Joint Mobilization
What is Joint Mobilization?
Joint mobilization is a manual therapy treatment technique mostly applied by physical therapists to improve joint mobility and relieve joint pain. It involves the passive movement of a joint by an external force to restore or enhance its range of motion, flexibility, and function.
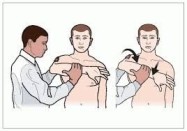
During joint mobilization, the therapist applies controlled and graded forces to the joint surfaces, using their hands or specialized instruments. The goal is to create specific mechanical effects on the joint tissues, including the ligaments, joint capsule, and surrounding structures. These techniques can include oscillatory movements, sustained stretching, gliding motions, and rhythmic oscillations.
Joint mobilization techniques are typically performed within the available range of motion of the joint, and the therapist carefully evaluates the patient’s response and adjusts the technique accordingly. The therapist may use their hands to apply force directly to the joint or may use belts, straps, or other tools to aid in the application of force.
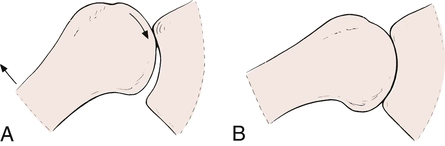
Joint mobilization is working on the convex-concave rule. When a convex surface is glide forward on a concave surface, the direction way of joint glide is opposing to the direction way of osteokinematic movement, whereas when a concave surface is glide on a convex the direction way of joint glide is in a similar direction way of osteokinematic movement.
To better understand joint mobilization need to understand the following few words:
Range of Motion (ROM)
The word range of motion (ROM) means precisely that; it is the degree of movement at a joint. In different terms, how distant one bone at a joint can move comparable to the other bone at that joint.
Relying on the joint, there may be differing ROM probable. Such as a triaxial joint e.g., the shoulder (glenohumeral) joint, would have more ROM than the elbow joint, which is a uniaxial joint.
ROM is generally called for sagittal, frontal, and transverse plane segment movements. So the elbow joint can move in flexion & extension in the sagittal plane; whereas the shoulder joint can move in flexion & extension in the sagittal plane, abduction & adduction in the frontal plane, and external rotation and internal rotation in the transverse plane.
Surely, we could even define diagonal plane ROM as well.
Active Range of Motion (AROM)
- Active Range of Motion (AROM) is described as the ROM that a joint can move when pushed by the squeeze of the musculature of that joint.
Passive Range of Motion (PROM)
- Passive Range of Motion (PROM) is described as the ROM that a joint can move when pushed by a power other than the musculature of that joint.
- A physiotherapist could supply this other power.
- But this other power could even be supplied by the individual itself; such as one could utilize their right hand to push the neck into a ROM.
- PROM is normally a little more than AROM.
Joint Play
Joint Play is described as the little part of nonaxial glide that is achievable at a joint at the end of PROM.
A further joint play is a dislocation of a joint.
Movement in joint play is generally nonaxial.
Axial Motion
- An axial motion is a movement in which one bone moves near an axis.
- An axis is an imaginary line, normally passing via the middle of the joint, near which movement happens.
- Due to the movement existing near the axis, the movement is circular.
- Axial movements are also understood as circular/angular movements.
- Most joint movements that physiotherapists think of are axial; e.g. flexion, and adduction. With an axial movement, various points along the bone that is moving would shift in various portions.
- Points nearer to the axis (i.e., the joint) transcribes a shorter rotation than points that are distant from the axis.
Nonaxial Motion
- A nonaxial motion is a movement in which the bone doesn’t move near an axis.
- Thus every point on the bone that is moving would move a similar amount.
- Nonaxial motions are also understood as gliding, sliding, and planar movements.
Fundamental Components of Motion
Although most physiotherapists understand words of movement e.g. flexion and abduction, there are fundamental movements that sustain these additional familiarly called movements.
The three fundamental kinds of movement that sustain all movements are spin, roll, and glide.
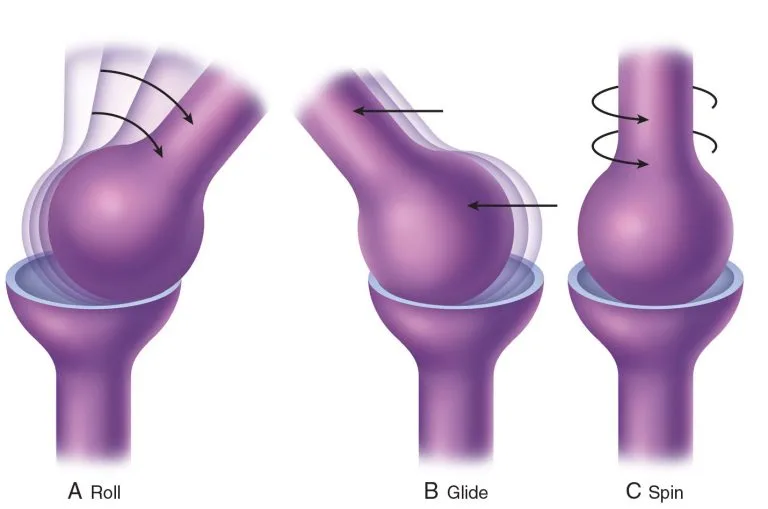
Spin
- Spin is a rotation, generally an extended-axis rotation, in which one bone spins on the other bone near the extended axis of the joint.
Roll and Glide
- Roll and glide are generally believed concurrently because when roll happens, it needs to be accompanied by glide for a beneficial joint movement to happen.
- Roll is an axial movement; glide is a nonaxial movement.
- Basically, when the articular surface of one bone rolls on the articular surface of the other bone, it would roll off the other bone (in different terms, dislocate) if there weren’t some restorative glide.
- Also if one bone were to not roll all the path off the other bone, if it did a pure roll movement, it would no longer be centered on the articular shell of the other bone.
- The word centration defines the maximum positioning of one bone being centered on the other. This is the maximum because the articular cartilage is generally widest in the middle of the articular surfaces. Articular cartilage is essential to soften the compression pressure of the two bones against each other.
- There are two kinds of compensatory glide that escort a roll movement.
- When a convex bone moves on a concave bone, the glide is in the opposing direction way of the roll. Such as would be the head of the humerus moving on the glenoid fossa of the scapula.
- When a concave surface bone moves on a convex surface bone, the glide is in a similar direction way as the roll. Such as would be the base of the proximal phalanx (concave) moving on the head of the metacarpal at a metacarpophalangeal joint (convex).
- Apprehending how the nonaxial glide connects to the axial roll at a joint suggests how the joint mobilization should be used. Such as, at the metacarpophalangeal joint, if there is a downfall of axial elongation of the finger, then due to finger extension including a dorsal roll with a dorsal glide, the nonaxial glide mobilization that would be required would be a dorsal glide.
What are the Principles of Joint Mobilization?
Fit joint movements without restriction. Synovial joints the movement facilitates biological movement by pushing synovial fluid to regions of avascular articular cartilage. Also, the power and resiliency of capsular tissue & periarticular tissue are held through joint activity. Immobilization leads to damaging effects for example articular adhesions, fatty infiltration, and physiologic adaptations to the power and toleration of soft tissue (ligaments, tendons, and capsular tissue). The word mobilization guides to try to correct joint movement and flexibility, and reduce aches related to joint structures utilizing manual, passive accessory-joint motion.
Joint mobilizations are passive manual therapy approaches used to joints and associated with soft tissues at differing velocities and amplitudes utilizing physiologic and additional movements for restoring goals. Range of motion (ROM) includes physiologic motions which are active or passive movements at a disseminated joint via one of the standard cardinal planes of flexion, extension, abduction, adduction, or medial and lateral rotation. Physiologic activities are occasionally named osteokinematic, classical/standard activities because they are motions of the fundamental bones of a disseminated joint system. These movements can be visualized by the bare eye and are generally estimated by a goniometer.
Osteokinematic movements happen in the cardinal planes of action like frontal, sagittal, and transverse. Hip, knee, and shoulder flexion activities are examples of osteokinematic motions. These are all activities that can happen under volunteer command. Arthrokinematic activities are those that happen at the bone ends, without reference to the motion. These activities aren’t under volunteer command. These kinds of activities are understood as accessory activities including movements precise to enunciating joint surfaces. These accessory joint actions are guided to glide/slide, spin, and roll.
Accessory and physiologic joint movements happen together while active ROM. If the full accessory movement doesn’t happen, there will be a boundary in regular physiological cardinal plane actions. Yet, accessory joint action can’t be selectively drafted, indicating that a patient can’t selectively conduct joint roll, glide, and spin independently on their own. The use of additional joint activity is represented as joint play/motion that happens within the joint as a reaction to an outer strength but not as a result of the volunteer action.
An arthrokinematic glide & an arthrokinematic slide motion are basically the same. Gliding and sliding happen as a precise point on one part of the articular surface reaches into connection with a sequel of areas on the related joint surface. An analogy of this would be a car wheel gliding on ice when brakes are caused. One element of the tire glides/slides across a series of areas on the ice surface. When the elbow is bent doing a biceps curl, the convex olecranon moves anteriorly and glides/slides posteriorly on the somewhat fixed concave trochlea of the distal humerus.
The arthrokinematic motion spin happens when a part of one joint rotates, clockwise/counterclockwise, near a fixed longitudinal axis. An example of this is when a forearm moves in supination & pronation. At the radiohumeral joint, the radial head will rotate on the capitellum of the humerus.
Rolling happens when considerable points of contact on one joint shell get into contact with multiple points of connection on the affiliated joint surface. The analogy for this action would be a car tire driving generally where the tire surface creates a connection with a separate part of the roadway. In persons, this happens as the convex surface of the distal femur spins forward and glides on the concave surface of the tibia when the person shifts from a seated to a standing position.
Joint Congruency and Position
The joint congruency and the words close-packed and loose-pack direct to joint position, which is relevant to the discussion of different grades of mobilization. Congruence guides to an articular position about concave and convex joint shells. A joint is harmonious when both bone-articulating surfaces are in touch throughout the total surface area of the joint. Regardless, the investigation of arthrokinematics joint movement remarks that joints are infrequently in complete unity. As joints activity, the extra actions of glide/slide, spin, and roll change the entire joint congruence.
MacConaill and Basmajian have defined close-packed positions as the congruent positions of a joint, where the joint articular textures are aligned and the capsule and ligaments are tight and the joint volume is tiniest. Normally, a closed-packed position is utilized for testing the probity and stability of ligaments and capsular systems. Regardless, the close-packed position defined by MacConaill and Basmajian isn’t utilized for mobilization approaches. The close-packed position is one of the stable positions. When the elbow and knee are fully extended the ligaments and joint capsule are tight which allows no independence of motion. Thus the knee and elbow in extension serve as two perfect samples of a close-packed position of joints.
Any joint position beside the close-packed position is a loose-packed position. The position in which the joint capsule and ligaments are most comfy and flexible, letting the highest amount of joint play is directed to the resting position of a joint. When the knee joint is bent to 30°, the intracapsular space is expanded, helping ligaments evolve more loosely. The loose-packed position is perfect for using joint mobilization approaches, but aching, inflexible, and dysfunctional joints are infrequently in perfect resting positions for the application of joint mobilization. The below table lists the loose-packed and close-packed positions of the prominent joints in the human. If a joint has a restriction of arthrokinematic action in which the close-packed position can’t be accomplished, ground reaction forces & gravitational forces aren’t maximally spread via the joint, therefore extra pressure and work have to be carried up by the periarticular muscles. If this dysfunctional motion pattern persists, a state of muscle overuse may happen.
| Joint | Resting Position | Closed-Packed Position |
|---|---|---|
| Facet (spine) Joint | Midway between flexion and extension | Extension |
| Temporomandibular Joint | Mouth slightly open (freeway space) | Clenched teeth |
| Glenohumeral Joint | 55° abduction, 30° horizontal adduction | Abduction and lateral rotation |
| Acromioclavicular Joint | Arm resting by side in normal physiologic position | Arm abducted to 90° |
| Sternoclavicular Joint | Arm resting by side in normal physiologic position | Maximum shoulder elevation |
| Ulnohumeral (elbow) Joint | 70° flexion, 10° supination | Extension |
| Radiohumeral Joint | Full extension, full supination | Elbow flexed 90°, forearm supinated 5° |
| Proximal radioulnar Joint | 70° flexion, 35° supination | 5° supination |
| Distal radioulnar Joint | 10° supination | 5° supination |
| Radiocarpal (wrist) Joint | Neutral with slight ulnar deviation | Extension with radial deviation |
| Carpometacarpal Joint | Midway between abduction-adduction and flexion-extension | Full flexion in the medial joints |
| Metacarpophalangeal Joint (all) | Slight flexion | Full extension, lateral rotation of the tibia |
| Metacarpophalangeal Joint (fingers) | Slight flexion | Full flexion |
| Metacarpophalangeal Joint (thumb) | Slight flexion | Full opposition |
| Interphalangeal Joint | Slight flexion | Full extension |
| Hip Joint | 30° flexion, 30° abduction, slight lateral rotation | Full extension, medial rotation |
| Knee Joint | 25° flexion | Full extension, lateral rotation of tibia |
| Talocrural (ankle) Joint | 10° plantarflexion, midway between maximum inversion and eversion | Maximum dorsiflexion |
| Subtalar Joint | Midway between extremes of range of motion | Supination |
| Midtarsal Joint | Midway between extremes of range of motion | Supination |
| Tarsometatarsal Joint | Midway between extremes of range of motion | Supination |
| Metatarsophalangeal Joint | Neutral | Full extension |
| Interphalangeal Joint | Slight flexion | Full extension |
The Convex-Concave Rule
Anatomically, all articular textures are either convex or concave even though the textures of some joints aren’t honestly of either shape. In these circumstances, fibrocartilage improves and alters the shape of the joint textures. On the convex surface of a joint, more cartilage is located in the middle of the texture, and on the concave surface of a joint, more cartilage is located at the edge.
The convex-concave rule precisely remarks When the concave texture is fixed and the convex texture is pushing, the gliding motion in the joint happens in a direction opposing to the bone action. Contrariwise, if the convex texture is fixed during the concave texture is moving, the gliding movement happens in a similar direction as the bone action. This happens due to the convex bone texture constantly holding an axis of spin while joint action. The concept of supplement joint movements (glide or slide, spin, and roll), as they use joint congruency and the convex-concave rule, is absolutely presented by MacConaill’s classification of accessory actions.
Grades of Joint Mobilization
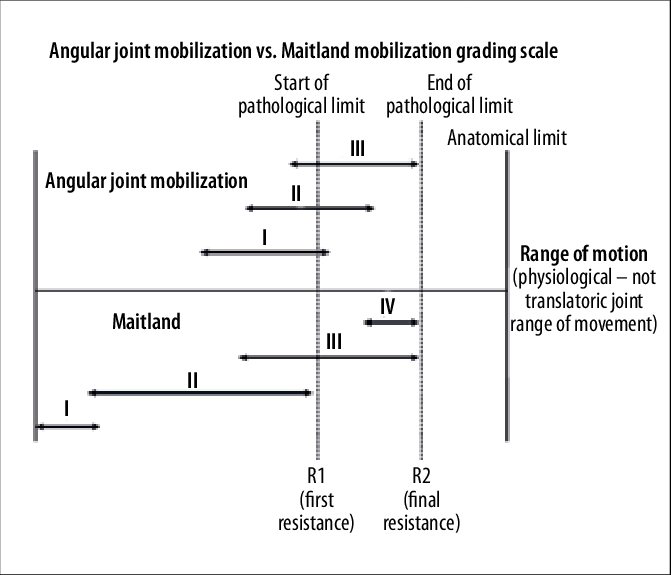
Maitland Joint Mobilisation Grading Scale:
Maitland has defined different grades of fluctuation for joint mobilization. The amplitude of separate oscillation grades drops within the range of motion (ROM) continuity between some starting points to the anatomical limit of the body tissue. Shows the different oscillation grades utilized in a joint with some restriction of movement. As the severity of the motion restriction gains, the point of restriction actions to the left away from the anatomical limit of body tissue. Regardless, the connections that exist among the 5 grades in words of their roles within the range of motion (ROM) stay the same. The 5 mobilization grades are described below:
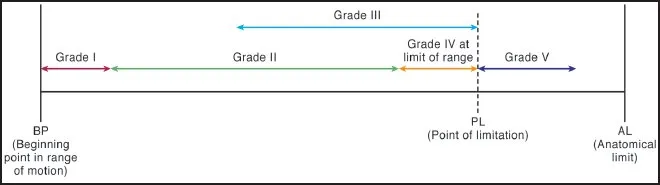
- Grade I: A small-amplitude action at the start of the range of motion (ROM). Utilized when aches and spasms restrict the action earlier in the range of motion (ROM).
- Grade II: A large-amplitude action up to the midrange of motion. Utilized when stiffness restricts action shortly with a brief oscillation than with a slow one, and when a gradually rising ache limits motion midway in the range.
- Grade III: A large-amplitude movement within the point of restriction in the range of motion (ROM). Utilized when aches and resistance from stiffness, static body tissue stress, and body tissue constriction restrict action around the end of the range of motion.
- Grade IV: A small-amplitude action at the exact end range of motion (ROM). Utilized when resistance restricts activity in the lack of aches and spasms.
- Grade V: A small amplitude, short thrust provided at the end range of motion (ROM), normally escorted by a popping sound in the treated joint, understood as a thrust manipulation of the joint. The popping sound is induced by cavitation, which happens because of reduced intra-articular tension in the joint capsule that generates bubbles in the synovial fluid to pop to balance tension. Utilized when the tiniest resistance restricts the end range of motion (ROM). Manipulation is most virtually conducted by the speed of the thrust instead of by the power of the thrust. Most sources approve that manipulation should be utilized only by people who are qualified particularly in these approaches because a significant value of skill and determination is essential for secure and adequate therapy.
The mobilization grading scale has been divided into two because of their clinical uses:
- Lower grades (I & II) are utilized to relieve aches and irritability (use Visual Analogue Scale (VAS) + Severity, Irritability Nature (SIN) scores).
- Higher grades (III & IV) are utilized to lengthen the joint capsule and passive tissues which reinforce and provide stability to the joint to raise the range of motion (ROM).
The rate of mobilization should be regarded as an oscillation in a rhythmical manner, containing:
- 2Hz – 120 movements/minute
- For 30 seconds – 1 minute
Kaltenborn Traction Grading Scale:
Kaltenborn has suggested a method utilizing traction mixed with mobilization as a mechanism of decreasing ache and mobilizing hypomobile joints. As concerned earlier, all joints have a specific amount of play/looseness. Kaltenborn guided to this looseness as slack. Some degree of slack is essential for regular joint movement. Kaltenborn’s 3 traction grades are described below:
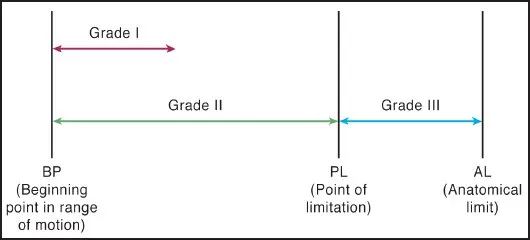
- Grade I traction (loosen): Traction that balances tension in the joint without exact partition of the joint surfaces. The goal is to create pain ease by decreasing the compressive pressures of articular surfaces while mobilization and is utilized with all mobilization grades.
- Grade II traction (tighten or take up the slack): Traction that actually divides the articulating surfaces and takes up the slack and stops play in the joint capsule. Grade II is utilized in the beginning cure to decide joint sensitivity.
- Grade III traction (stretch): Traction that implicates exact stretching of the soft tissue enclosing the joint to improve flexibility in a hypomobile joint.
Are Joint Mobilization and Joint Stretching similar?
Yes, joint mobilization is joint stretching. Although joint mobilization is called individually from joint stretching.
Grade III is effectively standard stretching that any therapist, trainer, or Pilates/yoga educator would conduct.
Grades IV and V joint mobilization are effectively tacked and stretch approaches.
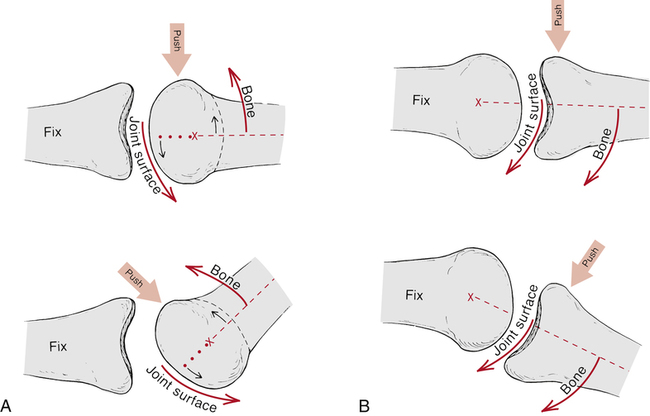
What is the Application of Joint Mobilization?
- Grades IV and V joint mobilization are effectively stapled and stretch methods.
- Bone A is stapled (stabilized) and then Bone B is shifted compared to Bone A.
- The relations for Grade IV and Grade V need to be as near on both bone (A and B) to the joint surface as doable to accomplish nonaxial glide mobilization if the connection is distant from the joint surface, a typical axial Grade III mobilization will happen rather.
- Hence, Grade IV and V joint mobilization is a state of stretching. It is a very precise format of stretching that is desired at lengthening the innate body tissue of the joint.
- Joint innate body tissue is formed of the fibrous joint capsule which includes the ligaments of the joint, and intrinsic muscles, if present (such as rotatores and intertransverse and interspinal of the spine).
- Grade IV joint mobilization is generally accomplished with a sequence of slow oscillations, each motion being very little amplitude, a bit of an inch/cm maintained for a bit of a second.
- The joint is conveyed to a body tissue tension barrier at the end range of the passive range of motion (PROM). Then mobilization force is applied to a joint.
- These Grade IV oscillations are normally repeated for a few sets of 3-5 repetitions, and possibly 10-15 seconds value of oscillations are executed. As with any state of manual therapy, precisely how the approach is conducted is based on the requirements and reactions of the patient on the table at that time.
- With Grade V joint mobilization, one fast thrust is normally conducted.
- Mobilizations are replicated for any directions of motion that are indicated.
When should Joint Mobilization be performed in Manual Therapy?
- Given that joint mobilization is a kind of joint stretching, as with all stretching, it will likely be most useful if conducted after soft tissue manipulation and warmth are foremost accomplished to the region so that the soft body tissues of the treated area will be lax and heated up, sufficiently tolerating the joint mobilization force.
- Joint mobilization targets stretching the innate body tissue of the joint, but the outside (extra-articular/periarticular) soft tissues need to be loose adequately to let the joint mobilization movement, so they should first be heated up.
Who can perform Joint Mobilization?
- A joint mobilization is a format of manual therapy, thus manual therapists or manual therapy doctors will conduct it.
- The permitted and moral scope of training for a manual therapist to accomplish joint mobilization leans on the kind of joint mobilization, the kind of therapist, and where the therapist is training.
- Grade V quick-thrust joint mobilization is normally accomplished by chiropractic and osteopathic doctors, as well as physiotherapists (physical therapists) and occupational therapists. These therapists and doctors can even conduct all other Grades of joint mobilization.
What is the effect of Joint Mobilization?
Neurophysiological effects:
Facilitates mechanoreceptors to ache
Impact on muscle spasm and muscle defending through nociceptive stimulation
Boost in an understanding of position and movement due to afferent nerve stimulations
Nutritional effects:
Distraction/small gliding motions cause synovial fluid activity
Activity can enhance nutrient exchange because of joint swelling and stiffness
Mechanical effects:
Enhance flexibility of hypomobile joints
Sustains extensibility and tensile force of articular body tissues
Utilized to induce synovial fluid movement, carrying nutrients to the avascular parts of articular cartilage
Control the painful and degenerating impacts of stasis
What are the benefits of Joint Mobilization?
Joint mobilization can enhance the range of motion (ROM), decrease pain, and enhance the machinists of a joint to assist with things for example raising your arm, flexing your spine, and walking.
While the conceivable mechanisms of motion are even partially visionary, the advantages delivered by joint mobilization are additional concrete.
This therapy has been discovered to have a favorable effect on the pain levels related to many of the musculoskeletal illnesses defined above. Mobilizations have even been related to momentary gains in joint range of motion (ROM) and enhanced general balance responses.
It is worth noting, that these advantages are normally moderately quick-lived. Due to this the physiotherapist/chiropractor will generally utilize joint mobilizations in a duo with other therapies, such as strengthening/stretching, to optimize the general effect.
Indications for Joint Mobilization
There is mainly one indication for joint mobilization which is a hypomobile joint dysfunction.
The joint mobilization will mobilize a stiff joint, it would be instructed if the joint has immobile and decreased mobility, in other terms, is hypomobile.
A hypomobile joint dysfunction is usually defined in fixed words as being a subluxation, misalignment, and bone out of its normal anatomical place. Normally, mobility defeat and static malposition are associated with each other. But eventually, the conclusion indicates joint mobilization is a defeat of joint flexibility.
To decide if joint mobilization is right for any precise musculoskeletal pathologic illness, we must comprehend and examine the pathomechanics of the illness. If there is joint hypomobility affected, then joint mobilization is demonstrated.
- Shoulder pain or impingement
- Acute/chronic back pain
- Plantar fasciitis (inflammation of the wide band of tissue sprinting in the base of the foot and inducing heel pain)
- Hip osteoarthritis
- Lateral epicondylalgia (tennis elbow)
- Ankle sprains/instability
- Knee osteoarthritis
Risks of Joint Mobilization
Joint mobilizations are normally believed to be secure for most people. This procedure does include the application of force/pressure (occasionally with a raised speed) to a region of the body, yet. Due to this, there are some risks contained.
Individuals with underlying illnesses should exercise alert before undergoing joint mobilization:
- Uncontrolled diabetes/atherosclerosis
- Individuals consuming anticoagulant (blood thinner) drug
- Vertebrobasilar disease (inadequate blood flow to the brain branch)
- Hypermobility disorders/hereditary joint laxity (illness-inducing hypermobility from the period of birth)
- Local blood vessel aneurysm (bump in a blood vessel)
- Osteoporosis (breakable bones)/poor bone density
- Acute spinal disk herniation (a situation in the spine inducing extreme pain that restricts activity)
- Acute/unhealed fractures
If you have queries regarding whether joint mobilizations are suitable for your condition, must consult your doctor before undergoing any new therapies. In many patients, the risk of mobilization may be reduced by conducting law-power, more additional kind versions of the procedure.
Precautions for Joint Mobilization
There is mainly one precaution for joint mobilization which is a hypermobile joint dysfunction or other unstable joint/body tissue.
The joint mobilization will mobilize a joint, in other terms, improve its movement, then if the joint is already hypermobile/unstable, it would be contraindicated to joint mobilization.
Mobilizing joint demands establishes a physical power in the body, which impacts other adjoining body tissues, any body tissue fluctuation in the area would contraindicate or at least precautionary conducting the joint mobilization therapy. Such as a patient with osteoporosis/a herniated disc may not endure the physical force which is required to accomplish the mobilization approach.
Conclusion
Joint mobilization is a hands-on method utilized by physiotherapists and chiropractors. It includes the use of physical pressure on a stiff/aching joint. This therapy can enhance your range of motion (ROM) and activity during decreasing your pain. It is considered to do this by reducing the sensitivity/excitability of the body tissue in the affected joint.
FAQ
What are 5 methods to mobilize a stiff joint?
Training that is regarded as joint mobilization is an extension, flexion, tibiofemoral glide, patellar movement, elongate-axis distraction, and other activities such as lateral activity and spin. When managed appropriately, this training can significantly aid in relieving pain and in fixing joint play.
What is the principle of mobilization?
Provided regular, fit joint shells, the complete range of motion relies on the extensibility and mobility of the soft body tissue formats. This is particularly authentic for activities that must be lengthening M-F-N (myo-fascial-neural) structures over more than one joint.
Which are the 3 types of joint movement?
Gliding motions happen as moderately flat bone textures push beyond each other. Angular motions are constructed when the angle between the bones which form the joint changes. Rotational activity is the activity of a bone as it spins close to its own longitudinal axis.
What is the risk of joint mobilization?
Even though incredibly rare, risks of joint manipulation & mobilization may contain but aren’t restricted to Bone fracture. Boosted ache in the regaled joint/elsewhere in the body. Nerve injury/irritation.
What are two types of moving joints?
Ball-and-socket joints, for example, the shoulder and hip joints, permit backward, forward, sideways, and spinning motions. Hinge joints, for example, in the fingers, knees, elbows, and toes, permit only flexing and extending motions.d toes, permit only flexing and extending motions.
Is joint mobilization good for arthritis?
Joint Mobilization improves mechanisms of conditioned pain modulation in persons with osteoarthritis (OA) in the knee joint.






14 Comments