Posterior Ankle Impingement and Physiotherapy Management
- Posterior ankle impingement syndrome is one of the impingement syndromes involving the ankle. It is classically described in ballet dancers.
- Ankle impingement is defined as the entrapment of an anatomic structure that leads to pain and a decreased range of motion of the ankle and can be classified as either soft tissue or osseous.
- Posterior ankle impingement syndrome refers to a group of abnormal entities that result from repetitive or acute forced plantar flexion of the foot.
- Posterior ankle impingement is more common in ballet dancers and soccer players though it can be seen in any patient active in sports.
Anatomy related to Posterior ankle impingement
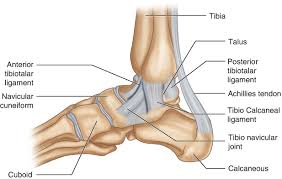
- A groove containing the flexor hallucis longus tendon along the posterior talus separates the medial and lateral tubercles of the posterior talus.
- The medial talocalcaneal and posterior tibiotalar ligaments insert upon the medial tubercle, whereas the lateral tubercle contains the attachment site of the posterior talofibular ligament.
- An intermalleolar ligament is present in most individuals, most commonly coursing from the medial malleolus to the lateral malleolus near the fibular attachment of the posterior talofibular ligament.
- The lateral tubercle of the talus, when elongated, is referred to as Stieda’s process. In addition, the lateral tubercle may articulate with a separate ossification center known as the os trigonum.
- The os trigonum is corticated and articulates with the lateral tubercle via a synchondrosis.
- The posterior surface of the os trigonum is non-articular but serves as a point of attachment for capsuloligamentous structures, in particular the posterior talofibular and posterior talocalcaneal ligaments.
Etiology of Posterior ankle impingement
- Posterior ankle impingement may complicate an acute traumatic plantar hyperflexion event, such as an ankle sprain, or may be related to repetitive low-grade trauma associated with plantar hyperflexion, especially as can be seen in the female ballet dancer.
- The more common causes are osseous in nature, such as the os trigonum, an elongated posterolateral tubercle of the talus, a downward sloping posterior lip of the tibia, an osteophyte from the posterior distal tibia, or a prominent posterior process of the calcaneus.
Clinical features of Posterior ankle impingement
- Patients who have posterior impingement complain of chronic deep posterior ankle pain worsened by forced plantar flexion or push-off forces as occur during activities such as ballet dancing, jumping, or running downhill.
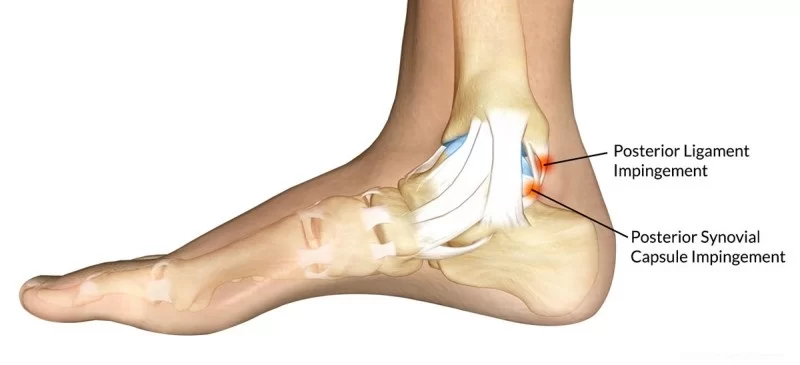
- In such positions, compression of soft tissue or bony structures between the posterior aspect of the distal tibia and calcaneus or between the posterior tibia and the posterolateral process of the talus can occur. In some patients, forced dorsiflexion is also painful.
- In this dorsiflexed position, traction is applied to the posterior joint capsule and posterior talofibular ligament, which both attach to the posterolateral talar process.
Diagnosis of Posterior ankle impingement
- MRI: imaging also depicts inflammatory changes in the soft tissues of the posterior ankle-namely, the posterior synovial recess of the subtalar and tibiotalar joints with posterior capsular thickening, a fluid-distended posterior joint space, and increased T2-weighted signal along the posterior margin of the ankle indicative of synovitis.
Examination
- It reveals pain on palpation over the posterolateral talar process, which is located along the posterolateral aspect of the ankle between the Achilles and peroneal tendons.
- Passive forced plantar flexion results in pain and often a grinding sensation as the posterolateral talar process is entrapped between the posterior tibia and calcaneus.
- The diagnosis can be confirmed if pain abates following the injection of an anesthetic into the posterolateral capsule of the tibiotalar joint.
Treatment of Posterior ankle impingement
Limitation:
- The first advice that has to be given to the patient is that he or she should stop any activity that increases pain, this allows the body to start the healing process without further tissue damage while at the same time preventing a worsening of the situation and the problem becoming chronic.
- Later on, an activity can gradually start building up before returning to its original levels.
- Alternative exercises can be used that generate less force on the ankle, this includes; swimming, cycling, water sports, etc.
- Another option is to use a slightly raised heel, this means that the foot does not need to go as far up as normal. The use of crutches is another method to prevent further damage to the ankle.
- Reducing Pain:
- Cryotherapy is an effective way of managing the pain created by AIS. Based on the available evidence, cryotherapy seems to be effective in decreasing pain.
- In comparison with other rehabilitation techniques, the efficacy of cryotherapy has been questioned.
- Additionally, the low methodological quality of the available evidence is of concern. Many more high-quality studies are required to create evidence-based guidelines on the use of cryotherapy.
- These must focus on developing modes, durations, and frequencies of ice application that will optimize outcomes after injury.
- Anti-inflammatory medication reduces pain and supports the healing process.
- Corticoid injection: An occasional injection of corticosteroids into the ankle joint may be helpful particularly if there is some underlying ankle arthritis present.
- Surgery:
- In some instances of AIS, operative treatment may be helpful. If the main cause of a patient’s symptoms is from impingement (rather than ankle arthritis) removing the prominent impinging bony spurs can relieve symptoms.
- Surgical treatment of ankle impingement involves removing the prominent bone spurs either by arthroscopic surgery or by opening up the ankle joint with an incision.
- If the bone spurs are large it is often easier and faster to simply open up the ankle joint and remove the bone spurs rather than attempt to do this arthroscopic.
- Surgery to remove impinging bone spurs from the front of the ankle will not typically help symptoms if the pain is generalized around the ankle due to significant ankle arthritis rather than specifically located in the front of the ankle.
- In some instances, surgery to remove the bony spurs can make a patient’s symptoms worse if it allows the ankle joint to move more and the ankle joint itself has significant arthritis.
- The bony spurs themselves will tend to grow back over time. Recurrence of symptoms is not uncommon.
- At long-term follow-up, arthroscopic excision of both soft-tissue overgrowths and osteophytes was shown to be an effective way of treating anterior impingement, provided that there was no preoperative narrowing of the joint space.
- Other Management Options:
- Soft tissue massage can help reduce pain.
- Use of heat improves blood circulation and stimulates the healing process
- Taping/Bracing of the ankle helps to control movement and support the natural structure of the ankle.
- These methods are questionable as there is a lack of detailed research supporting their use meaning it is not supported by evidence-based practice, one of the core principles of physiotherapy.
Physiotherapy Management
- Phase 1 of recovery: inflammation 0-3 days

- Rest and immobilization, but a frequent movement within pain limits.
- Use pain as a guideline to base you’re exercising on.
- Eating behaviors (vitamin C, proteins, anti-oxidants,…).
- Exercise basic functions, move feet and toes to improve blood circulation.
- Limit painkillers to the bare minimum.
- Phase 2 of recovery: limited functionality 4-10 days
- Mobilization to improve scar tissue quality.
- Muscle endurance training within free ROM.
- Proprioceptive training.
- Train muscle strength of “foot raiser muscles” (tricep surae muscles or the plantar flexor muscles.
- The gastrocnemius and soleus muscles) using more weight and less repetitions.
- Normal ROM should be reached.
- Phase 3 of recovery: early revalidation 11-21 days
- Mobilizations with a progressively enhancing ROM
- Proprioceptive training
- Muscle strength training
- Research and estimate the level of daily activity, modify therapy with this info
- Phase 4 of recovery: late revalidation 3-6 weeks

- Improve load capacity, running and climbing stairs.
- Coordination training with ADL.
- The goal is to end exercises with a load like before the incident.
- Progressive build-up of schedule: static? dynamic/selective? functional.
- Phase 5 of recovery: early sporting: 6-8 weeks
- Phase 6 of recovery: late sporting starting week 8
- Improve sporting: Practice and improve functions and activities based on sports. Sufficient rest and repair moments
- Prevention: It is recommended to improve the awareness of injury prevention strategies for players and athletes.
- These strategies were identified as the use of shin pads during training, carbohydrate intake before and after training and after matches, cool downs after training and matches, and flexibility work
FAQs
How do you treat a posterior ankle impingement?
Physical therapy and avoiding problematic activity are the initial lines of treatment if posterior ankle impingement is found. From time to time, a walking boot or cast might be applied to reduce inflammation and limit ankle motion. Anti-inflammatory drugs and ice can also be helpful.
Which tissue is responsible for posterior ankle impingement?
The most frequent source of posterior ankle impingement with symptoms is the os trigonum. Posteromedial impingement: Scar tissue made up primarily of posterior fibers is the main cause of chronic posteromedial pain.
How do you get rid of ankle impingement pain?
To rid of ankle impingement pain:
Pain-Relieving Drugs: Ibuprofen and other anti-inflammatory medications
Utilizing a heat and cold pack.
Applying cold packs or Hot packs for 10 to 15 minutes every two to three hours is recommended, as well as following any activity that increases symptoms.
Ankle Strap
Physical Therapy
Ankle Exercise
Injection.
Rarely Surgery.
Does posterior ankle impingement go away?
Whether you choose non-surgical or surgical therapy for posterior ankle impingement, it may take up to 12 weeks to fully heal.



One Comment