Sinus tarsi syndrome : Physiotherapy Treatment
What is sinus tarsi syndrome?
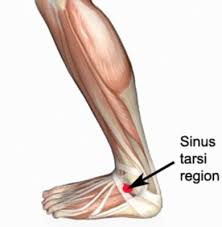
Sinus tarsi syndrome is a condition that affects the sinus tarsi, or the area on the inner side of the ankle joint. It is characterized by pain in this area. This pain can be exacerbated by weight bearing activities, such as walking or running. There are several possible causes for this condition, including overuse or stress on tendons and joints, as well as high arches in the foot.
Definition :
The sinus tarsi is a tube or tunnel between the talus and the calcaneus bones. Sinus tarsi syndrome is pain or injury to this area.
Traumatic injury to the ankle/foot (such as an ankle sprain) or overuse (such as repetitive standing or walking) are the main causes of this syndrome.
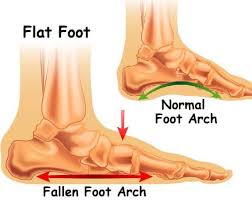
It may also occur if the person has a pes planus or an over-pronated foot, which can cause compression in the sinus tarsi.
Some characteristics are pain at the anterior lateral side of the ankle (anterior to the lateral mallelous) and a feeling of instability or difficulty walking on unstable surfaces.
Recent discussions of sinus tarsi syndrome (STS) describe this entity as primarily an instability of the subtalar joint due to ligamentous injuries that results in a synovitis and infiltration of fibrotic tissue into the sinus tarsi space .
Anatomy and bio-mechanics :
The sinus tarsi has been compared with the intercondylar fossa of the knee, and forms part of the subtalar joint complex.
The sinus tarsi is the opening of the talocalcaneal sulcus, which is shaped like a long funnel.
It has a large anterolateral opening, narrowing down to a smaller posteromedial opening.
The anterior opening is found anterior and inferior to the lateral malleolus, while the posterior opening sits behind the sustentaculum tali below the medial malleolus.
The inside of the sinus tarsi tunnel is filled with a host of numerous structures.
These include :
The large interosseous talocalcaneal ligament (ITCL)– The medial band of the ITCL is a single fibrous band.
The lateral half splits into two bands, which are separated by a vascular and innervated adipose tissue.
The ITCL is taut in supination and relaxed in pronation.
Adipose tissue– Serves as a bedding for numerous mechanoreceptors and free nerve endings, which along with the ligaments and muscles provide proprioceptive information on the movement of the foot and ankle.
The inferior part of the extensor retinaculum (IER) –This lies over the lateral opening and serves as a covering to the sinus tarsi.
The extensor digitorum brevis muscle– Attaches to the medial and distal aspect of the sinus tarsi, running over the calcaneocuboid joint towards the toes.
The cervical ligament (CL).
A synovial membrane– Surrounds the sinus tarsi
The main ligament is the ITCL. This is a wide and very strong ligament that originates from a broad attachment in the middle of the canal on the surface of the calcaneus and runs anteromedially to the deepest portion of the tarsal canal, where it inserts on the talus.
The CL is a smaller band, which has its origin on the lateral calcaneus, just medial to the attachment of the extensor retinaculum of the foot, and passes medially through the centre of the canal as it inserts on the talus .
A recent study published described new findings on the anatomical relationship between the capsules and each ligamentous structure of the subtalar joint.
It demonstrated (in a cadaveric study) that the tarsal canal and sinus consisted of three structured layers :
1) The anterior capsule of the posterior talocalcaneal joint, including the anterior capsular ligament.
2) The interosseous talocalcaneal ligament (ITCL) and inferior extensor retinaculum (IER) layers
3) The posterior capsule of the talocalcaneonavicular joint, including the cervical ligament (CL).
The tarsal canal ligaments maintain alignment between the talus and calcaneus and limit inversion.
The main stabilising ligament of the lateral ankle is the calcaneofibular ligament.
In addition, the ITCL is taut when the foot is supinated, and the CL helps resist hindfoot varus forces.
With inversion trauma, the ligaments are usually injured in the following order:-
anterior talofibular ligament (ATFL), calcaneofibular ligament (CFL), CL, and ITCL.
The more severe the injury, the more of these ligaments are injured.
Thus, tarsal canal ligament injury never occurs as an isolated lesion with an inversion sprain; it will also be associated with damage to the ATFL and/or the CFL.
Pathogenesis :
The syndrome known as STS was first described by O’Connor in 1958(5)and the true incidence of STS is unknown.
STS has been associated with ankle sprains that may also result in talocrural joint instability.
Some key findings between the correlation of ankle sprain and STS include:-
10-25% of patients with chronic talocrural joint instability will also have subtalar joint instability.
Nine out of twelve patients with recurrent ankle sprains had signs of increased talocrural and subtalar joint motions upon a radiographic examination.
Previous inversion sprain has been found in 70% of STS sufferers(8-10).
Due to the abundance of synovial tissue, the sinus tarsi is prone to synovitis and inflammation when injured. Injury to the sinus tarsi falls into three broad categories:
- An inversion injury to the ankle that also injures the sinus tarsi.
These injuries cause instability of the subtalar joint resulting in excessive supination and pronation movements.
The excessive movement of the subtalar joint imparts increased forces onto the synovium of the subtalar joint and across the sinus tarsi tissues.
The excessive forces result in subtalar joint synovitis with chronic inflammation and infiltration of fibrotic tissues in the sinus tarsi, which are responsible for the characteristic anterolateral ankle pain of STS.
2. Chronic inflammation due to excessive bouts of pronation.
3. Repeated forced eversion under impact load such as jumping.
This mechanism is thought to create a ‘whiplash injury’ to the rearfoot, with the talus moving anteriorly over the calcaneus.
Signs and symptoms :
- This syndrome are pain at the lateral side of the ankle.
- The pain is most severe when standing, walking on uneven ground or during the movements of supination and adduction of the foot’.
Because the pain usually presents months after an injury to the lateral ankle ligaments, STS is often misdiagnosed, and STS may often simply be confused with chronic ankle instability.
People suffering from the sinus tarsi syndrome also have a feeling of instability (functional instability) in the hind foot .
Moreover the loss of stability in the ankle will allow a greater range of motion to the subtalar joint.
This excessive movement will increase the forces onto the synovium and across the sinus tarsi.
The subtalar joint synovitis, which is responsible for chronic inflammation and infiltration of fibrotic tissues in the sinus tarsi, results in ankle pain.
The subtalar joint synovitis, which is responsible for chronic inflammation and infiltration of fibrotic tissues in the sinus tarsi, results in ankle pain.
Furthermore, those injuries can also damage ligaments of the tibiotalar and talocalcaneal joints and increase the mobility between the talocrural and subtalar joints.
Some of the features that may alert the practitioner that the patient has a STS include .
Vague and poorly localised anterolateral ankle pain.
Because the synovitis and fibrotic tissues associated with STS will take time to develop, athletes with injuries to the subtalar joint may not initially have symptoms that can be localised to the sinus tarsi.

Morning pain that usually subsides with use.
Pain running on a curve in the direction of the affected ankle.
Feeling of ankle and foot stiffness.
Feeling of instability and weakness of the ankle.
Athletes involved with cutting and jumping activities on firm surfaces will have the greatest difficulty with subtalar instability as these activities will cause excessive movements of the subtalar joint to the end ranges of pronation and supination.
Difficulty walking on uneven ground.
Pain on palpation and localised swelling over the sinus tarsi opening in the anterolateral ankle.
Normal talocrural movement but stiff subtalar joint movements.
Pain of forced eversion of the subtalar joint.
What causes sinus tarsi syndrome?

The sinus tarsi syndrome mainly occurs after a traumatic lateral ankle sprain or multiple ankle sprains (mostly due to a weak anterior talofibular ligament) which leads to injuries of the interosseus and cervical ligaments.
The ligaments of the sinus tarsi can be sprained or torn, and inflammation and hemorrhage of the synovial recess in the sinus tarsi can occur.
This happens in 70% of the cases.
This pathology is mostly a result of synovitis and infiltration of fibrotic tissue into the sinus tarsi space due to an instability of the subtalar joint, caused by ligamentous injuries.
The sinus tarsi syndrome can also occur as a compression injury, for example to people who have flat or pronated feet. The talus and calcaneus are pressed together as a result of the deformation.
This causes bone to bone contact of the talus and calcaneus, with inflammation or arthritis in the sinus.

Other Causes :

- Cysts
- Degenerative changes (progressive and often irreversible deterioration; loss of function in the tissues)
- Injury to the extensor digitorum brevis muscle (a muscle located on the top of the foot)
- A severely pronated foot: Note that pronation of the foot is a natural movement that occurs when the foot lands during running or walking. However, when a person overpronates the foot, it can cause pressure on the sinus tarsi. This can result in sinus tarsi syndrome. The treatment for overpronation involves orthotics (special shoes) that can help control the motion of the foot.
Examination :
A full ankle examination is required and it should be compare with the other ankle.
An acute ankle injury will typically present with pain accompanied by swelling, ecchymosis (discolourisation caused by bruising), and tenderness in the anterolateral ankle.
Because the synovitis and fibrotic tissues associated with STS will take time to develop, athletes with injuries to the subtalar joint may not initially have symptoms that can be localized to the sinus tarsi.
Stability of the subtalar joint is assessed with medial and lateral subtalar joint glides performed by moving the calcaneus over a stabilized talus in the transverse plane and with subtalar joint distraction.
In standing posture the patients may demonstrate a pes planus posture or an asymmetry of the rearfoot angle with the leg.
In passive examination, the range of motion of the ankle may be limited in pronation and supination, but pain over the sinus tarsi at the end range of plantar flexion combined with supination is a typical sign for STS.
The subtalar joint may have increased translation mobility if the interosseous and cervical ligaments are disrupted, but this is not always the case.
The therapist should examine the talocrural and subtalar joints for signs of hypermobility as injuries can affect both of these important articulations of the lower extremity.
Localized ankle discomfort to the sinus tarsi space and feelings of instability with pronation and supination movements of the subtalar joint will help identify STS.
The therapist should also evaluate if there is any muscle weakness of the peroneal and plantar flexor muscles.
This is done with resistance tests of the ankle: pronation tests and flexion tests.
There is a stability test that is thought to recreate instability of the subtalar joint.
The test is performed with the athlete in supine with the ankle in 10 degrees of dorsiflexion to keep the talocrural joint in a stable position.
The forefoot is first stabilized by the examiners hand, while an inversion and internal rotational force is applied to the calcaneus.
Then an inversion force is applied to the forefoot.
The examiner assesses for an excessive medial shift of the calcaneus and a reproduction of the athlete’s complaint of instability and symptoms.
Differential Diagnosis:
These common pathologies may give the same pain characteristics or symptoms:
- Ankle sprain
- Calcaneal fracture
- Talar fracture
- Peroneal tendonitis
- Subtalar joint arthritis
- Tarsal tunnel syndrome
Localization of pain to the sinus tarsi with the presence of ankle instability is a good indication that the patient has developed STS.
The diagnosis of STS has typically been confirmed by the cessation of symptoms upon injection of lidocaine into the sinus tarsi.
Diagnosis :
Diagnosis of Sinus Tarsi Syndrome may involve:
X-rays

A bone scan
A CT Scan
An MRI (reveals changes in the soft tissue of the sinus tarsi such as scar tissue from previous injuries)

An injection with a local anesthetic (to help the healthcare provider locate the area of the problem)
An ankle arthroscopy (a narrow tube attached to a fiber-optic video camera, inserted through a very small incision [the size of a buttonhole], to view and diagnose joint problems)
Ruling out other problems of the foot
How do you treat sinus tarsi syndrome?
The Treatment are divided mainly into 3 parts, Medical Treatment, Physiotherapy treatment and exercise and if conservative treatment is fails 3rd option is Surgical treatment.
Medical Treatment :
The treatment of the sinus tarsi syndrome can be conservative or operative.
The first one includes physiotherapy treatment with injections with corticosteroids in the sinus tarsi, local gels or drugs.
Sinus tarsi syndrome surgery :
Operative treatment is also very effective in most cases, but needs to be considered as a last resort if conservative treatment fails.
Subtalar arthroscopy is useful for the diagnosis and treatment of STS. Furthermore, subtalar arthroscopy allows for direct visualization of pathologic findings in STS.
STS can be treated by open surgery and subtalar arthroscopy when conservative treatments are ineffective. Kuwada reported a long-term treatment results of STS where all patients who underwent open excision during a 15-year period were reported to achieve 100% pain relief, and there were no complications.
Lowy et al.reported that 15 of 21 STS patients who underwent open surgery achieved complete pain relief and that the remaining 6 achieved partial relief.
Moreover, Frey et al. reported that, among STS patients, 43% had an excellent result and 43% had a good result after subtalar arthroscopy; only 3 patients (14%) had a poor result.
Thus, according to these studies, open surgery and arthroscopic treatments produce similarly satisfactory results.
Notable is that arthroscopic treatment alone resolves the symptoms of STS as well as open surgery, which involves the excision of all synovial tissue in the lateral contents of the sinus tarsi.
Subtalar arthroscopy has been reported to be associated with complications of neuritis, sinus tract formation, and superficial wound infection, although these responded to nonsurgical treatment.
Subtalar arthroscopy identified pathologies in the subtalar joint in patients with STS and showed that treatment of these pathologies led to improved function.
Given the preliminary clinical results and present degree of instrument sophistication, one would expect that the excision of an os trigonum and subtalar joint arthrodesis would evolve into mainstay procedures.
Moreover, as the definitive value of thermally induced capsule-ligamentous shrinkage is established, the possibility of addressing subtalar instability may be envisioned.
Physiotherapy Treatment :
Since the STS often occurs after an ankle sprain, the foot has been immobilized by a brace or tape during recovery of the joint and the ligaments.
Therefore mobilization of the ankle, especially of the subtalar and talocrural joint is necessary in the treatment of STS.
Joint mobilization exercises should be done in all directions, but especially in pro- and supination.
Also important is they should be executed at full range of motion, provided there is no pain provocation.
“’No random control trials for the efficacy of a rehabilitation program for STS are available’.
To influence the tissues in the sinus tarsi, the therapy may consist of friction massages, electrotherapy (for example ultrasound), laser-therapy, cryotherapy and other types of deep massages.
The use of ice massage over the lateral ankle may be useful to diminish inflammation and pain .
Activities should be started as soon as possible, if they can be done without pain.
As the peroneal muscles and Achilles tendon tend to weaken when having sinus tarsi, it’s vital to adjust a program therapy to reinforce those muscles.
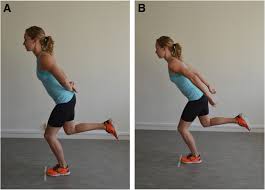
Flexion of the ankle by standing on the toes is a good exercise, and when done on the edge of a stair eccentric exercises can be done for a better strength gain.
Stability training is the last stage of rehabilitation.
The patient must do proprioceptive exercises, for example lunges, to improve the proprioception and stability in the ankle.
Training programs to improve the stability of the subtalar joint and lower extremity function will be the hallmark of treatment plans for STS.
Joint stability relies on passive joint structures, dynamic muscular responses, and neurological control.
The treatment program of STS includes proprioceptive training, balance training, taping and bracing, muscle strengthening exercises and orthese.
Some athletes have synovitis of the joint and anti-inflammatory medication would be helpful to reduce the inflammation. Ice on the affected area can help too.
Orthoses :

Stability of the subtalar joint may be initially improved with the use of an orthosis.
Ankle braces intended for CAI may be useful for some athletes with STS, but the overall design of these braces may not significantly improve the stability of the subtalar joint during athletic activities.
Foot orthosis have also been recommended as a method for limiting motion at the subtalar joint and reducing symptoms associated with STS.
The types of shoes the athlete is using for training, practice, and competition should also be considered, as well-constructed shoes can restrict excessive rearfoot movements.
General recommendations for shoes include those with a straight last, a firm heel counter, and rigid material through the midsole.
Shoes should also be assessed for wear, as materials within a shoe will begin to break down before the external material show signs of deterioration.
The use of a foot orthosis with an athletic shoe should be considered together, as the effect of an orthosis can be inconsistent.
An ongoing assessment of shoe and orthosis use is needed to provide adequate support for the foot and ankle throughout an athlete’s cycle of training and competition.
Taping or strapping has also been used to specifically limit movements of the subtalar joint and the midfoot.
Wilkerson et al have described a taping procedure that combines a closed basket weave with a subtalar sling to control movements at the talocrural and subtalar joints.
Viczenzio et al37 have described a modified Low-Dye taping method that uses a calcaneal sling intended to provide support to the medial longitudinal arch of the foot.
This method could be used to control or reduce the amount of pronation through the subtalar joint during walking and running activities.
Taping techniques have been used as a precursor for the use and selection of specific types of shoes and foot orthotics.
An external file that holds a picture, illustration, etc.
Sinus tarsi syndrome exercises.
Stability Training :
Training programs to improve the stability of the subtalar joint and lower extremity function will be the hallmark of treatment plans for STS.
Joint stability relies on passive joint structures, dynamic muscular responses, and neurological control.
Because tears or ruptures of the interosseous and cervical ligaments of the subtalar joint are believed to be the essential lesions that lead to STS, the dynamic muscular responses and neurological control of the rearfoot will need to be emphasized to compensate for the loss of passive stability .
The muscles that cross the subtalar joint are important for maintaining stability, as they act as force transducers to guide and control the pronation and supination motions of the subtalar joint.
The relative strength of these muscles is important, but their reaction time to joint perturbations and the ability to work in a coordinated fashion is even more important for the rehabilitation of STS.
Dynamic stability will also rely on the proprioceptive information from the muscle spindles and Golgi tendon organs of these muscles to compensate for the lack of proprioceptive information from the stabilizing ligaments of the joint.
The endurance of the muscles will also be important to maintain stability during long bouts of exercise or sports activities.
Training programs to improve joint stability have been described as multiphase processes that start the athlete at an appropriate level of activity and progresses to higher levels of activities while maintaining joint stability.
To help the athlete understand this process the progression of three phases are called:-
– Attain,
-Maintain, and
-Sustain.
The Attain phase will determine postures or positions the athlete is able to attain in a stable fashion.
The Maintain phase will develop coordinated isometric and eccentric muscle contractions of the muscles crossing the joint.
The Sustain phase will involve integrating all of the neuromuscular subsystems needed for stability during sports specific activities.
Attain stage :
Activities :
Single leg standing – Eyes open and closed.

Criteria for Progression :
Athlete demonstrates ability to attain a stable position through the foot and ankle.
Maintain stage :
Activities :
Single leg standing – Hip swings, and Star pattern reaching .Heel raises, oscillation with theraband, and impulse with medicine ball.


Criteria for Progression :
Athlete demonstrates ability to maintain stability and good alignment through the lower extremities.
Sustain stage :
Activities :-
Lunges and step down exercises


Bilateral and single-leg hops
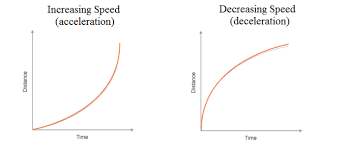
Forward and backward acceleration and deceleration
Pivoting and cutting maneuvers
Criteria for Progression :
Athlete demonstrates the ability to tolerate loading and pushing-off the involved lower extremity.
The Attain phase for subtalar joint instability is usually started with the athlete in standing positions.
The clinician should closely observe the arch of the foot and rear-foot to assess the athlete’s ability to attain a stable position for the subtalar joint while avoiding excessive pronation movements.
Single leg standing, with the contralateral limb held in approximately 30 degrees of hip flexion and 90 degrees of knee flexion, will emphasize ankle balance strategies.
The Attain phase begins with the eyes open and attempting to hold the single leg position for 30 to 60 seconds with minimal alterations in body position.
Once the athlete is able to hold a single leg standing position consistently, a progression to eyes closed conditions can be made.
The second phase, Maintain, is performed with perturbations to the single leg positions.
Perturbation forces are imparted near the level of the athlete’s center of gravity to replicate the type of forces that produce subtalar joint instability during athletic activities.
The perturbating forces are intended to facilitate rapid isometric and eccentric contractions of the stabilizer muscles of the ankle.
Perturbations to standing balance are begun with movements from the contralateral hip starting in the sagittal and coronal planes of motion, progressing to transverse plane motions.
Observations of the athlete’s rearfoot and hip stability will indicate his/her ability to maintain this position.
The clinician needs to insure that the athlete is not using excessive compensatory motions at the rearfoot or hip to maintain a single leg standing position.
The star excursion balance test activities can also be used in this phase, with the athlete in the single leg standing position and touching different lines drawn on the floor in a star pattern.
Standing heel raises and lowering exercises can be performed at a slow speed in double leg and single leg standing.
Emphasis is placed on promoting controlled concentric and eccentric muscle contraction of the ankle plantarflexors and subtalar joint pronator muscles .
External perturbations can be imparted with the athlete holding a two-foot length of theraband.
With both hands in front of the umbilicus, the therapist can then pull on the theraband with oscillating motions.
Catching and throwing a small ball or medicine ball while in single leg standing can also be used for perturbations in multiple directions and different timing .
The Sustain phase will begin with the athlete learning to “close the chain” meaning moving from an open kinematic chain to a stable closed kinematic chain position.
The emphasis is on developing the feedforward motor control of the lower extremities.
This activity can be started by having the athlete perform lunging steps and then stepping down from a 4 or 8 inch step onto the involved extremity into a single leg standing position.
Progression can be to lateral lunge steps and lateral step downs.
Observations of the athlete’s overall control of motion through the lower extremities with an emphasis on alignment of the knee and foot will insure that excessive subtalar joint motion is not occurring.
Progressions of the Sustain phase can be performed with the athlete jumping or hopping in place and then into hopping in different directions.
Running activities can begin by acceleration and deceleration with forward and backward motions.
Athletes needing to perform pivoting or cutting maneuvers can begin these activities at a slow speed maintaining good alignment of the foot and leg and avoiding excessive motions through the rearfoot.
Return to play criteria is based on the athlete’s ability to move in all directions and at appropriate speeds.
Athletes performing cutting and jumping maneuvers on firm surfaces, such as basketball and volleyball players, should be returned to full activities over a period of days to insure their tolerance to these stressful maneuvers.
A progression of the athletic activities should be assessed with the athlete in his or her normal practice or competitive environment.
The athlete’s anterolateral ankle symptoms will need to be well controlled to insure that the return to competition will not create chronic inflammation of the sinus tarsi tissues.




6 Comments