Legg-Calve-Perthes Disease
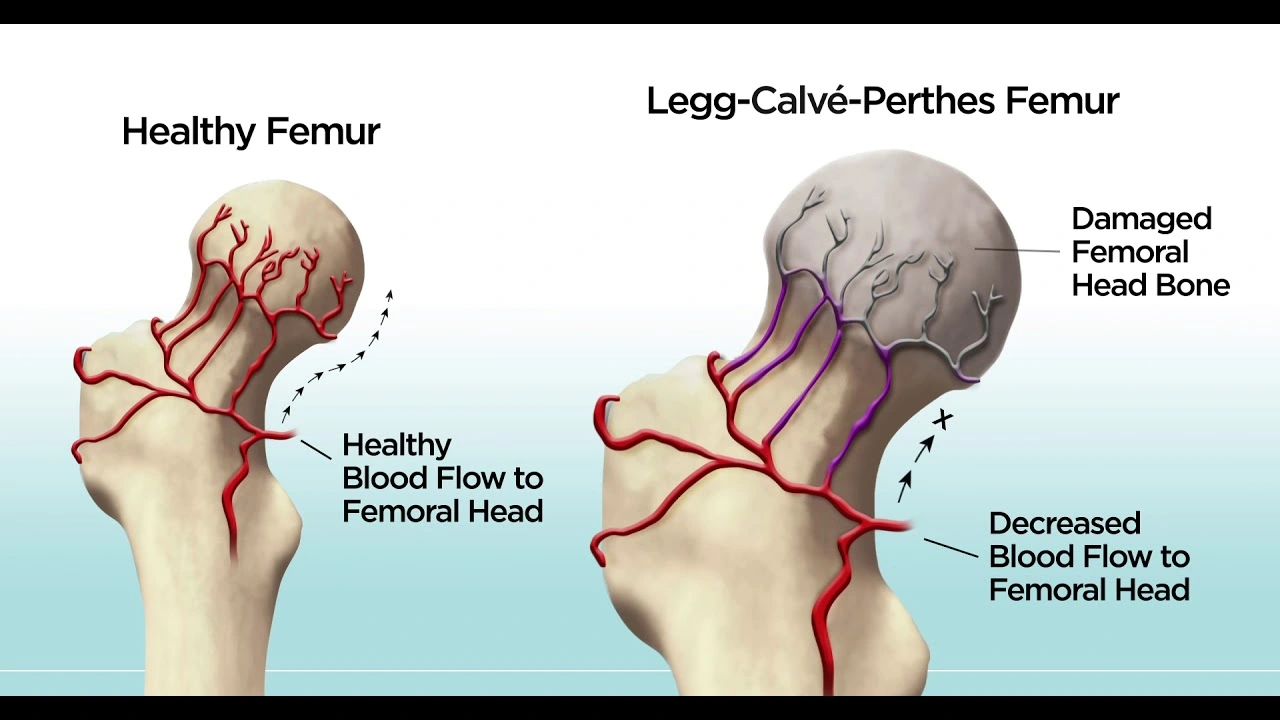
What is Legg-Calve-Perthes Disease?
Legg-Calve-Perthes disease is an infrequent childhood disease that involves the hip. It happens when the blood supply to the spherical head of the femur (thighbone) is temporarily disrupted. Without a sufficient blood supply, the bone cells die, a method is known as avascular necrosis.
Legg-Calve-Perthes disease also called Perthes disease, is named for the three individual doctors who first defined the disease as typically happening in kids who are between 4 and 10 years old. It is five times more familiar in boys than in girls, yet, it is probable to cause more extensive injury to the bone in girls. In 10% to 15% of all patients, both hips are involved.
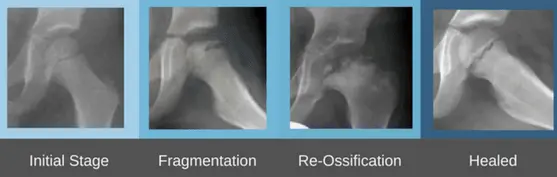
Stages of Legg-Calve-Perthes Disease
There are four stages of Perthes disease:
Initial / necrosis. In this phase of the condition, the blood supply to the femoral head is disrupted and bone cells die. The place evolves intensely inflamed and irritated and your kid may start to show signs of the condition, like limp or various ways of walking. This initial phase may last for fewer months.
Fragmentation. Over 1 to 2 years, the body removes the dead bone under the articular cartilage and fast substitutes it with an initial, softer bone (“woven bone”). It is during this stage that the bone is in a weaker form and the head of the femur is more probable to collapse into a flatter position.
Reossification. New, stronger bone evolves and starts to bring shape to the head of the femur. The ossification phase is frequently the longest phase of the condition and can last a few years.
Healed. In this phase, the bone regrowth is finished and the femoral head has got its final shape. How close the shape is to round will depend on several factors, involving the extent of injury that carried place during the fragmentation stage, as well as the kid’s age at the onset of the condition, which involves the potential for bone regrowth.
Epidemiology
Legg-Calve-Perthes disease – LCPD disease is relatively unusual and in Western populations has an incidence approaching 5 to 15:100,000.
Boys are five times more likely to be included than girls.
Presentation is normally at a younger age than slipped upper femoral epiphysis (SUFE) with peak presentation at 5-6 years, but trust intervals are as broad as 2-14 years.
Symptoms of Legg-Calve-Perthes Disease
Signs and symptoms of Legg-Calve-Perthes disease contain:
- Limping
- Pain or stiffness in the groin, hip, thigh, or knee
- Limited range of movement of the hip junction or joint
- Pain that is extreme with activity and enhanced with rest
- Legg-Calve-Perthes disease generally includes just one hip. Both hips are involved in some kids, generally at various times.
Risk factors
Risk factors for Legg-Calve-Perthes disease contain:
Age. Although Legg-Calve-Perthes disease can impact kids of almost any age, it most generally starts between ages 4 and 10.
Your child’s sex. Legg-Calve-Perthes is almost four times more familiar in boys than in girls.
Race. White children are more probable to create the disease than black children.
Genetic mutations. For a small numeral of a patient, Legg-Calve-Perthes disease seems to be linked to mutations in specific genes, but more study is required.
Differential Diagnosis
Differential diagnoses that must be considered given the radiographic findings contain:
- Infectious etiology involving osteomyelitis, septic arthritis, pericapsular pyomyositis
- Transient synovitis
- Multiple epiphyseal dysplasias (MED)
- Spondyloepiphyseal dysplasia (SED)
- Sickle cell disease
- Gaucher disease
- Hypothyroidism
- Meyers dysplasia
Doctor Examination
History
Limp of acute or insidious start, frequently painless (1 to 3 months)
If the ache is current, it can be localized to the hip or referred to the knee, thigh, or abdomen
With progression, the ache generally worsens with movement
No systemic symptoms should be seen
Physical Examination
Decline abduction and internal rotation of the hip
Atrophy of thighs and buttocks from aches leading to disuse
Ache on rotation referred to the anteromedial thigh and/or knee
Afebrile
Leg length discrepancy
Gait Evaluation
Antalgic gait (acute): Short-stance stage secondary to ache in the weight-bearing leg
Trendelenburg gait (chronic): Downward pelvic tilt away from the involved hip during the swing stage
Lab test
X-rays. These scans provide images of dense structures such as bone and are needed to verify a diagnosis of Perthes. X-rays will indicate the situation of the bone in the femoral head and assist your doctor or physician decide the stage of the condition.
A kid with Perthes can expect to have several x-rays carried throughout therapy, which may be 2 years or longer. As the disease progresses, x-rays frequently look worse before gradual progress is noticed.
Treatment of Legg-Calve-Perthes Disease
The goals of therapy involve pain and symptom management, restoration of hip range of movement, and containment of the femoral head in the acetabulum.
The more youthful the age at the time of display, the more benign condition course is expected, and also for the same age, the prognosis is better in boys than girls due to less maturity. Conservative therapy is favorable in kids with a skeletal age of 6 years or less at the time of condition start.
Nonoperative Treatment
Indicated for kids with bone age less than 6 or lateral pillar A involvement.
Movement restriction and defensive weight-bearing are suggested until ossification is finished.
People may still take interest in physical treatment.
The literature does not support the use of braces, orthotics, or casts.
NSAIDs can be defined as comfort.
Referral to an experienced pediatric orthopedist is suggested.
Good effects are reported in up to 60% of people.
Operative Treatment.
Femoral or Pelvic Osteotomy
Indicated in children over 8 years old.
Results are better in lateral pillars B and B/C with surgery corresponding to A and C
Research indicates that surgery should be early before deformity of the femoral head evolves.
Valgus or Shelf Osteotomies
Shown in kids who have hinge abduction.
Outcomes in progress to the abductor mechanism
Hip Arthroscopy
Is evolving more familiar as a modality for mechanical symptoms and/or femoroacetabular impingement
Hip Arthrodiastasis
Assumed a more controversial choice.
In later life, hip replacements may be required.
Physiotherapy treatment in Legg-Calve-Perthes Disease
Physiotherapy interventions have been indicated to enhance the range of motion and strength in this people population. Patients show greater progress in muscle strength, gait speed, functional mobility, and quality of movement performance.
Physiotherapy Goals
- Decrease pain
- Increase range of motion
- Increase strength
- Patient to be independent with the proper assistive instrument and weight-bearing precautions
- Enhance balance
- Enhanced efficiency in walking
Pain
Hot pack for ache management with stretching
Cryotherapy
Drugs as prescribed by the referring physician or doctor for pain
ROM (range of motion)
A static stretch for Lower Extremity musculature with or without the use of a hot pack
The dynamic range of motion and active assistive range of motion (AAROM) may be suitable if the person is muscle guarding due to ache
Conduct an active range of motion and active assisted range of motion following passive stretching to keep a newly gained range of motion
Accomplish stretching in a position that is appropriate for the individual and contains hip External Rotation, hip Internal Rotation, hip abduction, hip extension, and any further lower extremity movement that is significantly restricted
Strength
Start with isometric activity and progress to isotonic activities in a gravity-lessened position with another progression to isotonic activities against gravity. Contain concentric and eccentric contractions
Concentrate on strengthening of hip flexors, hip abductors, hip internal rotators, hip external rotators, hip extensors, or any other lower extremity muscle group that shows notable strength deficits. A special alert is to be provided to the gluteus medius to minimize intraarticular ache and for pelvic control during single-leg exercises and ambulation.
Performance of weight-bearing vs. non-weight-bearing activities is based on the weight-bearing status as specified by the physician or doctor, patients tolerance to weight-bearing positions, and security
Closed chain double limb activities with light resistance (less than full body weight) may be conducted
It is not suggested to perform single-limb closed-chain activities on the engaged side due to improved intra-articular pressure in the hip junction or joint
Balance
Exercises that contain a double limb stance and a narrowed base of assets on stable surfaces may be achieved if weight-bearing status and symptoms permit
It is not suggested to perform single-limb exercises due to improved intra-articular pressure in the hip junction or joint
Gait
Follow the referring physicians or doctor approaches for weight-bearing status.
Start gait training with the proper assistive instrument given weight bearing status as specified by the referring physician or based on the patient’s tolerance to full weight bearing due to ache or safety.
Post-operative management
Rehabilitation is defined regarding the different phases of rehabilitation.
Initial Phase (0-2 weeks post-cast removal):
The purposes of the Initial Stage are:
Minimize pain
Hot pack for relaxation and ache management with stretching.
Cryotherapy.
Medication for pain.
Optimize range of motion of hip, knee, and ankle
A passive static stretch hot pack may be used, based on people’s preferences and convenience.
The dynamic range of motion.
Perform an active range of motion and active assisted range of motion following passive stretching to keep the newly gained range of motion.
Increase strength for hip abduction, flexion, and extension and knee and ankle.
Start with isometric activities at the hip and improvement to isotonic activities in a gravity-lessened position.
Start with isometric activities at the knee and ankle, moving to isotonic activities in a gravity-lessened position with different progression to isotonic activities against gravity.
Start with 2 sets of 10 to 15 repetitions of each activity with progression to 3 sets of each activity to be used.
Improve gait and functional mobility.
Follow the referring physician’s procedures.
Transfer training and bed mobility to maximize freedom with ADLs.
Gait training with the proper assistive instrument, concentrating on safety and independence.
Improving skin integrity.
Scar massage and desensitization to underestimate adhesions.
A warm bath to enhance skin integrity following cast removal, if possible in the home environment.
A warm whirlpool may be used if the person is unable to safely use a warm bath for skin integrity management.
A physical therapist is supervised at a frequency of 2-3 times per week (weekly).
Intermediate Phase (2-6 weeks post-cast removal)
Purposes of the Intermediate Phase
Minimize pain (see initial phase)
Normalize the range of motion of the knee and ankle and optimize the range of motion of the hip in all directions
Improve the strength of the knee muscle and hip muscle
Isotonic activities of the hip in gravity-lessened positions and advancing to opposite to the gravity positions.
Isotonic activities of the knee and ankle in gravity lessened and opposite to the gravity positions.
Maintain independence with functional mobility maintaining and use of appropriate assistive devices.
Improving gait and functional mobility.
Follow the referring physician’s or doctor’s guidelines.
Persist gait training with the proper assistive instrument concentrating on safety and independence.
Start slow walking in chest-deep pool water with arms submerged.
Improving Skin Integrity.
Persist with scar massage and desensitization.
A physical therapist is supervised at a frequency of 2-3 times per week (weekly). It is suggested that exercises outside of Physical therapy are limited at this time due to some reason. If the referring physician or doctor permits, swimming is allowed.
Advanced Phase (6-12 weeks post-cast removal)
Goals
Minimize pain (see initial phase).
optimize range of motion and flexibility of the hip, knee, and ankle.
Improve the strength of the knee and hip, except for hip abductors, to at least 70% of the unaffected lower extremity and improve the strength of the hip abductors to at least 60% of the unaffected lower extremity due to mechanical drawback (4 + 5).
Isotonic activities of the hip, knee, and ankle in gravity lessened and opposite to the gravity positions, involving concentric and eccentric contractions.
WB and non-weight bearing (NWB) exercises can be used in combination based on the patient’s capacity and the purposes of the therapy session.
Startupper extremity-supported functional dynamic single limb exercises (eg. step-ups, side steps).
Resume with double limb closed chain activities with opposition, moving to single-limb closed chain activities with light resistance if weight bearing – WB status permits.
Use of a stationary bicycle in an upright or recumbent position maintaining the hip in less than 90 degrees of flexion.
Ambulation without the help of an assistive machine or pain.
Negotiate stairs independently using a step-to-pattern with upper extremity (UE) asset.
Enhance balance to greater than 69% of the top Pediatric Balance Score (39/56) or single-limb stance of the unaffected side.
Enhancing gait and functional mobility.
A physical therapist is supervised at a frequency of 1-2 times per week (weekly).
It is suggested that exercises outside of Physical therapy are restricted to swimming if the referring physician or doctor permits.
Note: Running and jumping exercises are limited at this time.
Pre-Functional Phase (12 weeks to 1+ year post-cast removal)
Goals
Minimize pain (see initial phase).
Optimize range of motion and flexibility of the hip, knee, and ankle.
Static stretch
Improve the strength of the knee and hip, except for hip abductors, to at least 80% of the unaffected lower extremity and improve the strength of the hip abductors to at least 75% of the unaffected lower extremity due to mechanical drawback.
Negotiate stairs independently with reciprocal way and upper extremity assets.
Enhance balance to 80% or greater of the top Pediatric Balance Score (at least 45/56) or single-limb stance of the unaffected side.
Non-painful gait pattern with tiniest deficits and normal efficiency.
A physical therapist is supervised at a frequency of 1-2 times per week (weekly).
It is suggested that exercises outside of Physical therapy contain swimming and bicycle riding as directed by the referring doctor or physician.
Note: Running and jumping exercises are limited at this time.
Functional phase
Goals
Relieve pain to 1/10 or less (see initial phase).
Normalizing range of motion: Improve range of motion to 90% or greater of the unaffected side for the hip, knee, and ankle, except for hip abduction and Improve hip abduction range of motion to 80% or greater due to potential bony block.
Normalizing strength: Improve the strength of the knee and hip, except for hip abductors, to 90% or greater of the unaffected lower extremity and Improve the strength of the hip abductors to at least 85% of the unaffected lower extremity due to mechanical drawback.
Move isotonic activities of the hip, knee, and ankle and contain concentric and eccentric contractions.
Weight-bearing – WB and non-weight bearing – NWB activities are used in combination based on the patient’s capability and purposes of the therapy session.
Functional dynamic single limb exercises (eg. step-ups, side steps) with upper extremity help as required for people security.
Improvement of single-leg closed chain activities with resistance.
Use of a stationary bicycle in an upright or recumbent position maintaining the hip in less than 90 degrees of flexion.
Ambulation with a non-ache full limp and normal efficiency.
Negotiation of stairs alone using a reciprocal pattern without upper extremity – UE support.
Enhance balance to 90% or greater of the top score on the Pediatric Balance Scale (at least 51/56) or single-limb stance of the unaffected side It is suggested that progression to the Functional Phase happens when the physician or doctor has decided there is adequate re-ossification of the femoral head based on radiographs. Note: Jumping and other impact exercises are still restricted and only progressed per instruction from the physician or doctor based on the healing and advancement of the conditioning process.
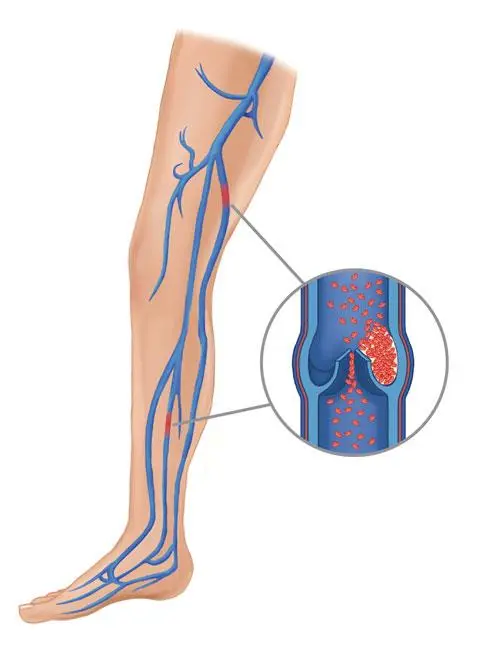
Complications
Kids who have had Legg-Calve-Perthes disease are at higher risk of developing hip arthritis in adulthood especially if the hip joint or junction heals in an irregular shape. If the hipbones don’t fit jointly well after healing, the joint or junction can wear out early.
In general, kids who are analyzed with Legg-Calve-Perthes after age 6 are more probable to develop hip issues later in life. The more youthful the kid is at the time of diagnosis, the better the options for the hip junction or joint to heal in a normal, spheroidal shape.
Prognosis
Kids younger than six have the best prediction since they have time for the dead bone to revascularize and remodel, with a fine option that the femoral head will heal and remain spherical after the resolution of the condition. Kids who have been analyzed with Perthes’ disease after the age of ten are at a very high risk of creating osteoarthritis and coxa Magna.
When an LCP condition diagnosis happens after age eight, a better result results with surgery instead of nonoperative therapies. The shape of the femoral head at the time when Legg-Calv Perthes disease heals is the most essential determinant of risk for degenerative arthritis; thus, the shape of the femoral head and congruence of the hip are the most helpful result measures.
FAQ
Is Perthes disease curable?
Most kids with Perthes’ disease ultimately heal, but it can bring anywhere from two to five years for the femoral head to regrow and return to normal, or near to normal.
Which characteristic would be common in Legg-Calve-Perthes disease?
What are the symptoms of Legg-Calve-Perthes disease? Kids with Legg-Calve-Perthes disease frequently produce a detectable limp. They may also experience immobility of the hip or complain of mild aches in the groin region, thigh, or knee. This ache is generally worse with exercise and enhances with rest.
Does Perthes need surgery?
Core decompression surgery is only suggested in the early phases of Perth’s condition, before the femoral head has collapsed, or flattened, and no longer fits neatly into the hip socket, called the acetabulum.
Is Perthes disease lifelong?
Kids with Perthes’ disease generally complain of aches in the groin area, the thigh, or the knee – especially after physical activity. They limp and have a limited range of motion (stiffness) of the hip junction or joint. These symptoms may continue on and off for numerous months. The condition itself lasts for a few years.
What does Perthes disease look like on an x-ray?
The specific findings of progressive burnt out (stage 4) Perthes condition are: femoral head deformity with broadening and flattening (coxa plana) proximal femoral neck malformation: coxa Magna. “sagging rope sign” (the slim sclerotic line running across the femoral neck)




One Comment