite movies
displaying family photos
adding favorite perfumes, flowers, or further scents to the room
maintaining or stroking their hand or arm
Therapy will start in an acute care hospital environment. In some circumstances, the patient may be transitioned to a nursing home or a further long-term maintenance facility.
Physiotherapy treatment
With bed-ridden people, per day immobilized in bed can raise the possibilities of additional complications including various body systems, from musculoskeletal problems to pulmonary issues. Therefore earlier mobility is very necessary. Prolonged bedridden persons are prone to contractures, muscle atrophy, degenerative joint disease, disused osteoporosis, bed sores, and breathing problems. The stamina decreases especially due to no motion.
Chest Therapy
It is very necessary for persons that are more probable to develop lung infection (more senior people, people that have already been in bed for a prolonged period, smokers, and people that will likely have to remain in bed for a long time). Request a physiotherapist for daily routines of Chest therapy, which will assist to control respiratory issues.
Positioning
Positioning suggests putting the person in a fine position. The family should forever hold in mind that any position if it is held for too long, will lead to difficulties (like bedsores and muscle contracture). That is why, actually if a position, for some exact reason, is suitable for a person, the position has to be altered every two hours.
Passive mobilization
Passive mobilization purpose to prevent muscle retraction and reduction of range of motion – ROM as well as further difficulties like bedsores and blood circulation issues.Some activity:
Neck exercises
Head turns: Rotate the patient’s head to one side then to the further side.
Head tilts: Tilt the patient head, getting the ear toward the one shoulder then further
Chin-to-chest: Slightly bow the patient head toward his or her chest.
Shoulder and elbow exercises
Shoulder movement: Lift the patient’s arm ahead and then up over his or her head and back down
Elbow bends: Put the patient’s arm at his or her side with the palm meeting up. Twist and straighten the arm.
Arm and wrist exercises
Wrist bends: Flex the patient hand back toward his or her shoulder. The fingers should tell toward the roof.
Wrist rotation: Slightly move the patient hand in rotations in one direction.
Palm up, palm down: Bend his or her hand so the palm meets up with the roof, and then turn the palm down
Hand and finger exercises
Finger bends: Bend the fingers into a fist. Lengthen the fingers too, then Bend and straighten per finger
Finger spreads: Outstretch the thumb and first finger separated, then obtain them back jointly.
Finger rotations: Move per finger in a ring in one order then in a further direction.
Hip and knee exercises
Hip and knee bend: Gradually flex the patient’s knee up as close to his or her chest as likely. Then slightly straighten the leg.
Leg movement, side to side: Move one leg getaway to the side, out from the further leg.
Leg rotation, in and out: Roll one of the patient’s legs toward the further leg then move the leg to another side
Ankle and foot exercises
For the toe activities, allow the patient’s foot to calm on the bed, and maintain only the toes
Ankle bends: Flex the patient foot so the toes indicate toward the roof and backward
Ankle rotation: Lift the patient’s foot barely off the bed. Move the foot in rings.
The toe bends: Bend the patient’s toes down toward the sole, Then lengthen them again.
Toe spreads: Extend the big toe and the second toe separated, then obtain them back jointly
Long-term care
Like a patient in a coma, a patient in a vegetative state needs comprehensive care.
Supplying good nutrition (nutritional help) is necessary. Patients are fed via a tube inserted via the nose and into the stomach (known as tube feeding). Occasionally they are fed via a tube inserted straight into the stomach or small intestine via an incision in the abdomen. Medicines may also be given via these tubes.
Many issues result from being incapable to move (immobilization), and actions to control them are important (see Issues Due to Bed Rest). For instance, the following can occur:
Pressures sores: Lying in one position can trim off the blood supply to some regions of the body, generating skin to crack down and pressure sores to start.
Contractures: Lack of motion can also conduct to endless stiffening and shortening of muscles (contractures) generating joints to evolve permanently bent.
Blood clots: Lack of motion causes blood clots more probable to form in leg veins known as deep vein thrombosis.
Pressure sores can be controlled by repeatedly repositioning the patient and putting defensive padding under regions of the body that are in touch with the bed, like the heels, to rescue them.
To control contractures, physical therapists slightly move the patient’s joints in all orders (passive range-of-motion activities) or splint joints in particular positions.
Preventing blood clots contains the use of medications and compression or elevation of the patient’s legs. Moving the limbs, as happens in passive range-of-motion activities, may also assist to control blood clots.
Because patients are incontinent, maintenance should be carried out to hold the skin clean and dry. If the bladder is not working and urine is being maintained, a tube (catheter) may be put in the bladder to drain urine. Catheters are carefully washed and regularly inspected to control urinary tract infections from forming.
Other issues
If healing is unlikely, family members, doctors, and occasionally the hospital ethics board should examine how aggressively future medical issues should be followed and when and if life-sustaining therapy should be removed. A patient’s wishes about like therapies should be evaluated if they are known for instance if wishes have been stated in an advance directive (living will).
Decisions for family members
A patient with this neurological condition can persist for decades, but the most patient will only stay for a few years. As a family member, you may have to make many necessary judgments about their care, like:
seeing the right nursing home or facility
attending to the financial elements of long-term care
creating life-support findings including feeding tubes, ventilators, and further measures used to support a patient alive
deciding whether to mark a accomplish not resuscitate (DNR) so no lifesaving steps will be accepted if the patient stops breathing
These are complex findings that should include an in-depth conversation with the doctors or physician include.
If the [atient has no living will or medical control of attorney, it may be useful to confer with an attorney regarding your requests and responsibilities.
The prognosis for Vegetative State
Some patient spontaneously heals from a vegetative state, but healing is generally incomplete. The possibilities of healing rely on the reason and time of the brain harm and the patient’s age, for the next:
Some healing is more probable if the reason is a head injury, a reversible metabolic abnormality (like low blood sugar), or a medication overdose instead of a significant stroke or cardiac arrest.
A younger patient may heal more use of their muscles than a more senior patient, but dissimilarities in the healing of behavior, mental function, and speech are not essential.
If a vegetative state stays for more than a few months, patients are unlikely to heal consciousness. If patients do heal, they are probable to be severely disabled.
Any healing from a vegetative state is doubtful after 1 month if the cause was anything further than head damage. If the reason was a head injury, healing is doubtful after 12 months. Yet, a few patients enhance over months or years. Infrequently, progress happens late. After 5 years, approximately 3% of patient heal the capability to communicate and understand, but few can live independently, and none can function commonly.
Most patient who stays in a vegetative state dies within 6 months of the original brain injury. Most of the another live approximately 2 to 5 years. The reason for death is usually a respiratory or urinary tract infection or extreme malfunction (failure) of several organs. But death may happen unexpectedly, and the reason may be unknown. A few peoples live for several years.
There have been accounts of a patient recovering some awareness after expending years in what seems to be a vegetative state or coma. These statements frequently affect a patient who had been in a minimally conscious state, generally after a head injury. The possibilities of healing from a minimally conscious condition are unexpected but more useful than those from a vegetative state.
FAQ
Can you recover from a vegetative state?
Some patients heal from a vegetative state, but it is generally not a full recovery. The brain injury will probably result in permanent disabilities. Healing is most possible if the reason for the vegetative state is an injury or a reversible disease like low blood sugar or a medication overdose.
Is vegetative state brain death?
Brain death varies from a vegetative state
A person in a vegetative state still has a functional brain stem, which suggests: some state of consciousness may live. breathing alone is generally feasible. there’s a slim possibility of healing because the brain stem’s core works may be uninvolved.
Is the vegetative state temporary?
Recovery from a vegetative state is doubtful after 1 month if a brain injury is nontraumatic and after 12 months if a brain injury is traumatic. If some healing happens after these intervals, most peoples are severely disabled.
What is the dissimilarity between a vegetative state and a coma?
The word coma generally guides to the condition in which a patient seems to be asleep but cannot be awakened. Persistent vegetative state guides to another state of altered consciousness in which the patient seems to be awake but does not react meaningfully to the outside globe.
Do people in vegetative states have brain activity?
No single area was associated with the possibility of recovering consciousness that is, the brain does not have a consciousness center. But general metabolism did show a contrast. Vegetative persons had, on average, 38 percent of the brain movement that fit people did.