Hip Impingement Syndrome
What Is Hip Impingement Syndrome?
- Hip Impingement is a condition of the hip where additional bone is present on joint surfaces.
- Femoroacetabular impingement (FAI), also known as Hip impingement, as a mechanical or structural disorder of the hip.
- It can be occur in people of all ages, including adolescents and young adults.
- It occurs when the femoral head (ball of the hip) pinches up against the acetabulum (cup of the hip).
- When this happens, damage to the labrum (cartilage that surrounds the acetabulum) can occur, causing hip stiffness and pain, and can lead to arthritis.
- Hip impingement occurs when something prevents the smooth, painless, and free movement of the ball-and-socket joint.
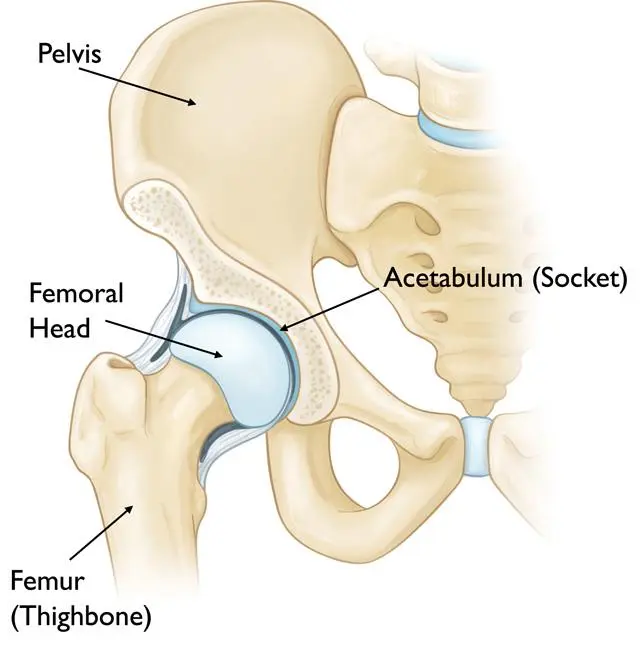
Anatomy Of The Hip Joint:
- In the healthy hip, the rounded top of thigh bone (femoral head) “plugs into” the hip socket (acetabular socket) in such a way that the femoral head can move smoothly within the socket.
- The ball and socket are lined with a thin layer of smooth cartilage that cushions and protects the bones, preventing them from rubbing or grinding against each other.
- The rim of the hip socket is lined with a special ridge of cartilage called the labrum that further helps to secure the femoral head in place inside the hip socket and prevents the dislocation.
Types Of Hip Impingement Syndrome:
There are mainly two types of hip impingement, Which includes:
- Cam impingement
- Pincer impingement
1. Cam impingement
- Cam impingement occurs because the ball-shaped end of the femur (femoral head) is not perfectly round. So, This interferes with the femoral head’s ability to move smoothly within the hip socket.
2.Pincer impingement
- Pincer impingement involves excessive coverage of the femoral head by the acetabulum. With hip flexion motion, the neck of the femur bone “bumps” or impinges on the rim of the deep socket and This results in cartilage and labral damage.
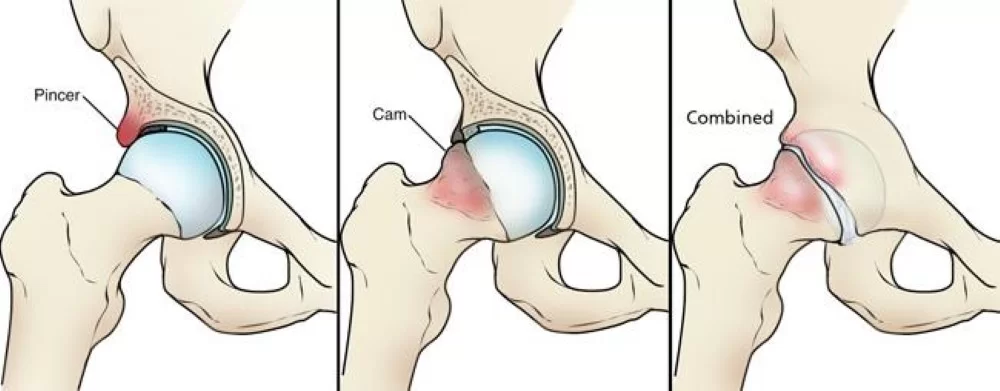
- Sometimes both of these conditions can exist at the same time, leading to cam and pincer impingement or it can also called combined impingement.
- Note that hip impingement can occur with or without the presence of osteoarthritis. In fact, sometimes untreated hip impingement is thought to lead to osteoarthritis in many patients.
Sign And Symptoms Of Hip Impingement:
In the early stages, there may be no symptoms associated with hip impingement or symptoms may be mild or vague. Some typical symptoms include:
- Stiffness in the thigh, hip, or groin
- The inability to flex the hip beyond a right angle
- Pain or stiffness in the groin or front of the thigh.
- This often occurs or is made worse with bending up of the hip or at the waist, such as when riding a bike, tying shoes or sitting for long periods of time.
Why It Occurs? (Causes Of Hip Impingement):
- Hip impingement may be caused by a misshapen femoral head, deformed femoral neck, or a hip socket that covers too much of the femoral head. Over time, repetitive “bumping” or impingement of the femur on the rim of the socket leads to cartilage and labral damage.
- People with hip impingement may have been born with a structurally abnormal ball-and-socket joint. In other cases, the hip joint may have become structurally abnormal during the development process.
- Repetitive activity that involve recurrent movement of the legs beyond the normal range of motion may cause hip impingement, which has been observed in certain athletes such as football, baseball, soccer, tennis, hockey, lacrosse players, dancers, and golf players.
- An injury to the hip joint may also cause symptoms of hip impingement.
- Further, certain conditions, such as Perthes disease and slipped capital femoral epiphysis (SCFE), may also become the cause of the hip impingement.
Who Is At Risk? (Risk Factors):
Current or past high level athletes, especially athletes or the one who play high intensity sports that require repeated hip flexion and twisting movements such as AFL, netball, and cycling, are at greater risk of hip impingement. Some of the other factors that may increase your risk includs:
- An active lifestyle especially throughout childhood and adolescence.
- Muscle imbalances
- Poor biomechanics
- Instability
- Past history of knee surgery
- Obesity
- Genetics
- Males are more at risk than females in such condition.
Diagnosis:
It based on a number of factors, that includes history, physical exam and imaging.
- X-rays should need to be done, including special views because it helps in evaluation of the abnormal shape of the bones.
- An MRI scan is often required to evaluate the soft tissue in the hip.
- Computed tomography (CT) scan which takes a series of small images at different angles and then applies a computer algorithm to construct a three-dimensional image of the hip. A CT scan is often used to show doctors the detailed structure of joints.
Treatment:
1. Non-surgical treatment (Conservative Treatment):
- The initial treatment for hip impingement syndrome does not involve any surgery. Many people with this condition can manage it with just simple lifestyle changes, And that includes:
The Activity Modification:
- Avoid the activities that worsen symptoms. Initially it is necessary to take as much rest as possible and put less stress on the hip joint.
Medical Treatment: Take Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
- Ibuprofen, naproxen, piroxicam, celecoxib, and others, may relieve pain and control inflammation. But NSAIDs should be used cautiously and for limited periods. It’s necessary to consult with physician before the use of the NSAIDs as it’s may have adverse side effects of certain diseases or certain drugs.
Steroid Injection:
- Injection of a corticosteroid along with a local anesthetic may also be helpful in relieving symptoms of hip impingement. It is important to limit the number of injections, as prolonged use of corticosteroid injections may likely to damage the surrounding structures.
Use assistive devices:
- Use of walking cane or crutches for a week or more when it’s needed. Because using assistive devises lessen the stress on hip joint.
Physiotherapy Treatment :
- Physiotherapy treatment is very effective in hip impingement because It helps to relieve pain, and restore the hip movement. See physiotherapy treatment below.
It is important to remember that this condition is an anatomical matter but symptoms can usually be managed well through conservative treatment. However, if you do not respond well to this approach after 4-6 weeks, you may require a corticosteroid injection or even the surgery.
2. Surgical Treatment:
There are mainly two main goals of surgical treatment in Hip Impingement Syndrome.
- The first is to address the damaged portion of the hip joint. This may involve repairing or removing of the damaged tissue.
- The second is to correct or improve the abnormal shape of the hip joint. This is often done arthroscopically by removing some of the extra bone. This involves small incisions and narrow instruments, and the surgeon will use a camera to look inside the hip.
If the surgeon feels you need a more extensive, open procedure, it would involve larger incision sites, a two- to four-day hospital stay and also the crutches for six to eight weeks.
3. Physiotherapy Treatment:
Physiotherapy treatment will help you to modify your lifestyle and activities and it also help you to control the symptoms. So that you can live your life normally without any complication of the condition.
I.Treatment Without Surgery:
Physiotherapy treatment without surgery can be conservative and it focus on prevention of further damage and management of the present symptoms.
- During the first 24 to 48 hours following the diagnosis, Physiotherapist may advise you to:
- Rest the area by avoiding walking or any activity that causes pain.
- Apply ice packs to the area for 15 to 20 minutes every 2 hours.
- Avoid high intensity exercise and movements requiring repeated hip flexion, twisting and deep squatting to relieve symptoms of hip impingement.
- Consult with a physician for further services, such as medication or imaging tests.
How physiotherapist will work with the you?
Reduce Pain And Swelling:
- If repetitive activities have caused the hip impingement, The Physiotherapist will help you to understand how to avoid or modify the activities to allow healing to begin. The therapist may use different types of treatments and technologies to control and reduce the pain and swelling, which includes application of ice, heat, ultrasound, electrical stimulation, taping, exercises, and also hands-on therapy, such as specialized massage.
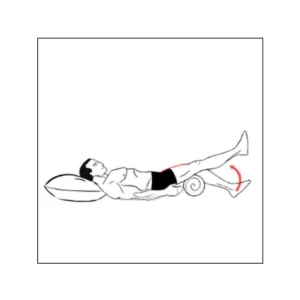
Improve Motion:
- Physiotherapist will choose specific activities and treatments to help restore normal movement in the hip and leg. These might begin with “passive” motion that they perform to gently move your hip joint, and progress to active exercises and stretches that you can do yourself.
- Joint mobilization may help ease pain from the hip joint and it also improves the motion of the joint.
- Note: These treatments do not always help the range of motion, especially if the shape of the bone at the hip joint has changed.
Improve Flexibility:
- A physiotherapist will determine if any leg or spinal muscles are tight, help you to stretch them, and also teach you how to stretch them.
- Stretching tight muscles can reduce abnormal forces that cause pain with motion.

Improve Strength:
- Strengthening of the hips and trunk can reduce abnormal forces on the already injured joint and help with strategies to compensate.
- The physiotherapist will choose and teach the correct exercises and equipment to steadily restore strength and agility. These may include using cuff weight, stretch bands, and weight-lifting equipment.
Improve Balance:
- Regaining a sense of balance is also important after an injury. A physiotherapist will teach exercises to improve balance skills.
Improving tolerance of daily activities:
- Your physiotherapist can consider your job and recreational activities and offer advice regarding maintaining postures that are healthier for your hip and activity modification. Often this involves limiting the amount of bending at the hip to avoid further hip damage.
Home Exercise Program:
- Your physiotherapist will teach the strengthening and stretching exercises to perform at home but these exercises will be specific for your needs.
Return To Activity:
- The physiotherapist will discuss the activity goals and use them to set your work, sport, and home-life recovery goals. The treatment program will help you to reach your goals in the safest, fastest, and most effective way possible. Your therapist will teach you exercises, work retraining activities, and sport-specific techniques and drills that match your lifestyle.
II.Treatment After Surgery (Post-Operative Treatment):
Postsurgical physiotherapy varies based on the procedure performed. It may include:
- To ensure your safety as you heal, your physiotherapist may recommend that you limit the amount of weight you put on the operated leg if there was a repair of the labrum. You may wear a brace to help limit the amount of bending at the hip. You might also use crutches to avoid overloading the leg if the bone on the femur was reshaped.
- Physiotherapist may use ice and electrical stimulation treatments during the first few therapy sessions to help you control your pain and swelling from the surgery. They may also use massage and other hands-on treatments to ease muscle spasm and pain.
- Your physiotherapist will guide you through safe range-of-motion, strengthening, and balance activities to improve your movement as quickly as possible while allowing the surgical site to heal properly.

- Treatments includes range-of-motion exercises and gradually work into active stretching and strengthening. Active therapy usually starts two to three weeks after surgery. So, therapist may start light isometric strengthening exercises. These exercises work the muscles without straining the healing process of the tissues.
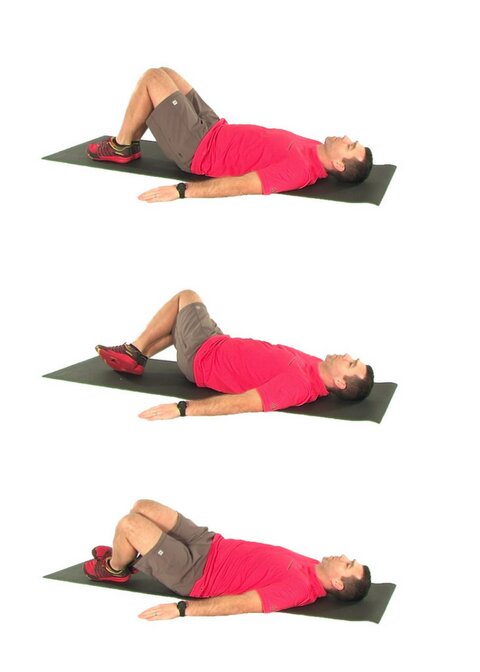
- After four weeks you may start doing more active strengthening. Exercises improve the strength and control of trunk, buttock and hip muscles. Your therapist will help you retrain these muscles to keep the bones in place.
- The therapist will help you to find ways that don’t put too much stress on your hip joint.
- The physiotherapist will also teach you the number of ways to avoid the possible problems in future.

Most people return to their normal activities about 3 months and to high-level sports about 4 to 6 months after surgery. Your physiotherapist will recommend a gradual return based on your condition.





2 Comments