Asthma
What is an Asthma?
”Bronchial asthma is a chronic, inflammatory disease of the respiratory tract, which is characterized by bronchial hyperreactivity and respiratory obstruction which is reversible (spontaneously or under the influence of bronchodilater) marked by wheezing, shortness of breath, chest tightness and coughing”.
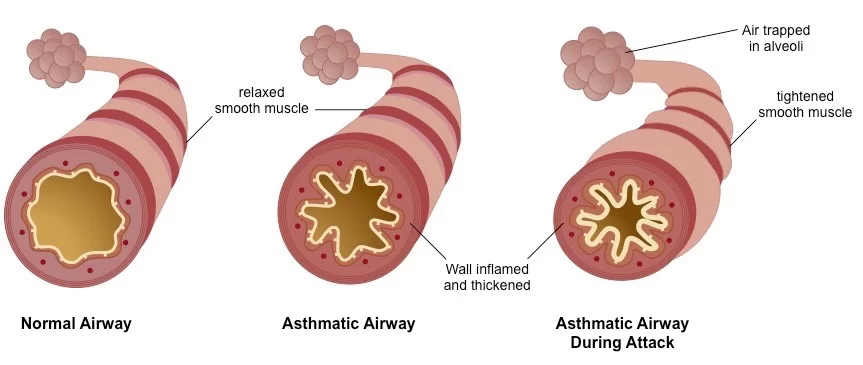
symptoms may be episodic or chronic but the pattern may vary considerably from time to time in individual patients. The changes causing airway obstruction in asthma include the hypertrophy and hyperplasia of bronchal smooth muscles, thickening of the epithelial basement membrane of the airways, oedema and eosinophilic infiltration of the bronchial wall, and hypertrophy of the bronchial mucus glands with an increase in number of the goblet cells. This leads to the narrowing of the larger bronchi and plugging of bronchi and bronchioles with viscid mucus which contains eosinophils and shed respiratory epithelial cells.
The lungs of patients dying from asthma show overinflation with widespread mucus plugs in airways of all sizes.
Causes of Asthma
The development of bronchial asthma is a multicausal process, which is caused by exogenic factors (environmental factors), and also by genetic dispositions. In addition, the course of the disease can be influenced by climatic changes and mental factors. Important exogenic activators are: · Allergens or Environmental allergens (house dust mites, pollen) Allergenic work substances (flour) or Food allergens · Toxins or chemical irritants ·Respiratory diseases · Pseudoallergic reactions (PAR) to analgesics (analgesic-induced asthma) · Physical exertion (mainly in children) Patients with allergic asthma or other atopical diseases show a polygenic inherited trait for an overshooting immune response of IgE. If both parents suffer from atopy, the children have an atopical disease as well in 40-50% of the cases.
Epidemiology
As a rule, bronchial asthma already occurs in infancy and is the most common chronic disease of this stage of life. There exist differing statements on the prevalence of bronchial asthma in Germany. Some authors mention 2-4%; other sources even 6-10%. The number of deaths caused by asthma in Germany is approx. 5000/year.
Classification
According to etiology
1. Allergic or extrinsic asthma- This generally begins earlier in life and is associated with atrophy-the presence of immediate hypersensitivity to external allergens associated with positive skin-prick tests. These patients show a high incidence of seasonal rhinitis and flexural eczema. There is usually a strong family history of asthma, hay fever, or eczema.
In patients with extrinsic asthma, episodes may be precipitated by exposure to antigenic materials, including pollens, house dust, animal furs, and feathers. Foodstuffs including milk, eggs, fish, and chocolate may, very occasionally, be incriminated. Patients with extrinsic asthma may also react adversely to non-allergic provoking factors including air temperature changes, emotional disturbances, exercise laughter, and respiratory tract infection(RTI).
2. Non-allergic or intrinsic asthma occurs later in life and allergic features are usually absent so the skin-prick test for common allergens is negative. This is more common in women than men.
3. Mixed form-Worsening symptoms of both types include bronchial irritation by strenuous exercise, exposure to cold air, dust, tobacco smoke, fumes, emotional stress, and respiratory infections.
According to a degree of severity
- Grade 1: Intermittent
- Grade 2: Persistent, mild
- Grade 3: Persistent, moderate
- Grade 4: Persistent, severe
According to clinical types.
- Episodic asthma may occur at any time by a feeling of chest tightness breathlessness and wheezing. Expiration becomes difficult with short gasping inspiration, and wheezes are usually expiratory and often audible without the aid of a stethoscope. A troublesome cough is common with scanty viscid mucus.
In severe episodes, there will be tachycardia,pulsus paradoxes, and central cyanosis.
2. Chronic asthma-There is persistence wheezing with breathlessness. cough with mucoid sputum and recurrent episodes of respiratory infections.
3. Childhood asthma-Wheeziness is common with minor respiratory infections. Non-asthmatic wheeziness usually resolves as the child grows. childhood asthma is commener in boys than girls and usually accompnies atopy.
4. Adult asthma-Asthma may persist into adult life from childhood.Irritanta including smog,ciggarette smoke, and pollens.
5. Status asthmaticus-These has been supersedes by ”SEVERE ACUTE ASTHMA” refers to episodes of severe wheezing and breathlessness lasting more than 24 hours not responding to normal medication and potentially threatning”PULSUS PARADOXUS ”and very quiet breath sounds on auscultation.
Pathophysiology
Genetic disposition and exogenous noxa trigger three pathophysiological processes which characterize bronchial asthma:
1. Inflammation of the bronchi
Allergens or infections elicit an infectious reaction of the bronchial mucous membrane. In allergic asthma, an IgE-induced reaction of the immediate type (Type 1 reaction) occurs immediately after inhalation of the allergen. The mast cells in the mucous membrane degranulate and thereby release inflammation mediators like histamine, ECF-A, bradykinin, and leukotrienes (“immediate reaction”). Apart from this immediate reaction, there also exists an IgG-induced late reaction after 6-12 hours or a combination of both reaction types (“dual reaction”). As a rule, the triggering allergen can only be identified at the early stage of the disease. In the course of years, the range of allergens often becomes wider, thereby making it more difficult or even impossible for the patient to avoid allergens.
2. Bronchial hyperreactivity
An unspecific bronchial hyperreactivity can be detected in almost all asthmatics. In case of the inhalation of irritants, the hyperreactivity manifests as a very strong constriction of the bronchial tubes, and can be objectified by the methacholine test.
3.Endobronchial obstruction
Endobronchial obstruction is the first clinically discernible “end product” of the pathophysiological processes of bronchial asthma. It develops through the shift of the bronchial lumen as a consequence of mucosal edema, increased mucus secretion (dyscrinism), and bronchospasms.
Symptoms
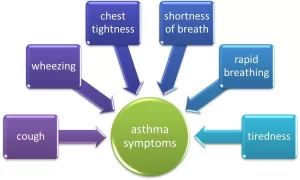
The severity of asthma varies from mild to severe and it is a chronic disease. An asthma attack is actually an acute exacerbation of the disease. When an attack is not there, it does not mean that Asthma is not there. The symptoms of Asthma consist of a triad of Dyspnea, Wheezing and Cough.
Symptoms of Asthma include:
- Cough: Cough can be productive or dry, and is especially seen in the early morning and at night.
- Breathlessness: Difficulty in breathing due to mucous plugging and airway spasm is worse by any physical activity like climbing stairs.
- Chest tightness: Tightness of the chest or pain in the chest is present along with other symptoms of asthma.
- Wheezing: Wheezing is an abnormal whistling sound due to difficult respiration. Wheezing is more commonly seen in children than adults.
Symptoms of Asthma in severe cases include:
- Bluish discoloration of lips and face with nasal flaring
- Rapid pulse
- Sweating
- Decreased level of consciousness
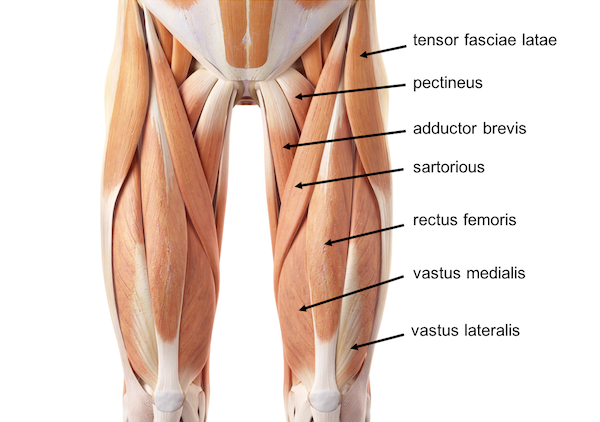
- In severe attacks, the accessory muscles (sternocleidomastoid and scalene muscles of the neck) become visibly active, and in extreme situations, the patient may begin a gasping type of respiratory pattern.
Less typically, a patient with asthma may complain of intermittent episodes of non-productive cough or breathlessness on exertion. Children most often experience these symptoms of Asthma and they tend to interfere with daily activities, sports, and games.
Diagnosis
Physical exam-
- To rule out other possible conditions — such as a respiratory infection or chronic obstructive pulmonary disease (COPD) — your doctor will do a physical exam and ask you questions about your signs and symptoms and about any other health problems.
Tests to measure lung function
You may also be given lung (pulmonary) function tests to determine how much air moves in and out as you breathe. These tests may include:
- Spirometry. This test estimates the narrowing of your bronchial tubes by checking how much air you can exhale after a deep breath and how fast you can breathe out.
Peak flow. A peak flow meter is a simple device that measures how hard you can breathe out. Lower than usual peak flow readings are a sign your lungs may not be working as well and that your asthma may be getting worse. Your doctor will give you instructions on how to track and deal with low peak flow readings.
Lung function tests often are done before and after taking a medication called a bronchodilator, such as albuterol, to open your airways. If your lung function improves with the use of a bronchodilator, it’s likely you have asthma.
Additional tests
Other tests to diagnose asthma include:
1. Methacholine challenge- Methacholine is a known asthma trigger that, when inhaled, will cause mild constriction of your airways. If you react to the methacholine, you likely have asthma. This test may be used even if your initial lung function test is normal.
2. Nitric oxide test-This test, though not widely available, measures the amount of the gas, nitric oxide, that you have in your breath. When your airways are inflamed — a sign of asthma — you may have higher than normal nitric oxide levels.
3. Imaging tests- A chest X-ray and high-resolution computerized tomography (CT) scan of your lungs and nose cavities (sinuses) can identify any structural abnormalities or diseases (such as infection) that can cause or aggravate breathing problems.
4. Allergy testing-This can be performed by a skin test or blood test. Allergy tests can identify allergies to pets, dust, mold, and pollen. If important allergy triggers are identified, this can lead to a recommendation for allergen immunotherapy.
5. Sputum eosinophils- This test looks for certain white blood cells (eosinophils) in the mixture of saliva and mucus (sputum) you discharge during coughing. Eosinophils are present when symptoms develop and become visible when stained with a rose-colored dye.
6. Provocative testing- for exercise and cold-induced asthma. In these tests, your doctor measures your airway obstruction before and after you perform vigorous physical activity or take several breaths of cold air.
PREVENTIVE TREATMENTS OF BRONCHIAL ASTHMA-
Avoid your triggers
Taking steps to reduce your exposure to asthma triggers is a key part of asthma control, including:
USE YOUR AIR CONDITIONER- Air conditioning reduces the amount of airborne pollen from trees, grasses, and weeds that find their way indoors. Air conditioning also lowers indoor humidity and can reduce your exposure to dust mites. If you don’t have air conditioning, try to keep your windows closed during the pollen season.
DECONTAMINATION YOUR DECOR- Minimize dust that may worsen nighttime symptoms by replacing certain items in your bedroom. For example, encase pillows, mattresses, and box springs in dustproof covers. Remove carpeting and install hardwood or linoleum flooring. Use washable curtains and blinds.
MAINTAIN OPTIMAL HUMIDITY- If you live in a damp climate, talk to your doctor about using a dehumidifier.
PREVENT MOLD SPORES- Clean damp areas in the bath, kitchen, and around the house to keep mold spores from developing. Get rid of moldy leaves or damp firewood in the yard.
REDUCE PET DANDER- If you’re allergic to dander, avoid pets with fur or feathers. Having pets regularly bathed or groomed also may reduce the amount of dander in your surroundings.
Clean regularly Clean your home at least once a week. If you’re likely to stir up dust, wear a mask or have someone else do the cleaning.
Cover your nose and mouth if it’s cold out. If your asthma is worsened by cold or dry air, wearing a face mask can help.
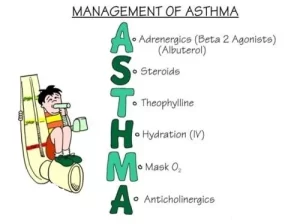
Treatment
Prevention and long-term control are key to stopping asthma attacks before they start. Treatment usually involves learning to recognize your triggers, taking steps to avoid them, and tracking your breathing to make sure your daily asthma medications are keeping symptoms under control. In case of an asthma flare-up, you may need to use a quick-relief inhaler, such as albuterol.
MEDICATIONS-
The right medications for you depend on a number of things — your age, symptoms, asthma triggers, and what works best to keep your asthma under control.
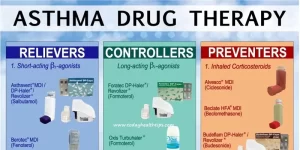
Preventive, long-term control medications reduce the inflammation in your airways that leads to symptoms. Quick-relief inhalers (bronchodilators) quickly open swollen airways that are limiting breathing. In some cases, allergy medications are necessary.
Long-term asthma control medications, generally taken daily, are the cornerstone of asthma treatment. These medications keep asthma under control on a day-to-day basis and make it less likely you’ll have an asthma attack. Types of long-term control medications include:
INHALED CORTICOSTEROIDS- These anti-inflammatory drugs include fluticasone, budesonide, flunisolide, ciclesonide, beclomethasone, mometasone, and fluticasone furoate.
You may need to use these medications for several days to weeks before they reach their maximum benefit. Unlike oral corticosteroids, these corticosteroid medications have a relatively low risk of side effects and are generally safe for long-term use.
LEUCOTRIEN MODIFIERS – These oral medications — including montelukast, zafirlukast, and zileuton — help relieve asthma symptoms for up to 24 hours.
In rare cases, these medications have been linked to psychological reactions, such as agitation, aggression, hallucinations, depression, and suicidal thinking. Seek medical advice right away for any unusual reaction.
LONG-ACTING BETA AGONIST- These inhaled medications, which include salmeterol and formoterol, open the airways.
Some research shows that they may increase the risk of a severe asthma attack, so take them only in combination with an inhaled corticosteroid. And because these drugs can mask asthma deterioration, don’t use them for an acute asthma attack.
COMBINATION INHALERS- These medications — such as fluticasone-salmeterol, budesonide-formoterol, and formoterol-mometasone — contain a long-acting beta agonist along with a corticosteroid. Because these combination inhalers contain long-acting beta agonists, they may increase your risk of having a severe asthma attack.
THEOPHYLIN- Theophylline is a daily pill that helps keep the airways open (bronchodilator) by relaxing the muscles around the airways. It’s not used as often now as in past years.
Quick-relief medications are used as needed for rapid, short-term symptom relief during an asthma attack — or before exercise if your doctor recommends it. Types of quick-relief medications include:
SHORT ACTING BETA-AGONIST- These inhaled, quick-relief bronchodilators act within minutes to rapidly ease symptoms during an asthma attack. They include albuterol and levalbuterol .
SHORT ACTING BETA-AGONIST- can be taken using a portable, hand-held inhaler or a nebulizer — a machine that converts asthma medications to a fine mist — so that they can be inhaled through a face mask or a mouthpiece.
IPRATROPIUM – Like other bronchodilators, ipratropium acts quickly to immediately relax your airways, making it easier to breathe. Ipratropium is mostly used for emphysema and chronic bronchitis, but it’s sometimes used to treat asthma attacks.
ORAL AND INTRAVENOUS CORTICOSTEROIDS- These medications — which include prednisone and methylprednisolone — relieve airway inflammation caused by severe asthma. They can cause serious side effects when used long-term, so they’re used only on a short-term basis to treat severe asthma symptoms.
If you have an asthma flare-up, a quick-relief inhaler can ease your symptoms right away. But if your long-term control medications are working properly, you shouldn’t need to use your quick-relief inhaler very often.
Keep a record of how many puffs you use each week. If you need to use your quick-relief inhaler more often than your doctor recommends, see your doctor. You probably need to adjust your long-term control medication.
Allergy medications may help if your asthma is triggered or worsened by allergies. These include:
ALLERGY SHOTS (immunotherapy)- Over time, allergy shots gradually reduce your immune system’s reaction to specific allergens. You generally receive shots once a week for a few months, then once a month for a period of three to five years.
OMALIZUMAB (Xolair)- This medication, given as an injection every two to four weeks, is specifically for people who have allergies and severe asthma. It acts by altering the immune system.
PHYSIOTHERAPY MANAGEMENT-
The majority of patients suffering from asthma will seek physiotherapy for dyspnoea and hyperventilation. Physiotherapists treat in a variety of ways with the aim to improve breathing techniques. Physiotherapy techniques for asthma are in addition to medication and should never be used as a replacement for prescribed medication, however, may reduce the dosage required.
Breathing Techniques
1. BREATHING RETRAINING TECHNICS –
Breathing techniques may have more benefit on mild–moderate asthma. The aim of breathing retraining is to normalize breathing patterns by stabilizing respiratory rate and increasing expiratory airflow. Instructions are given by the physiotherapist on how to complete this technique, with the following components:
- Decreasing Breaths Taken (Reducing Respiratory Rate)
- Taking Smaller Breaths (Reducing Tidal Volume)
- Deep Breathing (Diaphragmatic breathing through the use of abdominal muscles and lower
- thoracic chest movement)
- Breathing through the Nose (Nasal Breathing)
- Relaxation (Relaxed, controlled breathing)
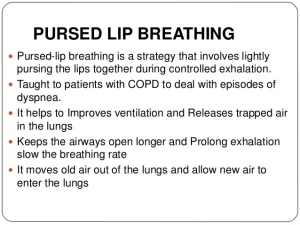
- Decreasing Air Leaving (Decreased expiratory flow through pursed lip breathing)
- These retraining techniques help control breathing and reduce airflow turbulence,
- hyperinflation, variable breathing patterns,s, and anxiety.
2. BUTEYKO BREATHING TECHNIQUE –
The Buteyko breathing technique is another breathing retraining technique; however, it is specific to reducing hyperinflation. It was developed based on the theory that asthmatic bronchospasm is caused by hyperventilation, leading to a low PaCO2 and therefore all asthmatic symptoms are due to this. The narrowed airways induce an “air hunger” causing a switch to mouth-breathing and an increased respiratory rate leading to hyperinflation. Buteyko believes that this hyperinflation then also contributes to bronchoconstriction. The Buteyko technique aims to reduce ventilation and subsequently lung volume, as a treatment for asthma and other respiratory diseases. A qualified practitioner is necessary to train the patient.
The Buteyko breathing Technic
- Breathe normally through the nose for 2-3 mins
- Breathe out normally, close your nose with your fingers, and hold
- Record number of seconds
- On the first need to breathe, release the nose and return to nasal breathing (Control Pause)
- Wait 3 minutes
- Repeat and hold your breath for as long as possible (Maximum Pause)
Breathing pattern retraining and relaxed breathing techniques are two approaches to physiotherapy management of asthma. The aim of breathing pattern retraining is to develop a more efficient pattern of respiration, thereby reducing breathlessness. This is usually accomplished by slowing the breathing rate and encouraging relaxed, ‘abdominal’ breathing (Bruton, 2006). Another potential mechanism for breathing pattern retraining is that by encouraging a longer expiratory time, the effects of any static/ dynamic hyperinflation may be reduced.
Mild asthmatics can hold their breath for up to twenty seconds, moderate asthmatics for fifteen seconds, and severe asthmatics for up to ten seconds. The aim of this method is to increase the control pause to 60 seconds and the maximum pause to 2 minutes. It is practiced twice a day, with the practitioner there to help with breath holding and ensure safety. Its aim is to reduce minute volume through reduction of respiratory rate, and increasing carbon dioxide levels through breath holding, reducing bronchospasm caused by hyperventilation in the asthmatic patient.
3 PHYSICAL TRAINING-

Physical training with asthma is advised when taking the proper precautions, and should not be avoided. The American College of Sports Medicine (ACSM) Guidelines provide tips and safety precautions for asthmatics to exercise safely.
Physical training should be prescribed by physiotherapists for asthmatics to increase fitness and cardiorespiratory performance, reduce symptoms such as breathlessness and improve quality of life. Breathlessness, chest tightness and wheezing can occur when exercising, deterring patients from physical exertion . Fear avoidance can contribute to a further deterioration of physical health and quality of life, leading to anxiety and depression. It has been shown that maintaining physical training in asthmatics improves disease symptoms and quality of life, therefore making it a crucial management strategy.
4 RESPIRATORY MUSCLE TRAINING-
Hyperinflation in asthma causes increased lung volume, leading to altered inspiratory muscle mechanics. Inspiratory muscles are shortened resulting in a sub-optimal length-tension relationship for contraction. There is a decreased capacity for tension generation when breathing, resulting in accessory muscles of inspiration being utilised.
Breathing exercises are carried out using an external device to make breathing more difficult. This helps to strengthen the inspiratory muscles, making it easier to breathe in everyday life .A breathing device is used , which sets up a load to breathe against. During inspiration air is only released if enough effort is used to force open the valves of the device. Respiratory muscles are forced to work harder, increasing their strength, leading to diaphragmatic breathing becoming easier, reducing hyperinflation.
The following physiotherapy management techniques would also be beneficial:
Removal of secretions
- Percussions
- Shaking
- Vibrations
- Postural drainage
- Effective coughing
- Range of motion exercises for patients who need hospitalization.




27 Comments