Shoulder Hand Syndrome Exercise: Physiotherapy Treatment
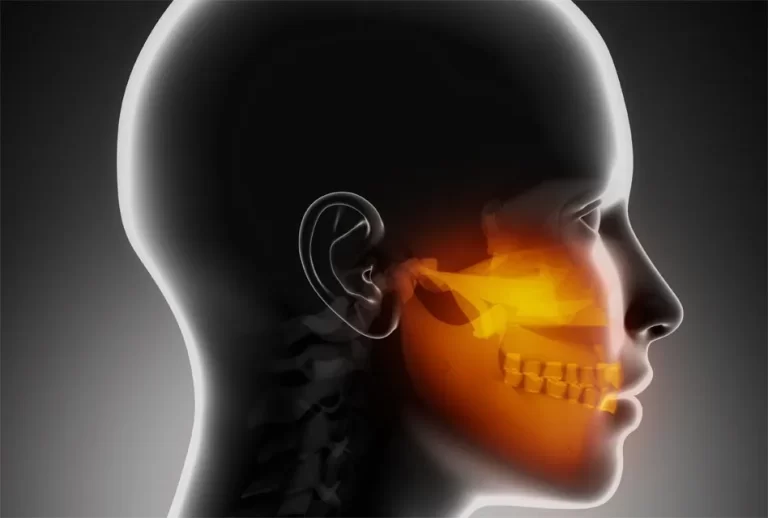
What is Shoulder-hand syndrome?
- A condition characterized by shoulder pain, swelling, stiffness, vasomotor symptoms of arm and hand, and skin edema/in duration, seen in patients above age 50 after an acute MI, or less commonly a cerebrovascular accident or head trauma.
- Shoulder-hand syndrome is attributed to reflex sympathetic stimulation; some patients later develop adhesive capsulitis, sclerodactyly, and decreased range of motion with regional demineralization.
- There is a waste of the muscles and the hand may become hot, sweaty, and swollen. Spontaneous recovery is usual but this may take up to two years.
- Shoulder-hand syndrome (steinbrocker syndrome), also known as reflex sympathetic dystrophy syndrome refers to shoulder pain and shoulder movement disorder associated with ipsilateral hand pain and swelling characteristics, sometimes a group of integrated finger contractures signs.
- The prevalence of both men and women, women slightly more than men, 90% of patients with age of onset is 50 years of age.
- The shoulder-hand syndrome generally develops as a reflex dystrophy with accompanying causalgia, characterized by pain in the shoulder.
- This is also associated with swelling and pain in the hand, on the involved side. Changes in the shoulder joint are identical to those seen in the frozen shoulder syndrome.
- The shoulder hand syndrome begins to emerge as the patient persists in keeping the shoulder and shoulder girdle immobile. Disuse of the involved muscles brings on a progressively painful stiff shoulder.
- Uniform edematous swelling of the hand begins to develop and finger joint motion becomes progressively limited.
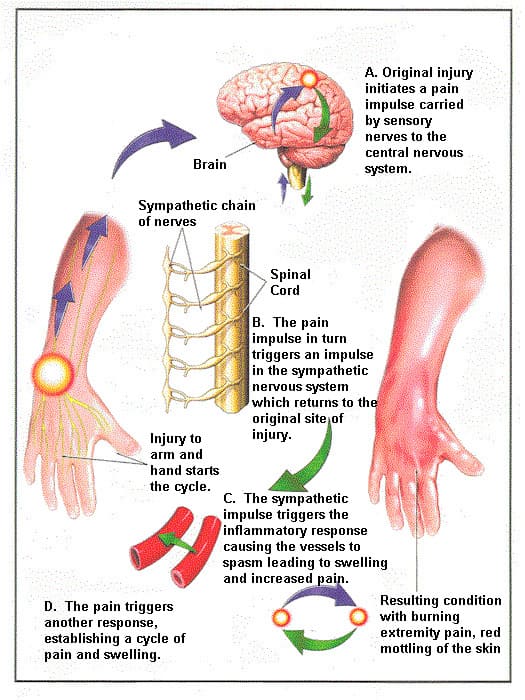
- The mechanism postulated to be responsible is a reflex-like response to pain sensation by sympathetic nerves, which communicate with the involved sensory nerve in the internuncial pool in the spinal cord.
- The sympathetic nerves respond to the distally occurring pain by triggering a reflexive efferent reactive vasomotor action in the involved region.
- This effectively reduces blood circulation to the tissues perceived to be involved in the pain pattern.
- The changes in the hand brought on by shoulder-hand syndrome progress in three stages:
- (1) The patient complains of a burning pain in the hand which is coincidentally either cold and clammy or cold, red, moist, stiff, and superficially sensitive to touch or pressure.
- (2) The hand appears white and creaseless, the skin thickened, and the hand is increasingly cold and stiff.
- (3) The hand appears pale and thin, and there is muscular atrophy (guttering) with contractures of the joints (osteoporosis may become evident with an x-ray).
- At the end of this process, the hand and arm are generally useless and non-functional.
Causes
- Trauma (often minor).
- Ischemic heart disease and myocardial infarction.
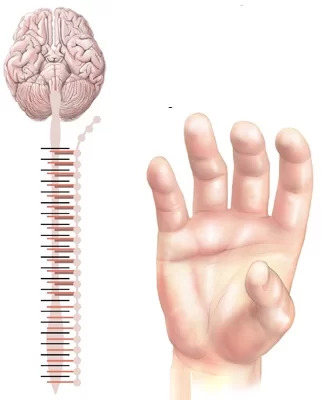
- Spinal cord disorder.
- Cerebral lesions.
- Stroke
- Infections.
- Surgery.
But it’s unclear exactly how shoulder-hand syndrome manifests itself. A neurological system “short circuit” is one explanation put forward. The sympathetic (unconscious) nervous system becomes overactive as a result of this “short circuit,” affecting the local sweat glands and blood flow.
Usually, symptoms follow an accident or surgery.
Additional reasons might be nerve pressure, infection, cancer, issues with the neck, stroke, or heart attack. It appears that some individuals are more genetically prone to this condition than others.
Signs and Symptoms:
- Due to different causes, and clinical manifestations. Secondary to myocardial infarction by more than 2 to 16 weeks after the disease onset, the longest up to 14 months.
- A slightly more common incidence of left shoulder and hand over the right shoulder and hand or bilateral shoulder and hand onset showed gradual shoulder and hand stiffness, fatigue and discomfort, or hand sudden pain, stiffness, swelling, hypersensitivity, sweating, and skin color change.
- The course of the disease can be divided into three stages.
- Stage 1: Shoulder and hand pain, movement disorders to diffuse swelling appear later, the gradual emergence of stiffness, a wider range of shoulder pain, not involving the elbow.
- This period of sustainability is 3 to 6 months.
- Stage 2: Pain and swelling may gradually reduce and subside gradually, but the shoulder joint dysfunction, finger flexion contracture and stiffness, and muscle atrophy.
- X-ray film showed significant osteoporosis, this period will last 3 to 6 months.
- Stage 3: Palm and subcutaneous tissue contraction, finger tonic deformation activities significant barriers, the shoulder was frozen shoulder less residual pain.
- The duration of symptoms varies, in some cases up to a few years, and some stop in the course of development or healing.
Clinical Features:
- Pain:
- Occurring in one or more extremities is described as severe, constant, burning, and/or deep aching pain.
- All tactile stimulation of the skin (e.g. wearing clothing, a light breeze) may be perceived as painful (allodynia).
- Paroxysmal dysaesthesias and lancinating pains.
- Skin changes:
- The skin may appear shiny (dystrophy-atrophy), dry, or scaly.
- Hair may initially grow coarse and then thin. Nails in the affected extremity may be more brittle, grow faster, and then slower.
- Rashes, Ulcers and Pustules.
- Abnormal sympathetic (vasomotor changes) activity may be associated with skin that is either warm or cold to touch.
- Increased sweating (sudomotor changes) or increased chilling of the skin with goose flesh (pilomotor changes).
- Swelling:
- Localized, initially pitting and later Brawnyb.Edema may be sharply demarcated along a line on the skin surface.
- Movement disorder:
- May develop dystonia.
- Tremors and involuntary jerking of extremities may be present.
- Disuse atrophy sets in natural history.
- Spreading symptoms:
- A “continuity type” of spread where the symptoms spread upward from the initial site, e.g. from the hand to the shoulder.
- A “mirror-image type” where the spread was to the opposite limb.
- An “independent type” where symptoms spread to a separate, distant region of the body. This type of spread may be spontaneous or related to a second trauma.
- Total body RSD.
Pathology:
- Sympathetic pain results from tonic activity in myelinated mechanoreceptor afferents. Input causes tonic firing in neurons that are part of a nociceptive pathway.
- Injury to central or peripheral neural tissue.
- Elevated levels of soluble tumor necrosis factor receptor 1 (sTNF-R1) and enhanced tumor necrosis factor-alpha activity in patients with polyneuropathy with allodynia.
- Distal degeneration of small-diameter peripheral axons may be responsible for pain, vasomotor instability, edema, osteopenia, and skin hypersensitivity of shoulder hand syndrome.
- Cortical changes suggest a possible role in pathophysiology.
Differential Diagnosis
- Unrecognized local pathology (fracture, sprain).
- Traumatic vasospasm.
- Cellulitis.
- Lymphedema.
- Raynaud’s disease.
- Thromboangiitis obliterans.
- Erythromelalgia.
- DVT.
- Also, nerve entrapment syndromes, occupational overuse syndromes, and diabetic neuropathy.
Treatment of Shoulder Hand Syndrome:
Absolutely, a skilled multidisciplinary team that is motivated, well-coordinated, and uses individualized therapy to treat the disease is the key to successful treatment.
- No scientifically validated cure exists
- Therapy is directed at managing the signs and symptoms of the disease
- A multidisciplinary approach utilizing pharmacotherapy, physical therapy, and psychological therapy is most appropriate.
Physiotherapy Treatment:

- Early physical therapy is essential to avoid atrophy and contractures of the affected limb.
- Physiotherapy has been shown to reduce pain and motor impairment and improve the function and coordination ability of the limb.
- Requires that the patient take an active role in their care.
- Physical therapy intervention includes:
- TENS.
- Aquatic therapy.
- Mirror therapy
- Desensitization
- Gradual weight bearing.
- Stretching.
- Fine motor control.
- In acute phase:
- Immobilization and contralateral therapy should be the treatment. Intensive active therapy in the acute phase can lead to deterioration.
- In chronic phase:
- Passive physical therapy includes manipulation, manual therapy, massage, and mobilization.
- Lymphatic drainage can be used to facilitate the regression of edema.
- You can also threat tender points by the following rules: more severe tender points as identified by tenderness to palpation are treated before less severe tender points; more proximal or more medial tender points are addressed before more distally and laterally located points; the area of greatest accumulation of tender points is treated first; when tender points are located in a row, the one in the middle of the row is treated first.
- Therapeutic exercise including isometric strengthening therapy followed by active isotonic training in combination with sensory desensitization programs.
- The strengthening training includes exercises for all four extremities and trunks. The exercises can be done with theraband.
- Desensitization programs contain giving stimuli of different fabrics, different pressures (light or deep), vibration, tapping, heat, or cold. The exercises can be stress-loading (f.e. scrubbing, walking, carrying weights), endurance training, written instructions, and functional training. It is also useful to give the patient a home exercise program.
- Mirror therapy or mirror visual feedback:
- Mirror therapy involves placing both hands into a box with a mirror separating the two compartments and, while moving both hands, watching the reflection of the unaffected hand in the mirror.
- Reducing pain intensity and improving function in post-stroke shoulder hand syndrome.
- A significant improvement in pain with mirror therapy.
- Improve function.
- Graded motor imagery/learning:
- Graded motor imagery consists of recognition of hand laterality and imagined hand movement.
- Relaxation.
- Cognitive-behavioral therapy:
- Contains relaxation training, deep breathing exercises, and biofeedback.
- Neuromodulation or invasive stimulation techniques:
- Neuromodulation contains peripheral nerve stimulation with implanted electrodes, epidural spinal cord stimulation, deep brain stimulation, and electrotherapy.
- Electrotherapy includes transcutaneous electric nerve stimulation TENS, Spinal cord stimulation, and non-invasive brain stimulation (repetitive transcranial magnetic stimulation).
- Other treatments:
- Whirlpool bath/ contrast baths.
- Vocational and recreational rehabilitation.
- Psychological therapies: cognitive-behavioral therapy (CBT), operant conditioning (OC), counseling, pain education, and relaxation techniques.
- Acupuncture, electroacupuncture.
- Tactile sensory discrimination training.
- Weight-bearing.
- Ultrasound therapy.
- Kinesiotaping.
- Psychological therapy:
- An integral part of the multidisciplinary treatment approach. Many patients with shoulder hand syndrome have a significant amount of psychological dysfunction, which is a reflection of the disease process itself as opposed to a cause thereof.
- Pain coping skills.
- Biofeedback.
- Relaxation training.
- Cognitive behavioral therapy.
- Mirror therapy.
- Invasive/intervention therapy:
- Sympathetic nerve blocks.
- Spinal cord stimulation.
- Surgical/chemical sympathectomy.
- Peripheral nerve stimulator.
- Intrathecal baclofen pump.
Surgical Treatment
In the case that non-surgical therapies are ineffective, surgical interventions may provide a more effective means of managing the condition.
Spinal cord stimulator:
Your spine is implanted with tiny electrodes that send modest electric shocks to the damaged nerves.
Pain pump implantation:
This involves implanting a tiny device close to the belly that sends painkillers to the spinal cord.
Counseling and psychological testing are important additional treatments for shoulder-hand dysfunction.
FAQ
What is shoulder hand syndrome?
The phrase “shoulder hand syndrome” refers to painful upper extremity impairments caused by disruptions in the sympathetic nervous system. The sympathetic nervous system is thought to be reflexively stimulated, causing the observed trophic and vasomotor symptoms.
What is the cause of shoulder-arm syndrome?
A painful impairment known as a shoulder-arm syndrome can occasionally occur after a sprain, laceration, or minor fracture. The patient still has an arm and hand that is full, discolored, sore, uncomfortable, and non-functional, even if the original cause may have been insignificant.
How do you get rid of hand and shoulder pain?
To get rid of hand and shoulder pain:
Apply ice to the shoulder region for fifteen minutes, then remove it for fifteen more. For two to three days, do this three to four times a day.
Give your shoulder some rest over the upcoming days.
Return to your normal activities gradually.
Acetaminophen (like Tylenol) or ibuprofen can help lessen pain and inflammation.
What is another name for shoulder-hand syndrome?
Another name for shoulder-hand syndrome are:
Reflex sympathetic dystrophy
Sudeck’s atrophy
Shoulder-hand syndrome
Steinbrocker syndrome
Causalgia.
What is the shoulder-hand syndrome score?
The presence or severity of clinical symptoms of shoulder-hand syndrome (SHS), or CRPS of the upper limbs following a stroke, is measured using the Shoulder-Hand Syndrome (SHS) Score. It can be used to monitor how well subluxation therapy is working to prevent or lessen SHS.
What is Stage 3 of shoulder hand syndrome?
Stages of shoulder hand syndrome are:
Stage 1–acute
Stage 2–dystrophic
Stage 3–atrophic.




Thank you for the information. It’s helpful.
Its good and easy to learn and ita useful
It’s the first time in 5 months that I got a correct info about my condition after consultations of orthopedics, neurologists and physiotherapist
Thank you so much it is becoming very helpful for my final exams in bachelor of physiotherapy in final year …