Pseudo-boutonniere Deformity
What is a Pseudo-boutonniere deformity?
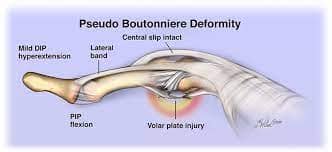
Pseudo-boutonniere deformity, also known as “pseudo-boutonniere,” is a hand deformity that resembles the classic boutonniere deformity but has different underlying causes and mechanisms. The condition involves the abnormal positioning of the fingers, typically affecting the middle joint of the finger (proximal interphalangeal joint or PIP joint) and the distal interphalangeal joint (DIP joint).
In a classic boutonniere deformity, the PIP joint is flexed, and the DIP joint is hyperextended due to an injury to the central slip of the extensor tendon. However, in the case of a pseudo-boutonniere deformity, the PIP joint is hyperextended (extended) and the DIP joint is flexed.
Causes of Pseudo-boutonniere Deformity:
- Rheumatoid Arthritis: The most common cause of pseudo-boutonniere deformity is rheumatoid arthritis, an autoimmune condition that affects the joints, causing inflammation, deformities, and joint destruction.
- Trauma: Finger injuries, such as forced hyperextension or axial loading, can lead to pseudo-boutonniere deformity.
- Tendinitis or Tenosynovitis: Inflammation of the extensor tendon or the tendon sheath may lead to deformity.
- Other Inflammatory Conditions: Conditions like psoriatic arthritis or systemic lupus erythematosus can also contribute to the development of pseudo-boutonniere deformity.
Symptoms:
Symptoms of pseudo-boutonniere deformity may include pain, swelling, limited range of motion, and a noticeable change in finger alignment.
Pseudo-boutonniere deformity is characterized by specific symptoms related to the abnormal positioning of the finger joints. The deformity primarily affects the middle joint of the finger, known as the proximal interphalangeal joint (PIP joint), and the end joint of the finger, known as the distal interphalangeal joint (DIP joint). The main symptoms of pseudo-boutonniere deformity include:
- Hyperextension of the PIP Joint: The PIP joint is abnormally bent backward, causing it to hyperextend. This means that the middle joint of the finger appears to be pushed back and straightened, rather than bending in its normal range.
- Flexion of the DIP Joint: The DIP joint is flexed, meaning it is abnormally bent forward. This creates a finger deformity in which the fingertip bends downward toward the palm.
- Finger Pain: Pseudo-boutonniere deformity may be accompanied by pain in the affected finger, especially when attempting to move the finger or performing activities that involve gripping or grasping.
- Swelling: The finger may appear swollen due to inflammation in the affected joints and surrounding tissues.
- Limited Range of Motion: The affected finger may have restricted movement due to abnormal joint positioning and potential joint inflammation.
- Functional Impairment: The deformity can lead to difficulties with fine motor tasks and decreased hand function, affecting daily activities like writing, typing, or gripping objects.
- Redness and Warmth: In cases related to underlying inflammatory conditions like rheumatoid arthritis, there may be redness and warmth around the affected joint.
It is important to note that the symptoms of pseudo-boutonniere deformity can vary in severity depending on the underlying cause and the extent of joint damage. If you notice any of these symptoms or suspect you have a finger deformity, it is essential to seek medical evaluation from a healthcare professional, such as a hand surgeon or a rheumatologist, for proper diagnosis and appropriate treatment. Early intervention can help prevent further joint damage and improve outcomes.
Differential Diagnosis
In medicine, a differential diagnosis is the process of considering and evaluating various potential medical conditions or diseases that could be causing a patient’s symptoms. It involves comparing and contrasting the clinical features of different conditions to arrive at the most likely explanation for the patient’s presentation. A comprehensive and accurate differential diagnosis is crucial for appropriate and timely treatment.
When it comes to pseudo-boutonniere deformity, the condition itself is a specific deformity of the finger joints. However, it is essential to differentiate it from other hand and finger conditions that may present with similar symptoms. Here are some conditions that could be included in the differential diagnosis of pseudo-boutonniere deformity:
- Classic Boutonniere Deformity: The classic boutonniere deformity is the opposite of the pseudo-boutonniere deformity. In the classic boutonniere deformity, the middle joint of the finger (PIP joint) is flexed, and the end joint (DIP joint) is hyperextended due to an injury to the central slip of the extensor tendon.
- Rheumatoid Arthritis (RA): RA is an autoimmune disease that primarily affects the joints, causing inflammation, pain, and deformities. It can lead to pseudo-boutonniere deformity as well as swan-neck deformity (flexion at the DIP joint and hyperextension at the PIP joint).
- Osteoarthritis (OA): OA is a degenerative joint disease that can affect the finger joints, leading to pain, swelling, and deformities. Bony enlargement and loss of joint space may be seen on X-rays.
- Psoriatic Arthritis: This is a type of inflammatory arthritis that can occur in people with psoriasis. It can lead to joint pain, swelling, and deformities similar to those seen in RA.
- Trauma: Finger injuries, such as fractures, dislocations, or tendon injuries, can cause deformities and pain in the fingers.
- Flexor Tendon Injuries: Injuries to the flexor tendons in the fingers can result in deformities that resemble boutonniere deformity.
- Dupuytren’s Contracture: This condition involves the thickening and contracture of the palmar fascia, leading to finger flexion contractures.
- Systemic Lupus Erythematosus (SLE): SLE is an autoimmune disease that can cause joint inflammation and deformities, including those affecting the fingers.
- Gout: Gout is a form of arthritis caused by the accumulation of urate crystals in the joints, leading to sudden and severe joint pain and swelling.
- Infectious Arthritis: Bacterial, viral, or fungal infections can cause joint inflammation and deformities in the fingers.
- Tendinitis or Tenosynovitis: Inflammation of the tendons or tendon sheaths in the fingers can lead to pain and finger deformities.
Proper evaluation by a healthcare professional, such as a rheumatologist or an orthopedic hand specialist, along with imaging studies like X-rays or MRI, can help differentiate between these conditions and arrive at an accurate diagnosis. Early diagnosis and appropriate management are essential to prevent further joint damage and improve patient outcomes.
Diagnosis
A healthcare professional, such as a hand surgeon or a rheumatologist, will diagnose the condition by assessing the physical appearance of the finger, reviewing the patient’s medical history, and possibly conducting imaging tests like X-rays.
Treatment:
Treatment for pseudo-boutonniere deformity aims to address the underlying cause and improve finger function. Depending on the severity and the specific cause, treatments may include:
- Immobilization: In less severe cases, wearing a splint or brace that keeps the PIP joint in a neutral or slightly extended position may be recommended to allow the joint to heal.
- Physical Therapy: Exercises and stretching may be prescribed to maintain joint flexibility and strength.
- Medications: Anti-inflammatory drugs or disease-modifying antirheumatic drugs (DMARDs) may be used to manage pain and inflammation associated with underlying conditions like rheumatoid arthritis.
- Corticosteroid Injections: In some cases, a corticosteroid injection into the affected joint may help reduce inflammation and relieve symptoms.
- Surgical Intervention: Severe or chronic cases, especially those due to advanced rheumatoid arthritis, may require surgical intervention to correct the deformity and restore finger function.
It is crucial for individuals experiencing finger deformities to seek medical attention promptly to receive an accurate diagnosis and appropriate treatment to prevent further damage and disability.
Physical Therapy Treatment
Physical therapy plays a crucial role in the management of pseudo-boutonniere deformity. The primary goal of physical therapy is to improve finger function, reduce pain, and increase range of motion. A physical therapist will work closely with the patient to develop a personalized treatment plan based on the specific underlying cause of the deformity and the severity of the condition. Here are some common physical therapy interventions used in the treatment of pseudo-boutonniere deformity:
- Splinting: Initially, a therapist may use a custom-made splint to maintain the PIP joint in a slightly extended position while allowing the DIP joint to flex freely. The splint helps protect the joint and prevent further deformity. The therapist will teach the patient how to properly wear and remove the splint.
- Range of Motion Exercises: Gentle and controlled exercises are used to improve finger flexibility and range of motion. These exercises may include passive and active stretching of the finger joints.
- Strengthening Exercises: Strengthening exercises for the finger extensor muscles and other hand muscles can help stabilize the joint and enhance finger function.
- Modalities: Therapeutic modalities like ultrasound, heat, or cold therapy may be used to reduce pain and inflammation in the affected finger.
- Joint Mobilization: Manual techniques may be employed by the physical therapist to mobilize the affected joint and improve its mobility.
- Activity Modification: The physical therapist may suggest modifications to daily activities and work tasks to prevent further strain on the affected finger and joint.
- Patient Education: Educating the patient about the condition, proper joint protection, and home exercises is essential to promote active participation in the rehabilitation process.
- Taping: In some cases, the therapist may apply specific taping techniques to support the finger joint and assist in correcting the deformity.
It is important to note that the success of physical therapy largely depends on the underlying cause of the pseudo-boutonniere deformity and the patient’s commitment to the treatment plan. In cases where the deformity is due to an inflammatory condition like rheumatoid arthritis, it is crucial to work closely with a multidisciplinary team, including a rheumatologist, to manage the overall condition effectively.
The physical therapist will regularly assess the patient’s progress and adjust the treatment plan as needed to ensure optimal outcomes. The length and frequency of the physical therapy sessions will vary depending on individual factors and the severity of the condition. Patients are encouraged to communicate openly with their therapist and follow the prescribed exercises and recommendations to achieve the best possible results.
How to prevent Pseudo-boutonniere deformity?
Preventing pseudo-boutonniere deformity involves taking measures to reduce the risk factors associated with its development, especially in cases related to inflammatory conditions like rheumatoid arthritis. While it may not be possible to completely eliminate the risk of developing this deformity, the following strategies can help minimize the likelihood of its occurrence:
Early Diagnosis and Treatment: If you have a known inflammatory condition like rheumatoid arthritis or any other condition affecting your finger joints, it is crucial to seek early diagnosis and appropriate medical treatment. Early intervention can help manage the underlying condition and reduce the risk of joint damage and deformities.
Regular Medical Checkups: Regularly visit your healthcare provider or rheumatologist for routine checkups, especially if you have an existing inflammatory condition. Frequent monitoring allows for timely adjustments to your treatment plan and helps prevent potential complications.
Medication Adherence: If you are prescribed medications for an inflammatory condition, such as disease-modifying antirheumatic drugs (DMARDs), biologics, or other medications, make sure to take them as directed by your healthcare provider. Adherence to medication can help control inflammation and reduce the risk of joint damage.
Hand Exercises: Engage in gentle hand exercises regularly to maintain finger flexibility and strength. Range of motion exercises and hand stretches can help keep the finger joints mobile and reduce the risk of stiffness.
Joint Protection: Be mindful of your hand and finger movements, especially during repetitive activities or tasks that put strain on the finger joints. Use proper ergonomics and hand protection to prevent excessive stress on the fingers.
Avoid Trauma: Try to avoid hand injuries, as trauma to the fingers can increase the risk of deformities. Be cautious during sports, manual labor, or any activities that may subject your fingers to sudden impacts or overextension.
Weight Management: Maintain a healthy weight to reduce unnecessary stress on the finger joints. Excess body weight can exacerbate joint problems and increase the risk of deformities.
Use Assistive Devices: If you have existing joint problems, consider using assistive devices like special grips or ergonomic tools that can reduce strain on the fingers during daily activities.
Manage Inflammation: Implement lifestyle modifications to manage inflammation, such as adopting a healthy diet rich in anti-inflammatory foods and avoiding smoking, which can worsen inflammation.
Stay Active: Regular physical activity can help maintain overall joint health and improve circulation to the fingers. However, it is essential to engage in activities that are suitable for your condition and avoid activities that exacerbate joint pain or strain.
Remember that every individual’s condition is unique, and preventive measures may vary based on specific health concerns. It is essential to work closely with your healthcare provider or a rheumatologist to develop a personalized prevention plan tailored to your needs and medical history. Early intervention and proactive measures can significantly improve the long-term outlook and quality of life for individuals at risk of developing pseudo-boutonniere deformity.
Summary
Pseudo-boutonniere deformity is a finger deformity characterized by hyperextension (extension) of the proximal interphalangeal joint (PIP joint) and flexion of the distal interphalangeal joint (DIP joint). It resembles the classic boutonniere deformity but has different underlying causes and mechanisms.
Causes of pseudo-boutonniere deformity include conditions such as rheumatoid arthritis, trauma, tendinitis, tenosynovitis, and other inflammatory conditions.
Treatment for pseudo-boutonniere deformity involves addressing the underlying cause and improving finger function. It may include splinting, range of motion exercises, strengthening exercises, modalities, joint mobilization, activity modification, taping, and patient education.
To prevent pseudo-boutonniere deformity, individuals should seek early diagnosis and treatment for underlying conditions, adhere to prescribed medications, perform hand exercises, protect the joints, avoid trauma, manage inflammation, maintain a healthy weight, use assistive devices if needed, and stay physically active.




2 Comments