Physiotherapy Treatment of Hemiplegia
What is a Hemiplegia?
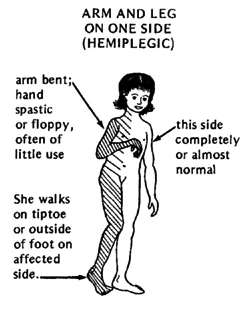
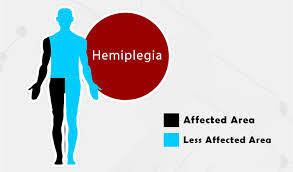
Hemiplegia is a neurological condition in which paralysis or weakness on one side of the body. The term “hemiplegia” is derived from the Greek words “hemi” (meaning half) and “plegia” (meaning paralysis). It can affect either the right or left side of the body, and the paralysis or weakness typically extends from the arm and leg to the face and may vary in severity.
Hemiplegia is often caused by damage to the motor cortex or the pathways that control movement on one side of the brain. Brain damage can result from various conditions such as Stroke.
Definition of Hemiplegia
- Hemiplegia means complete paralysis of half of the body. Hemiparesis is unilateral paresis, that is, weakness of the entire left or right side of the body.
- Hemiplegia and hemiparesis can be caused by different medical conditions, such as congenital causes, trauma, tumors, or stroke.
- Hemiplegia is caused by damage to the central nervous system (brain and spinal cord): the execution orders of movements are not transmitted to the muscles. In addition to motor problems, other functions can be altered as memory or sensitivity.
Signs and Symptoms of Hemiplegia
- Pain. There is pain associated with brain injury and localized pain in the affected limbs.
- Aphasia. People who suffer from hemiplegia, even though the process of thinking and developing ideas is held, are struggling to find words and articulate. In addition, they may have difficulty understanding the meaning of words they hear or read them.
- Disorders of the sphincters. A quarter of people with hemiplegia have sphincter disturbances resulting in either urinary incontinence or urinary retention, fecal incontinence is still.
- Sexual dysfunction: erection, ejaculation is compromised in many men with hemiplegia. Moreover, a decreased libido, especially at the beginning of the disability, is often found.
- In some cases, the lesions, arm, and leg are affected, in others only the arm or only the face.
- Loss of motor skills.
- Pusher syndrome.
- Difficulty with gait.
- Difficulty with balance while standing or walking.
- Having difficulty with motor activities like holding, grasping or pinching
- Increasing stiffness of muscles.
- Muscle spasms.
- The majority of children who develop hemiplegia also have abnormal mental development.
- Behavior problems like anxiety, anger, irritability, lack of concentration or comprehension.
- Emotions — depression.
- Shoulder pain — Often associated with a loss of external rotation of the glenohumeral joint, commonly due to the increased tone of the Subscapularis muscle and Pectoralis major muscle.
- Shoulder Subluxation.
- Difficulty in swallowing.
- Trouble with vision. Blurred vision or weakness of the eyes. Speech becomes difficult. Numbness, tingling, or loss of sensations on one half of the body.
- Heightened emotional sensitivity with inability to handle stressful situations.
- Memory seems poor. Unable to recall recent or past events concerning people, places and activities.
- Loss of control over bladder and bowel movements leading to an inability to hold on to stool or urine.
Causes of Hemiplegia
- The most common cause of hemiplegia is stroke. Strokes can cause a variety of movement disorders, depending on the location and severity of the lesion.
- Hemiplegia is common when the stroke affects the corticospinal tract. Other causes of hemiplegia include spinal cord injury, specifically Brown-Séquard syndrome, traumatic brain injury, or disease affecting the brain. As a lesion that results in hemiplegia occurs in the brain or spinal cord, hemiplegic muscles display features of the Upper Motor Neuron Syndrome.
- Features other than weakness include decreased movement control, clonus (a series of involuntary rapid muscle contractions), spasticity, exaggerated deep tendon reflexes and decreased endurance.
- Other causes of hemiplegia in adults include trauma, bleeding, brain infections and cancers. Individuals who have uncontrolled diabetes, hypertension or those who smoke have a higher chance of developing a stroke.
- Weakness on one side of the face may occur and may be due to a viral infection, stroke or a cancer.
- The stroke may be caused by: A clot formed within the blood vessel blocking the blood supply’-> a thrombusA thrombus breaks away from its site of origin and forms a block elsewhere in the circulation. -> an emboliA bleed from a blood vessel supplying the brain -> a hemorrhage
Common causes are
- Head injury
- Diabetes
- Brain tumor
- Migraine syndrome -> recurrent headaches of severe intensity occasionally accompanied by sensations of numbness and tingling in one half of the body.
- Inflammation of the blood vessels -> vasculitis
- Diseases affecting the nerves -> like Multiple Sclerosis; acute necrotizing myelitis.
- Vascular: cerebral hemorrhage, stroke, diabetic neuropathy.
- Infective: encephalitis, meningitis, brain abscess.
- Neoplastic: glioma-meningioma.
- Demyelination: disseminated sclerosis, lesions to the internal capsule.
- Traumatic: cerebral lacerations, subdural hematoma rare cause of hemiplegia is due to local anaesthetic injections given intra-arterially rapidly, instead of given in a nerve branch.
- Congenital: cerebral palsy.Lack of blood supply damages nerve cells in the brain. Birth trauma, difficult labor, perinatal strokes in infants within 3 days of birth can all cause cerebral palsy.
- Disseminated: multiple sclerosis.
- Psychological: parasomnia (nocturnal hemiplegia).
- Hereditary diseases: leukodystrophies. This is a rare disorder affecting the myelin sheath which covers and protects nerve cells in the brain. The condition usually appears in infancy or childhood.
Pathophysiology
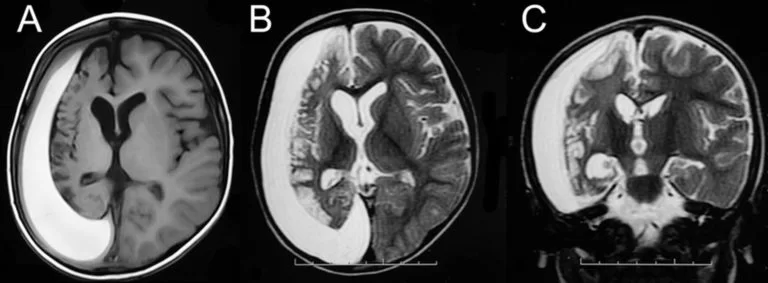
- The exact cause of hemiplegia is not known in all cases, but it appears that the brain is deprived of oxygen and this results in the death of neurons. When the corticospinal tract is damaged, the injury is usually manifested on the opposite side of the body.
- For example if one has an injury to the right side of the brain, the hemiplegia will be on the left side of the body. This happens because the motor fibres of corticospinal tract ( also called pyramidal fibres), which take origin from the motor cortex in brain, cross to the opposite side in the lower part of medulla oblangata and then descend down in spinal cord to supply their respective muscles. Depending on the site of lesion in brain, the severity of hemiplegia varies.
- A lesion in internal capsule where all the motor fibres are condensed in a small area, will cause dense hemiplegia i.e. complete loss of power of all muscles of one half of body while a lesion at cortical or subcortical level will cause varied amount of weakness of one half of the body.
Diagnosis
- Complete blood count.
- Blood biochemistry test.
- Cranial CT: a highly detailed, non-invasive, imaging procedure that combines x-rays with computer technology and allows the study of the brain from many angles.
- Cranial MRI: a non-invasive, highly sensitive procedure that uses electromagnetic properties of tissues providing detailed studies of their structures.
- An EEG (electroencephalogram): can measure the nerve activity within the brain.
PREVENTION:
- Hemiplegia caused by cerebral palsy is non-progressive and doesn’t deteriorate with aging. But, conditions like Alternating Hemiplegia can have serious consequences as the child has repeated attacks. Here are a few tips to prevent these recurring attacks.
- With time, it is understood that these attacks of hemiplegia have definite triggers. Exposures to high as well as cold temperatures, emotional stresses, physical fatigue, bathing, infections especially of the respiratory system etc. are know triggers of Alternating Hemiplegia. Finding the specific triggers and avoiding them can help in preventing the long-term sequelae that usually develop.
- Flunarizine, a calcium channel blocker, has been used widely, although it rarely stops episodes completely. However, it does seem to reduce the severity of episodes and how long they last. Some reports also suggest that the episodes happen less often.
Treatment of Hemiplegia
- Hemiplegia usually takes a while to recover. There are two facets in treating the condition.
- Check further progress of underlying condition Rehabilitation and control of disability.
- Hemiplegia is often non-progressive and many available measures make coping with it less stressful to the person affected as well as caregivers.
- Neuromuscular Electrical Stimulation (NMES): High-intensity electrical stimulation is a proven way to maintain size – and even function – in muscles that must temporarily take a complete break from activity.
- The right kinds of electrical stimulation can keep muscles relatively sound, even when they are not being stimulated by the nerves or engaging in any real activity.
Botulinum Toxin injections: Some forms of hemiplegia make the limb muscles very taut and resistant even to passive movements. Botulinum injections decrease the high muscle tone of these muscles. However, it is only a temporary and expensive solution to a chronic condition.
Intensive physiotherapy sessions: Activities like standing, walking are done repetitively under the guidance of trainers to prevent muscle degeneration from prolonged under use.
In Alternating Hemiplegia, the child may require admission in the intensive care unit (ICU) especially if there are any respiratory infections or breathlessness. Low doses of ibuprofen (pain-killer) will help in minimizing muscle pains after an acute attack. Sound sleep is known to decrease the severity of the attacks. Hence, one must ensure that the child gets a sufficient amount of sleep.
Physiotherapy Treatment of Hemiplegia
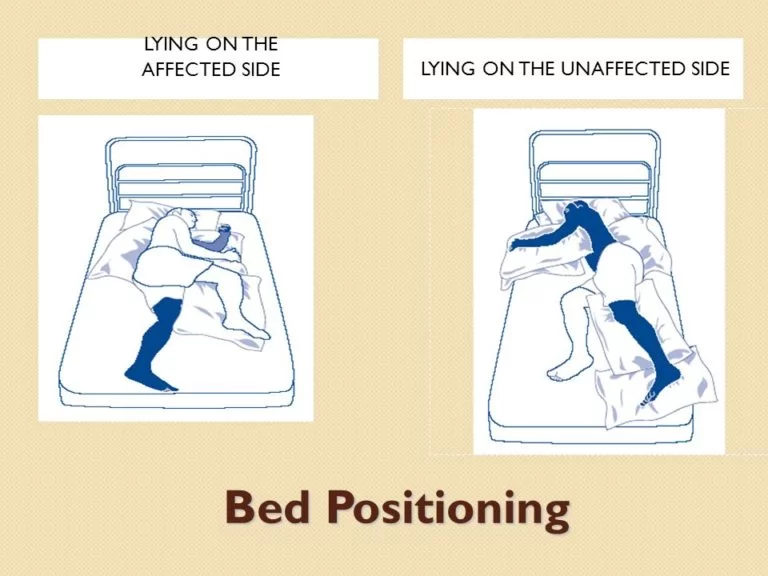
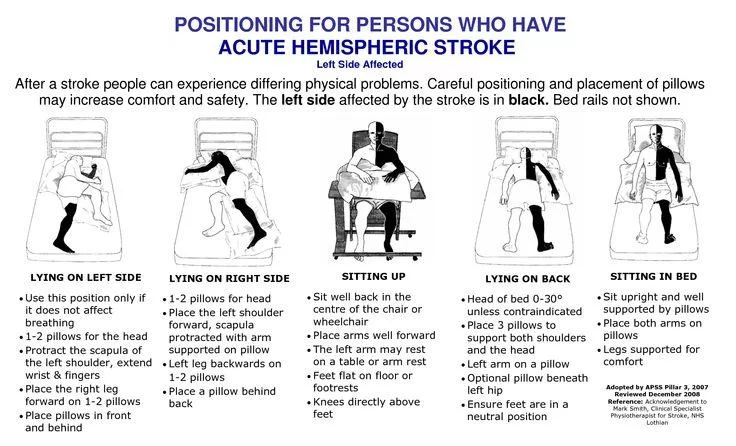
LYING ON AFFECTED SIDE:
- One or two pillows for head.
- Affected shoulderpositioned comfortably.
- Place unaffected legforward on one or two pillows.
- Place pillows in front or behind to give support.
LYING ON UNAFFECTED SIDE:
- One or two pillow for head.
- Affected arm forward and supported on pillow(s)
- Affected leg backwards on one or two pillows.
- Place pillow behind.
SITTING IN BED:
- Sitting in bed is desidable for short periods only.
- Must be upright and well supported with pillows.
- Giving extra support using pillows under arms or knees.
LYING ON BACK:
- Keep three pillows in a ‘triangle’, supporting shoulders and head.
- Keep affected arm on pillow.
- Ensure feet in a neutral position.
LOOSEN UP YOUR NECK MUSCLE:
- Slowly look over your right shoulder then your left shoulder.
- Touch your right ear to your right shoulder, then your left ear to your left shoulder. (Do not raise your shoulder, bend your neck.)
- Bend your head forward to bring your chin to your chest, then lift your head back to an upright position.
LOOSEN UP THE MUSCLES AROUND YOUR SHOULDER BLADE:
- Sit at the table with your elbows and forearms resting on the table, your elbows bent and your hands out in front of you. Make sure that neither the chair nor table has wheels.
- Without moving your arms on the table, bring your chest toward the table while sitting up straight and tall. Then move your chest away from the table and slouch. Continue this sequence.
- Rest both hands on a towel on the table. Move your hands straight out in front of you straightening your elbows completely and leaning forward slightly. Bring your hands back in towards your chest and return to sitting up straight. Repeat this sequence. Repeat the same motions, sliding your arms slightly to the right. Repeat the same motions, sliding your arms slightly to the left.
- Rest both hands on a towel on the table. Slide your hands forward until both elbows are straight. Now slowly slide your hands from side to side, going only as far to the side as the width of your shoulders.
Rest both hands on a towel on the table. Make a small circle on the table surface with your hands sliding the towel. Make the circle as wide as your shoulders.
RANGE OF MOTION EXERCISES FOR ELBOW, SHOULDER AND WRIST:
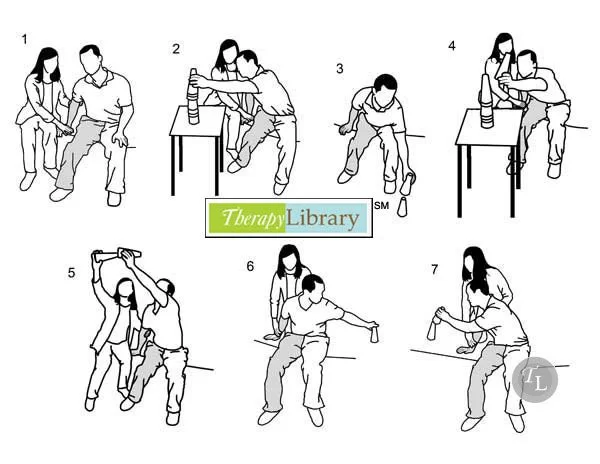
- Put your affected hand in your non affected hand. Move your arms forward to straighten your elbows,keeping your hands at shoulder or chest level. Return both hands to your chest. Repeat.
- With your elbows straight and your hands together, raise your hands to shoulder or eye level. Repeat.
- Keeping your elbows straight, reach towards the floor with your arms between your knees. Repeat over your right knee, then over your left knee.
- Sit with your hands together on the same knee. Bring the back of your right hand to your right knee, then the back of your left hand to your left knee, keeping your hands together. Repeat.
- With your hands still together, bring your hands to your left shoulder by bending your elbows, then to your right knee by straightening your elbow. Then reverse and bring your hands to your right shoulder, then your left knee. Repeat
- With your forearms resting on the table, thumbs up, bend your wrists to the left and then to the right.
With your forearm resting on the table, gently bend your fingers into your palm, and then straighten your fingers. - Holding the base of your thumb, gently rotate your thumb in a complete circle.
IMPROVING MOTOR CONTROL:
Neurofacilitatory Techniques:
Bobath
- Berta & Karel Bobath’s approach focuses to control responses from damaged postural reflex mechanism. Emphasis is placed on affected inputs facilitation and normal movement patterns
Rood
- Emphasise the use of activities in developmental sequences, sensation stimulation and muscle work classification. Cutaneous stimuli such as icing, tapping and brushing are employed to facilitate activities.
Proprioceptive neuromuscular facilitation (PNF)
- Developed by Knott and Voss, they advocated the use of peripheral inputs as stretch and resisted movement to reinforce existing motor response.
- Total patterns of movement are used in treatment and are followed in a developmental sequence. It was shown that the commutative effect of PNF is beneficial to stroke patient.
- Comparing the effectiveness of PNF, Bobath approach and traditional exercise, demonstrated that no one approach is superior to the rest of the others.
Learning theory approach:
Conductive education-
- In Hemiplegia Physical Therapy, Conductive education is one of the methods in treating neurological conditions including hemiplegic patients.
Motor relearning theory-
- Carr & Shepherd, both are Australian physiotherapists, developed this approach in 1980. It emphasises the practice of functional tasks and importance of relearning real-life activities for patients. Principles of learning and biomechanical analysis of movements and tasks are important.
- There is no evidence adequately supporting the superiority of one type of exercise approaches over another. However, the aim of therapeutic approach is to increase physical independence and to facilitate the motor control of skill acquisition and there is strong evidence to support the effect of rehabilitation in terms of improved functional independence and reduced mortality.

Functional electrical stimulation (FES):
- FES is a modality that applied a short burst of electrical current to the hemiplegic muscle or nerve.
- In Hemiplegia Physical Therapy, FES has been demonstrated to be beneficial to restore motor control, spasticity, and reduction of hemiplegic shoulder pain and subluxation. It is concluded that FES can enhance the upper extremity motor recovery of acute stroke patient.
- FES could reduce spasticity in stroke patient. A recent meta- analysis of randomized controlled trial study showed that FES improves motor strength.
- FES can significantly improve arm function, electromygraphic activity of posterior deltoid, range of motion and reduction of severity of subluxation and pain of hemiplegic shoulder.
Biofeedback:
- Biofeedback is a modality that facilitates the cognizant of electromyographic activity in selected muscle or awareness of joint position sense via visual or auditory cues. In Hemiplegia Physical Therapy the result of studies in biofeedback is controversial.
- A meta-analysis of 8 randomized controlled trials of biofeedback therapy demonstrated that electromyographic biofeedback could improve motor function in hemiplegic patient.
- Another meta-analysis study on EMG has showed that EMG biofeedbcak is superior to conventional therapy alone for improving ankle dorsiflexion muscle strengthbshowed that biofeedback could improve earlier postural control to improve impaired sitting balance.
LIMB PHYSIOTHERAPY.
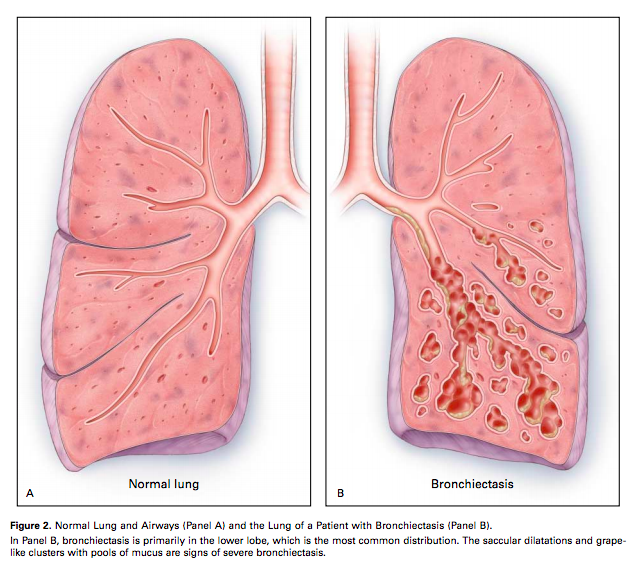
CHEST PHYSIOTHERAPY:
- Directed coughing and FET can be used as a technique for bronchial hygiene clearance in hemiplegic patient.
POSITIONING:
- In hemiplegia Physical Therapy consistent “reflex-inhibitory” patterns of posture in resting is encouraged to discourage physical complication of hemiplegia and to improve recovery.
TONE MANAGEMENT:
- A goal of hemiplegia Physical Therapy interventions has been to “normalize tone to normalize movement.” Therapy modalities for reducing tone include stretching, prolonged stretching, passive manipulation by therapists, weight bearing, ice, contraction of muscles antagonistic to spastic muscles, splinting, and casting.
Manual stretch of finger muscles, pressure splints, and dantrolene sodium do not produce apparent long-term improvement in motor control. - Dorsal resting hand splints reduced spasticity more than volar splints, but the effect on motor control is uncertain while TENS stimulation showed improvement for chronic spasticity of lower extremities.
SENSORY RE-EDUCATION:
- Bobath and other therapy approaches recommend the use of sensory stimulation to promote sensory recovery of hemiplegic patients.
GAIT TRAINING:

Intervention aims to optimize walking performance by:
- Preventing adaptive changes in lower limb soft tissues.
- Eliciting voluntary activation in key muscle groups in lower limbs.
- Increasing muscle strength and coordination.
- Increasing walking velocity and endurance.
- Maximizing skill, i.e., increasing flexibility.
- Increasing cardiovascular fitness.
The major emphasis in walking training is on:
- Support of the body mass over the lower limbs
- Propulsion of the body mass
- Balance of the body mass as it progresses over one or both lower limbs
- Controlling knee and toe paths for toe clearance and foot placement
- Optimizing rhythm and coordination.
CONVENTIONAL GAIT TRAINING:
Conventional gait training has focused on part-practice of components of gait in preparation for walking. It includes
- Symmetrical Weight bearing training
- Weight shifting
- Stepping training (swinging / clearance )
- Heel strike
- Single leg standing
- Push off / Calf rise. Followed by,
Circuit training (reaching in sitting and standing, sit-to-stand, step-ups, heel lifts, isokinetic strengthening, walking over obstacles, up and down slopes).
Traditional approaches to stroke recovery have a focus on neuro facilitation or neuro developmental techniques (NDT) to inhibit excessive tone, stimulate muscle activity if hypotonia is present and to facilitate normal movement patterns through hands-on techniques. Practice based on the framework advocated by Berta Bobath remains the predominant physical therapy approach to stroke patients in the UK and is also common in many other parts of the world, including Canada, United States, Europe, Australia, Hong Kong and Taiwan. The Bobath framework has evolved from its original foundations, however, therapists surveyed on the core Bobath elements still emphasize normal tone and the necessity of normal movement patterns to perform functional tasks. Strength training to improve walking ability Task-specific training to improve walking ability.
TREADMILL TRAINING:
- Body weight-supported treadmill training was one of the first translations of the task-specific repetitive treatment concept in gait rehabilitation after hemiplegia.





It was fyn
This is helping me more and more as a physiotherapy student am completing this year thnx alot
Hi I am an occupational therapist, the information that you provided was very informative and helpful to further continue therapeutic intervention for my patients who have sustained a stroke. If you have the exercises you provided in PDF form, I would very much like to download copies to implement in my treatment plans.
Apka treatment humko bahoot axa lga
NYC…
100%✓
Please
Please contact your doctor as early as possible.
Hello !
Please Contact Dr. Nitesh Patel – Senior Physiotherapist in Samarpan Physiotherapy Clinic, Ahmedabad mo no : 09898607803
Hello Dr. Nitesh, you have been doing a great work and I have been following all your teachings I am learning from there greatly thank you.