Scaphoid Fracture
Overview
A scaphoid fracture is a common injury that occurs in the wrist, specifically involving the scaphoid bone, which is one of the small bones located near the base of the thumb. The scaphoid plays a crucial role in wrist movement and stability. Fractures of the scaphoid typically result from a fall onto an outstretched hand, causing direct impact to the wrist.
The most common type of carpal fractures are scaphoid fractures, which typically affect younger, more active people. They are responsible for 60% to 70% of carpal bone fractures and 2% to 7% of all fractures. It happens frequently that scaphoid fractures are initially overlooked during clinical and radiographic examinations. These injuries may initially be misdiagnosed as a straightforward wrist sprain.
Delays in diagnosing scaphoid fractures can result in a range of unfavorable consequences, such as radiocarpal joint osteoarthritis, nonunion (no fusion), delayed union, and reduced grip strength and range of motion. Adequate immobilization, prompt diagnosis, and referral for surgical opinion when necessary can all help reduce the risk of unfavorable results.
Although scaphoid fractures are common, they pose special challenges due to their unique geometry and the scaphoid’s delicate vascular pattern. Non-unions and consequent degenerative wrist arthritis can result from delayed diagnosis and insufficient therapy for acute scaphoid fractures.
Due to the high risk of non-union (14–50% if displaced), this misdiagnosis may result in increased morbidity for the patient. Within five years, arthritis, deformity, and instability always appear if untreated, and they can cause severe disability. Because these injuries frequently occur in young, active patients, there are major secondary disability-related morbidity and cost implications.
A scaphoid fracture may be treated surgically or with casting. The location and severity of the fracture in the bone can affect the best course of care. Scaphoid fractures are more likely to cause problems with the healing process than fractures in other bones because they involve areas of the bone that have a poor blood supply, and because a fracture can further disrupt, slow, or stop the flow of blood to the bone.
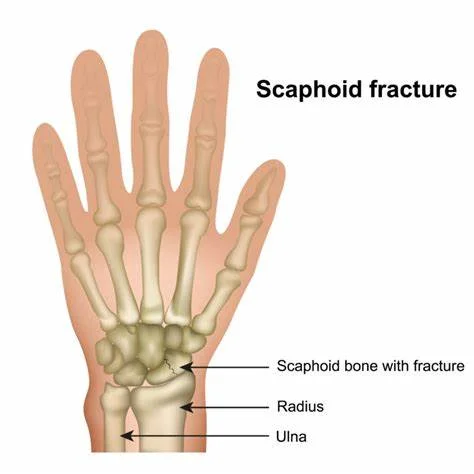
Relevant Anatomy
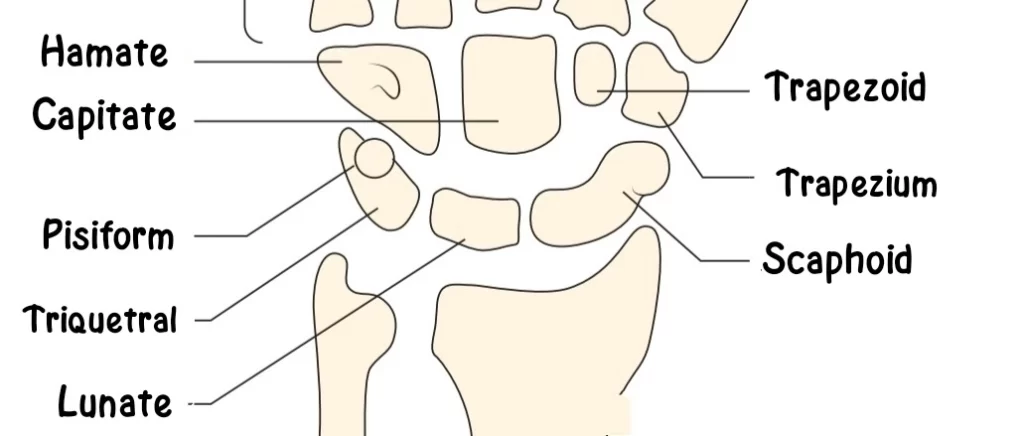
The eight carpal bones and the two forearm bones, the radius and ulna, combine to form the wrist. At the base of the hand, the carpal bones are positioned in two rows. Every row contains four bones.
Another of the bones located on the thumb side of the wrist, located slightly above the radius, is the scaphoid bone. The wrist joint’s stability and range of motion are both dependent on the bone.
There are 27 bones in the hand, with eight being carpal bones. At the base of the hand, there are two rows of carpal bones, each with four bones. One of the 8 carpal bones at the wrist is the scaphoid bone. One of the arm bones, the radius, is situated above it on the inside of the wrist.
The most comfortable way to recognize the scaphoid bone is to hold your thumb in the “thumbs-up” or “hitch-hiking” position. It is situated at the base of the wrist’s rear hollow created by the thumb tendons. This region, which is also sometimes referred to by the name “anatomic snuffbox,” is usually the site of greatest tenderness or pain following a scaphoid fracture.
Blood flows from the heart to the limbs, or arms and legs, and from the proximal (close to the body) to the distal (fingers and toes) regions of the body. Most of the bones in the arms and legs flow in this direction, with blood moving from the bone’s closest point to the body to its furthest point from the fingers or toes.
The Greek word for “boat” is the source of the word “scaphoid.” The scaphoid bone is somewhat long and curved, giving it a boat-like appearance. Because it connects the proximal row of carpal bones—the bones closer to the radius and ulna—to the distal row of carpal bones—the bones closer to the fingers—the scaphoid is particularly significant to wrist function. For the wrist to move as optimally as possible, the scaphoid must be able to move smoothly and freely.
A scaphoid fracture is a break in the hand’s scaphoid bone. Making up 60% of carpal breaks, it is one of the most frequent fractures of the carpal bones. Additionally, 11 percent of hand fractures are caused by it.
In addition to facilitating wrist movement, the scaphoid bone influences the wrist joint’s stability. The full range of motion in the wrist is impacted when a bone fractures.
The scaphoid’s blood supply, however, flows “backward”: blood enters the distal (or closest to the thumb) portion of the scaphoid and then returns to the proximal (or closest to the body) portion. Because of this, fractures involving the distal scaphoid heal far faster than those involving the proximal scaphoid. Indeed, there’s a chance that proximal scaphoid fractures will seriously impair blood flow, leading to necrosis, or partial scaphoid death. This condition, known as “avascular necrosis,” may result in chronic wrist issues.
The scaphoid has a waist situated between its proximal and distal poles, as seen in its anatomy. Dorsal carpal branches of the radial artery provide the majority of the supply of blood to the scaphoid bone. Because the blood supply is retrograde, fractures at the scaphoid waist put the proximal pole at a higher risk of developing avascular necrosis.
Parts Of Scaphoid Bone
Three parts make up the scaphoid:
- The end nearest to your thumb is called the proximal pole.
- Waist: the bone’s curved middle, located beneath the anatomic snuffbox
- Your forearm is the end nearest to your distal pole.
Because of its size and location on the outside of your wrist, the scaphoid is prone to fractures and injuries. Approximately 70% of carpal fractures occur in this bone, making it the most commonly fractured carpal bone.
Scaphoid fractures occur at the waist in about 80% of cases, the proximal pole in 20%, and the distal pole in 10%.
The fracture’s healing depends on where it is. Because the distal pole and waist have good blood supplies, fractures there typically heal quickly.
A fracture can easily cut off the poor blood supply that supplies the majority of the proximal pole. The bone dies without blood flow, a condition known as avascular necrosis. Proximal pole fractures don’t heal also or as rapidly.
Pathophysiology
The largest of the eight carpal bones is the scaphoid. The scaphoid’s waist is located between its proximal and distal poles, as shown in the anatomy. The majority of the scaphoid bone’s blood supply comes from the radial artery’s dorsal carpal branches. They enter the dorsal ridge and send retrograde flow to 80% of the proximal pole. The superficial palmar arch is derived from the radial artery, which enters and supplies the distal tubercle and distal pole. Because the blood supply is retrograde, scaphoid waist fractures increase the risk of avascular necrosis in the proximal pole.
Approximately 65% of fractures happen at the waist, 25% at the proximal third, and 10 percent at the distal third.
The proximal segment of the scaphoid has a 100% rate of avascular necrosis (AVN), which decreases to 33% at the distal segment. This indicates a strong correlation between the incidence of AVN and the location of the fracture.
Epidemiology
- Scaphoid fractures are most common among young adults, with an average age of 29.
- Greater frequency in men.
- This is unusual in the elderly and pediatric populations, where the distal radius or physis are more likely to fracture first.
- Scaphoid fractures cause 15% of all acute wrist injuries.
- Scaphoid fractures are associated with a high rate of nonunion (8-10%), malunion (common), and the long-term consequences of carpal instability, as well as post-traumatic arthritis.
- Fractures on this side of the scaphoid are more likely to cause aseptic necrosis and nonunion due to no blood vessels entering the nearest pole of the scaphoid.
- Ligamentous tears in the wrist are often associated with displaced fractures.
Mechanism
Scaphoid fractures can result from direct axial compression or hyperextension of the wrist, as can happen from falling on an outstretched hand and hitting the palm. There are three primary kinds of scaphoid fractures according to the Herbert classification system. Fractures occur at the proximal pole in 10%–20% of cases, the middle waist in 60%–80% of cases, and the distal pole in the remaining cases.
Causes of Scaphoid Fracture
The FOOSH represents “fall onto an outstretched hand.” It is the process that causes a lot of fractures to the upper limbs.
You cock your wrist and extend your arm in an attempt to break the fall with your hand as soon as you sense that you are about to fall.
Your wrist and arm absorb the full force of the impact, but your face, head, and back are shielded from harm. A fracture could result if it makes your wrist bend backward more than it should.
The location of a fracture depends on the angle at which your wrist hits the ground. Your scaphoid bone is more likely to break the farther your wrist is bent back. A distal radius fracture (also known as a Colles or Smith fracture) occurs when your wrist is not as extended, causing the radius bone to absorb the force of impact.
Scaphoid injuries are common because it is the primary joint that connects your hand to your forearm. The scaphoid muscle transfers all of the energy generated when your hand strikes the ground to your forearm when you fall on it. This tiny bone is subjected to extreme stress from the force, which increases the risk of fracture.
Many sports, particularly those involving skiing, skating, and snowboarding, can result in FOOSH injuries. One simple way to avoid these injuries is to wear a wrist guard.
Scaphoid fractures can also result from engaging in sports like shot put or gymnastics that put repeated strain on the scaphoid bone. Automobile accidents and a forceful blow to the palm are two more causes.
Clinical Features
Usually, patients who have fallen onto an outstretched hand complain of wrist pain.
- Because the scaphoid affects the dorsal rim of the radius, axial loading of the wrist, resulting in forced excessive extension and radial deviation, can cause a fracture.
- Other common causes include traumatic injuries from contact sports and car accidents.
There will be an immense impact of the hand on the arm that passes via the scaphoid bone after the traumatic event.
Sign and Symptoms
Swelling and pain near or around the anatomic snuffbox as well as on the thumb side of the wrist are common symptoms of scaphoid fractures. When you try to pinch, grasp, push, or pull something, or move your thumb or wrist, the pain could get very bad.
It may not be immediately apparent to you that you have a broken scaphoid bone unless your wrist is malformed. Some scaphoid fractures cause mild pain that could be misdiagnosed as a wrist sprain.
It is essential to see a doctor if your wrist pain does not go away within a day of the injury as this could indicate a fracture. Treating a scaphoid fracture as soon as possible may help prevent complications.
Types of Scaphoid Fracture
There are certain displayed by the fractured scaphoid that prevent healing. Because they are naturally unstable and prone to displacement, fracture fragments must come into motionless contact to unite. As previously stated, the scaphoid’s blood supply is insecure.
The scaphoid has been divided into three anatomic sections for therapeutic decision-making: proximal, medial, and distal.
There are two more categories for fractures: displaced and non-displaced.
Non-displaced Fractures
Strict immobilization in a well-formed short-arm thumb spica promotes effective healing of non-displaced distal fractures. The use of a long or short arm cast is debatable. A thumb spica is the current therapy for this kind of fracture, however, there is some evidence to support the idea that the thumb could be left out of the cast.
Screw fixation may help the patient return to pre-injury activities faster; depending on the patient’s needs, a surgical referral may be required.
Orthopedic consultation is recommended for these patients because the fracture line moves proximally, increasing the risk of displacement and nonunion. If a conservative approach is chosen, thumb immobilization with a long arm cast is recommended.
Displaced Fractures
Surgery is recommended for fractures with minor displacement because they are prone to nonunion.
The fixation will involve the use of double-threaded headless screws. The fracture morphology dictates which surgical technique is best. Referral and splinting are recommended.
Casting with a short or long arm is the standard treatment for undisplaced and stable scaphoid fractures.
Diagnosis
Physical Examination
In the anatomic snuffbox, scaphoid fractures most frequently result in pain and swelling on the base of the thumb.
Patients who have experienced recent trauma typically present with wrist pain. Patients frequently appear late because the injury does not show up on simple radiographs. Pain frequently occurs on the radial side of the wrist and worsens with movement. The wrist’s range of motion may be reduced, as well as swelling. Finding out if the patient smokes is critical because it increases the risk of non-union by about 20%.
When examining the wrist, use the “look, feel, and move” method. Unless there is a concurrent carpus dislocation, such as a lunate dislocation, the deformity is unlikely. To rule out any related injuries, palpate the distal radius, ulna, and metacarpals. Anatomic snuffbox. Dorsally is traditionally tender, especially after a wrist fracture. The snuffbox is located between the first and third extensor compartments, with the extensor pollicis longus tendon on the ulnar side and the abductor pollicis longus and extensor pollicis brevis tendons lying radially. Tenderness over the volar aspect scaphoid tubercle, which is felt as a bony prominence radial to the flexor carpi radialis at the level of the distal palmar crease, may also occur.
One of three places is typically where tenderness presents itself:
- When a distal pole fracture occurs, the volar prominence located at the distal wrist
- Anatomical snuffbox for waist or mid-body fractures.
- Distal to the proximal pole fractures for Lister’s tubercle.
The scaphoid compression test, which is more sensitive, entails compressing each scaphoid pole with the examining thumb and index finger. If a fracture is present, this maneuver is likely to cause pain. A scaphoid fracture is also suggested by pain in the anatomic snuffbox during the ulnar deviation of the wrist.
X-ray
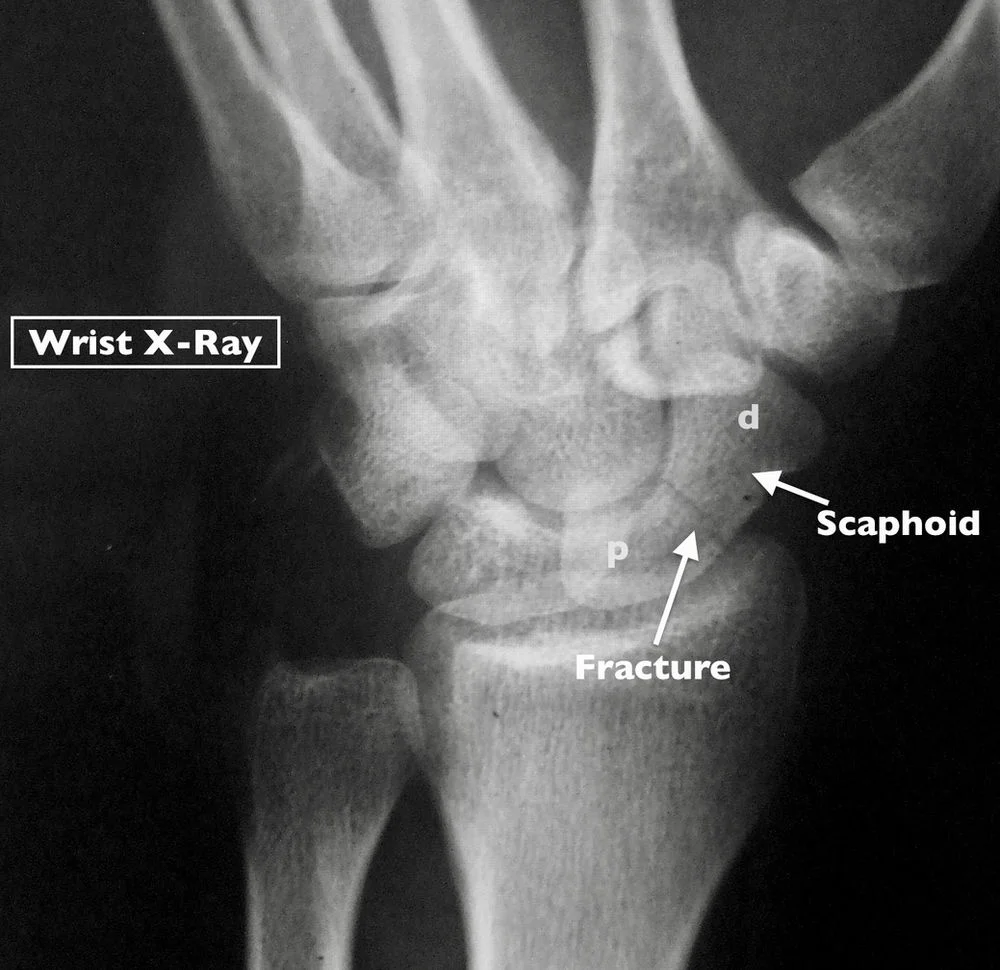
X-rays can be used to obtain images of dense structures such as bones. Your doctor will most likely order an X-ray to determine whether you have a scaphoid fracture and if the fractured bone fragments are displaced. An X-ray will allow your doctor to see if there are any additional fractures or dislocations.
Scaphoid fractures are not always visible on an X-ray right away. Your doctor may advise you to wear a wrist splint or cast for two to three weeks before returning for a follow-up X-ray if they suspect you have a fracture but it is not visible on the scan. Scaphoid fractures often take some time to appear on an X-ray. Wear your cast or splint and avoid doing anything that could worsen your injury while you wait.
The assessment begins with the scaphoid and PA views of the wrist, which are obtained with the wrist at approximately 20 degrees ulnar deviation and 30 degrees extension. Up to 25% of scaphoid fractures are thought to be invisible on first plain radiographs. If there is a high level of clinical suspicion, repeat plain radiographs and immobilize the wrist in a cast or splint for seven to fourteen days. Bone scans can be performed 72 hours after the injury to detect occult fractures if immediate confirmation is required.
Magnetic resonance imaging (MRI) scan
If clinical suspicion persists despite negative repeat radiographs, Magnetic Resonance Imaging (MRI) is recommended. Magnetic resonance imaging (MRI) is the most accurate diagnostic method, as it can detect any associated ligamentous damage or bone edema/contusions. According to a recent meta-analysis, MRI is 99.8% specific and 97.7% sensitive.
CT scan (computerized tomography)
A CT scan can be useful in identifying a scaphoid fracture and in determining whether there is bone displacement. The results of the CT scan may be used by your doctor to guide the creation of your treatment strategy.
USG (Ultrasonography)
To get a good image of the scaphoid bone and identify a fracture, USG is an additional option. In a 2018 study with 114 participants, it was discovered that USG could identify scaphoid fractures with over 98% accuracy.
Differential Diagnosis
The location of tenderness, pain during specific movements, and radiographic abnormalities can be used to distinguish between these diagnoses.
- Fracture of the distal radius
- Additional Fractures of the carpal bones
- Dissociation of the scapholunate
- Osteoarthritis
- De Quervain Tenosynovitis
Treatment of Scaphoid Fracture
Your doctor’s recommended course of action will be contingent upon several factors, including but not limited to:
- The location of the bone fracture
- If the pieces of bone are misplaced
- How long ago did your injury occur?
- Your overall health and age
Medical Management
In 7–14 days, follow-up films should be taken for suspected fractures with positive clinical signs on examination but negative radiographs. More imaging, such as an MRI or CT scan, should be done if the pain continues and the radiographs are still normal. It is advisable to think about using pharmacists to help with pain management.
Conservative Management
Non-operative management of non-displaced fractures occurring within the distal third of the bone involves immobilization in a cast. There is disagreement over the best length for an arm cast and whether or not to use a thumb spica to immobilize the thumb, but there isn’t any data to support either position at this time.
Recurring radiographs are typically taken during the six-week immobilization period to evaluate the union.
The position of the fracture affects the time it takes for union.
- For approximately ninety percent of non-displaced or little displaced (≤ 0.5 millimeters) scaphoid waist fractures, the distal third should heal in 6–8 weeks.
- Inside the middle third in 8–12 weeks
- First third in a matter of weeks.
- Conservative treatment is possible for scaphoid waist fractures with little displacement (0.5–1.5 mm), but extended cast immobilization for between eight and ten weeks is necessary.
The shaky blood supply as well as retrograde arterial flow are secondary reasons for the relative increase in healing time when moving from the distal to the proximal region.
In general, if there is a clinical suspicion of a scaphoid fracture but no visible fracture on the initial radiographs, a short arm thumb spica should be applied, and the patient reevaluated in two weeks. If a cast is not applied, the fracture may worsen over time. The patient should be pain-free at the two-week visit, and an additional radiograph should be obtained.
Nonsurgical Treatment
Fracture near the thumb:
Closer to the thumb (distal pole) non-displaced scaphoid fractures are more likely to heal with appropriate care and limited activity. There is adequate blood flow to this area of the scaphoid bone, which is important for healing.
Your doctor might put your hand and forearm in a splint or cast if you have this kind of fracture. Typically, the cast or splint will cover your thumb and be placed below the elbow.
Each patient’s healing process is unique. Using X-rays or other imaging studies, your doctor will keep an eye on your healing process.
Fracture near the forearm:
Healing may be more difficult if the scaphoid is broken (but not displaced) in the proximal pole (closer to the forearm) or in the middle of the bone (the waist). As previously stated, there is insufficient blood supply to these parts of the scaphoid.
If your doctor decides to treat this type of fracture with a cast, the cast may cover your thumb and the area above the elbow. In comparison to a more distal fracture near the thumb, you will typically need to wear the cast or splint for a longer period.
Bone stimulator:
Your physician might occasionally advise using a bone stimulator to speed up the healing of fractures. This tiny gadget emits electromagnetic pulses or low-intensity ultrasonic waves to promote healing.
Surgical Treatment
If your scaphoid fracture is at the waist, proximal pole, or dislocated, your doctor may recommend surgery. Surgery aims to improve the prognosis of the fracture by reorienting and stabilizing it.
Reduction
The doctor will push the bone back into position during the procedure. This is sometimes accomplished with a smaller incision and specialized guided instruments. In other cases, an open incision is made and the fracture is manually adjusted. Your doctor may use an arthroscope, a small camera, to help reduce certain fractures.
Internal fixation
Metal implants, such as screws, plates, and/or wires, are used in this section of the procedure to hold the scaphoid in place while the bone heals and to save the fractured ends together.
Depending on which portion of the scaphoid is broken, the surgical incision’s location and size will vary. Occasionally, a tiny incision may be made to insert the implants into bone fragments. In other cases, a larger incision is required before fixing the scaphoid fragments to ensure proper alignment. You can choose to make the incision on the back or palm side of your wrist.
Bone Graft
An internal fixation may or may not be utilized in conjunction with a bone graft. The replacement of the broken bone with a new bone is known as a bone graft. It can promote the growth and repair of bones. You may donate bone from your hip, elbow, forearm, or another location. Additionally, some manufacturers provide grafts that can be used in the fracture to avoid the need for the surgeon to remove bone from your body.
Physiotherapy Management
When the fracture is deemed stable and the cast is taken off following the period of immobilization, both post-operatively or conservatively, the hand and wrist are probably going to be stiff and have less muscle strength.
Physiotherapy’s main objectives are:
- Restore active range of motion (AROM).
- Reduce edema
- Boost wrist and grip power
- Go back to the functional tasks and goals.
ROM Exercises
Since the wrist and hand will be stiff, the first stages of ROM exercises following immobilization should concentrate on active-assisted ROM.
The wrist and thumb should be the main focus of these exercises, but the fingers, elbow, and shoulder should also be taken into account as these areas may also become stiff after immobilization.
If the complete range of motion is still limited, manual therapy exercises involving joint mobilizations to the radiocarpal, radioulnar, and possibly even the carpal joints may prove beneficial during the therapy session.
To lessen any lingering pain or swelling, additional manual therapy techniques like massage or soft tissue work may also be beneficial.
Strengthening Exercises
It is crucial to perform wrist and hand strengthening exercises after complete or functional AROM has been restored.
This is a crucial phase in the healing process because, without hand strengthening, the patient may have long-term functional deficits and run the risk of suffering new injuries.
Functional Restoration
Once AROM has been restored and a strong baseline developed, the focus should shift to customized objectives and tasks.
Scaphoid fractures often affect young to middle-aged individuals who are active, have jobs, or care for families. To accomplish these goals, customized rehabilitation and exercise regimens are required. If the fracture was treated properly in the early stages—that is, without missed avascular necrosis—full function will eventually be restored.
It has been demonstrated that early surgical intervention in the sporting group resulted in a quicker return to play, averaging 6-11 weeks, as opposed to 4-16 weeks for conservative management.
Recovery
You might need to wear a cast or splint for up to six months, or until your fracture heals, depending on whether you require surgery or nonsurgical treatment. Scaphoid fractures heal more slowly than most other types of fractures. You should refrain from the following activities during this time unless your doctor gives the all-clear for advanced activity:
- Pushing, pulling, lifting, or carrying something weighing more than one pound
- Throwing while your arm is painful
- Participating in sports that involve contact
- Climbing trees and ladders
- Activities like trampoline jumping or inline skating may pose a risk of falling onto your hands.
- Smoking while operating heavy machinery or vibrating equipment
After scaphoid fractures, some patients experience wrist stiffness. Patients who need more extensive surgery or wear a cast for an extended period are more likely to experience this.
You must keep your fingers moving normally during your recuperation. In addition to prescribing an exercise regimen, your doctor might also recommend a skilled hand therapist to help you restore as much wrist strength and range of motion as possible.
Some patients may not regain their pre-injury range of motion and strength, even with hand therapy and significant patient effort during home therapy.
Prognosis
It has been demonstrated that 86% of the time, conservatively treated non-operative fractures result in good to excellent functional outcomes. Studies show that although less than 1% of fractures require surgery, patients who do so have very good functional outcomes.
Active as well as active-assisted range of motion exercises usually take six weeks during rehabilitation; strength training starts three to four months after surgery or injury. For non-operative fractures, patients can frequently anticipate almost no functional deficits and good to excellent outcomes in the case of fractures requiring surgical treatment.
Complication
Never neglect signs of discomfort, edema, or soreness. You still need treatment even if your symptoms aren’t very bad. Untreated scaphoid fractures can lead to more severe consequences down the road, such as:
- Acute compartment syndrome (ACS): A build-up of pressure within your muscles can prevent blood flow to affected areas, leading to irreversible damage to your muscles and nerves.
- Malunion: This is the misalignment of your broken bones during the healing process.
- Nonunion: Your bones might not fuse back together again, either entirely or partially.
- Avascular necrosis (osteonecrosis): This is a painful bone ailment that deteriorates with time and may limit your range of motion. It happens when the blood supply to one of your bones is interrupted.
- Hand and wrist arthritis: Avascular necrosis and nonunion can cause this condition. Hand arthritis results in pain, edema, stiffness, and deformity.
Prevention
There’s not much you can do to prevent scaphoid fractures other than taking safety precautions when walking (use a cane or walker if you’re using one) and being cautious on uneven surfaces because these fractures are typically caused by falls or other accidents.
To reduce your chance of getting an injury, follow :
- Set on your seatbelt whenever possible.
- When performing part in any sport or activity, wear the proper protective gear.
- Make sure nothing in your house or place of business could harm you or anyone else.
- At home, always use the proper tools or equipment when reaching for objects.
- Avoid standing on chairs, tables, or countertops.
- Adhere to a diet and exercise regimen that will support the health of your bones.
- Always use a cane or walker to assist with walking, and exercise caution when using it on uneven surfaces.
FAQs
Is a scaphoid fracture serious?
In reality, there’s a chance that proximal scaphoid fractures will seriously impair blood flow, leading to necrosis, or partial scaphoid death. This condition, known as “avascular necrosis,” may result in chronic wrist issues.
What are the 3 tests for scaphoid fracture?
When assessing patients who may have a scaphoid fracture, the three most popular clinical tests are anatomical snuff box tenderness, scaphoid tubercle tenderness, and pain on axial compression of the thumb.
What is the best treatment for a scaphoid fracture?
Cast therapy is typically effective for scaphoid fractures where there is no bone displacement at the site of the fracture. For some patients, the healing process for a fracture may take longer than six weeks.
What age is scaphoid fracture common?
With a mean age of 29, scaphoid fractures primarily affect young adults. greater frequency in men. Unusual in the elderly and pediatric populations, where the distal radius or physis, respectively, are more likely to break first.
What is the quickest method for scaphoid bone healing?
A short arm thumb spica cast immobilizes the wrist and thumb until the fracture heals. For the first six weeks of treatment, some surgeons might place this in a cast above the elbow, then switch to a shorter cast. However, a bone stimulator may be used if, even after six weeks of casting, the fracture is not healing properly.
Can a scaphoid fracture heal without surgery?
Your arm will be treated by having a cast applied from your wrist to your elbow if the fracture hasn’t moved. To allow the scaphoid bone to heal properly, it must stay in this position for eight to twelve weeks.
REFERENCES
- Scaphoid Fracture of the Wrist – OrthoInfo – AAOS. (n.d.). https://orthoinfo.aaos.org/en/diseases–conditions/scaphoid-fracture-of-the-wrist
- Scaphoid Fracture: What You Need to Know About a Broken Wrist. (2023, June 27). Healthline. https://www.healthline.com/health/bone-health/scaphoid-fracture#causes
- Scaphoid Fracture. (n.d.). Physiopedia. https://www.physio-pedia.com/Scaphoid_Fracture
- Professional, C. C. M. (n.d.). Scaphoid Fracture. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/22240-scaphoid-fracture
- Scaphoid Fracture: Symptoms & Treatment | The Hand Society. (n.d.). https://www.assh.org/handcare/condition/scaphoid-fracture
- Hayat, Z. (2023, August 4). Scaphoid Wrist Fracture. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK536907/
- Steffes, M. J. (n.d.). Scaphoid Fracture – Hand – Orthobullets. https://www.orthobullets.com/hand/6034/scaphoid-fracture
- De Pietro Crt, M. (2022, November 30). What to know about scaphoid fractures. https://www.medicalnewstoday.com/articles/scaphoid-fracture#Diagnosis