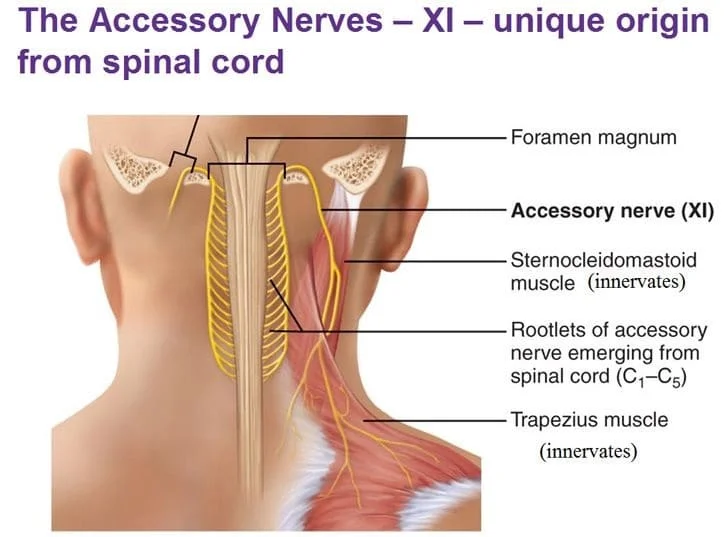
SPINAL ACCESSORY NERVE
Introduction
The accessory nerve is a cranial nerve that supplies the sternocleidomastoid and trapezius muscles.
It is considered the eleventh of twelve pairs of cranial nerves, or simply cranial nerve XI, as part of it was formerly believed to originate in the brain.
The accessory nerve divides it into a spinal part and a cranial part.
The fibers arising from the intracranial component are known as the cranial accessory nerve, while those fibers arising from the spinal nucleus are called the spinal accessory nerve.
ANATOMY OF SPINAL ACCESSORY NERVE
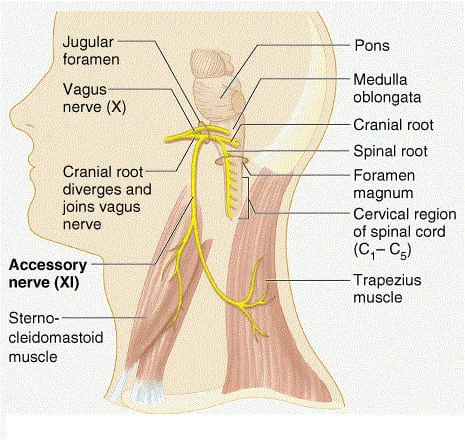
The accessory nerve is divided into spinal and cranial parts.
Spinal Component
The spinal portion arises from neurons of the upper spinal cord, specifically C1-C5/C6 spinal nerve roots.
These fibres coalesce to form the spinal part of the accessory nerve, which then runs superiorly to enter the cranial cavity via the foramen magnum.
The nerve traverses the posterior cranial fossa to reach the jugular foramen.
It briefly meets the cranial portion of the accessory nerve, before exiting the skull (along with the glossopharyngeal and vagus nerves).
Outside the cranium, the spinal part descends along the internal carotid artery to reach the sternocleidomastoid muscle, which it innervates.
It then moves across the posterior triangle of the neck to supply motor fibres to the trapezius.
Cranial Component
The cranial portion is much smaller and arises from the lateral aspect of the medulla oblongata.
It leaves the cranium via the jugular foramen, where it briefly contacts the spinal part of the accessory nerve.
Immediately after leaving the skull, the cranial part combines with the vagus nerve (CN X) at the inferior ganglion of the vagus nerve (a ganglion is a collection of nerve cell bodies).
The fibres from the cranial part are then distributed through the vagus nerve. For this reason, the cranial part of the accessory nerve is considered part of the vagus nerve.
STRUCTURE
- The fibres of the spinal accessory nerve originate solely in neurons situated in the upper spinal cord, from where the spinal cord begins at the junction with the medulla oblongata, to the level of about C6.
- These fibres join together to form rootlets, roots, and finally the spinal accessory nerve itself.
- The formed nerve enters the skull through the foramen magnum, the large opening at the skull’s base.
- The nerve travels along the inner wall of the skull towards the jugular foramen.Leaving the skull, the nerve travels through the jugular foramen with the glossopharyngeal and vagus nerves.
- The spinal accessory nerve is notable for being the only cranial nerve to both enter and exit the skull.
- This is due to it being unique among the cranial nerves in having neurons in the spinal cord.
- After leaving the skull, the cranial component detaches from the spinal component.
- The spinal accessory nerve continues alone and heads backward and downwards. In the neck, the accessory nerve crosses the internal jugular vein around the level of the posterior belly of the digastric muscle.
- As it courses downwards, the nerve pierces through the sternocleidomastoid muscle while sending it motor branches, then continues down until it reaches the trapezius muscle to provide motor innervation to its upper part.
Nucleus
- The fibres that form the spinal accessory nerve are formed by lower motor neurons located in the upper segments of the spinal cord.
- This cluster of neurons called the spinal accessory nucleus, is located in the lateral aspect of the anterior horn of the spinal cord.
- And stretches from where the spinal cord begins (at the junction with the medulla) through to the level of about C6.
- The lateral horn of high cervical segments appears to be continuous with the nucleus ambiguus of the medulla oblongata, from which the cranial component of the accessory nerve is derived.
Embryology
The XI nerve and the vagus nerve both originated from the same ganglionic crest (ectoderm) during embryological development. Both sensitive and motor components are present in the construction. Its caudal terminus gains additional motor functions and its cranial end gets more sensitive as development goes on.
The ganglion crest lateralizes and splits into a right and left portion at around 20 days. The caudal portion of the crest gives rise to a band of fibers that will eventually become the accessory nerve. The level of the fourth, fifth, and sixth cervical segments corresponds to this band of fibers.
In the fourth week, it breaks away from the vagus nerve’s attachment and launches itself into the sternocleidomastoid muscle, a mesodermal mass. The nerve, which connects to the future spinal cord at irregular intervals, is situated medial to the dorsal rootlets near the end of the fifth week of pregnancy. It is joined to the primary spinal ganglion.
A row of ganglia located in the nerve after it has formed makes up the cranial section. Larger ganglia will grow during development and connect to the vagus nerve’s jugular ganglion.
The XI nerve extends and assumes its shape in the second and third months.
Blood Supply
The posterior inferior cerebellar artery’s proximal, distal, and recurrent branches supply blood to the intracranial section of the nerve. The musculospiral artery of the ascending pharyngeal artery and the collaterals of the anterior spinal artery both have an impact on the spinal roots of the nerve.
The occipital artery and the lingual artery’s branches supply blood supply to the extracranial area.
Lymphatic Drainage
Lymphatic nodes line the nerve’s extracranial journey at the level of the posterior triangle of the neck; the external jugular vein is affected by the venous system, which traces the nerve’s complete course through tiny veins.
Nerves
The auxiliary nerve and the root of C1 are anastomose; nonetheless, contradictory writings also refer to C2-C3. The function of the intriguing anastomosis between the stellate ganglion and the IX is unknown.
When it emerges from the jugular foramen, it also exchanges messages with a branch of the large auricular nerve. The XI has a lipostomosis (anastomosis with the vagus) at the level of the C1 transverse process’ upper margin.
Variation
- In the neck, the accessory nerve crosses the internal jugular vein around the level of the posterior belly of the digastric muscle, in front of the vein in about 80% of people, and behind it in about 20%, and in one reported case, piercing the vein.
- The accessory nerve is described as having a small cranial component that descends from the medulla and briefly connects with the spinal accessory component before branching off of the nerve to join the vagus nerve.
- This cranial component does not make any distinct connection to the spinal component the roots of these distinct components were separated by a fibrous sheath in all but one subject.
DEVELOPMENT
The accessory nerve is derived from the basal plate of the embryonic spinal segments C1–C6.
SPINAL ACCESSORY NERVE FUNCTIONS
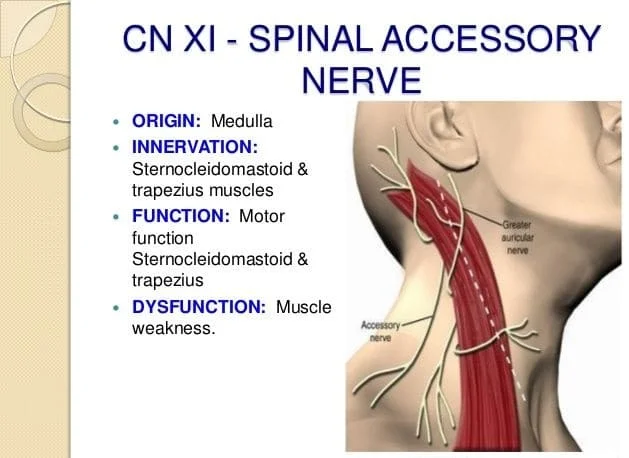
Motor Function:
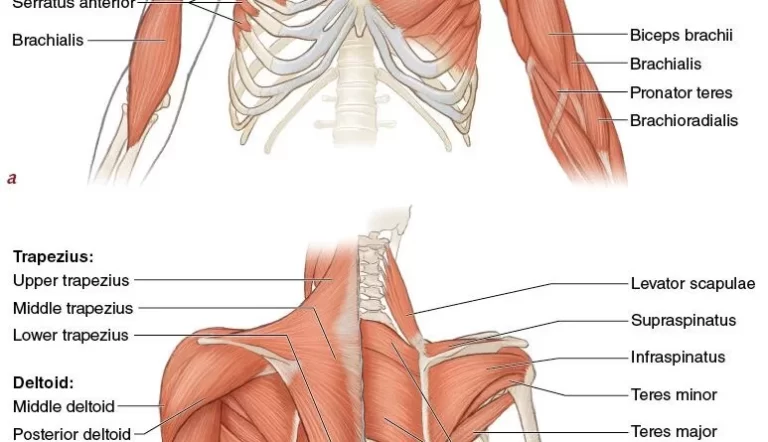
The spinal accessory nerve innervates two muscles – the sternocleidomastoid and trapezius.
Sternocleidomastoid:
Attachments: Runs from the mastoid process of the temporal bone to the manubrium (sternal head) and the medial third of the clavicle (clavicular head).
Actions: Lateral flexion and rotation of the neck when acting unilaterally, and extension of the neck at the atlanto-occipital joints when acting bilaterally.
Trapezius:
Attachments: Runs from the base of the skull and the spinous processes of the C7-T12 vertebrae to the lateral third of the clavicle and the acromion of the scapula.
Actions: It is made up of upper, middle, and lower fibres.
The upper fibres of the trapezius elevate the scapula and rotate it during the abduction of the arm.
The middle fibres retract the scapula and the lower fibres pull the scapula inferiorly.
Clinical Importance
EXAMINATION
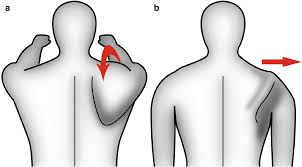
- The accessory nerve is tested by evaluating the function of the trapezius and sternocleidomastoid muscles.
- The trapezius muscle is tested by asking the patient to shrug their shoulders with and without resistance.
- The sternocleidomastoid muscle is tested by asking the patient to turn their head to the left or right against resistance.
- One-sided weakness of the trapezius may indicate injury to the nerve on the same side or injury to the spinal accessory nerve on the same side (Latin: ipsilateral) of the body being assessed.
- Weakness in head-turning suggests injury to the contralateral spinal accessory nerve: a weak leftward turn is indicative of a weak right sternocleidomastoid muscle (and thus right spinal accessory nerve injury).
- A weak rightward turn is indicative of a weak left sternocleidomastoid muscle (and thus left spinal accessory nerve).
- Weakness of shrug on one side and head-turning on the other side may indicate damage to the accessory nerve on the side of the shrug weakness or damage along the nerve pathway at the other side of the brain.
- Causes of damage may include trauma, surgery, tumours, and compression at the jugular foramen.
- Weakness in both muscles may point to a more general disease process such as amyotrophic lateral sclerosis, Guillain–Barré syndrome, or poliomyelitis.
Injury:
- Injury to the spinal accessory nerve commonly occurs during neck surgery, including neck dissection and lymph node excision.
- It can also occur as a result of blunt or penetrating trauma, and in some cases spontaneously.
- Damage at any point along the nerve’s course will affect the function of the nerve.
- The nerve is intentionally removed in “radical” neck dissections, which are attempts at exploring the neck surgically for the presence and extent of cancer.
- Attempts are made to spare it in other forms of less aggressive dissection.
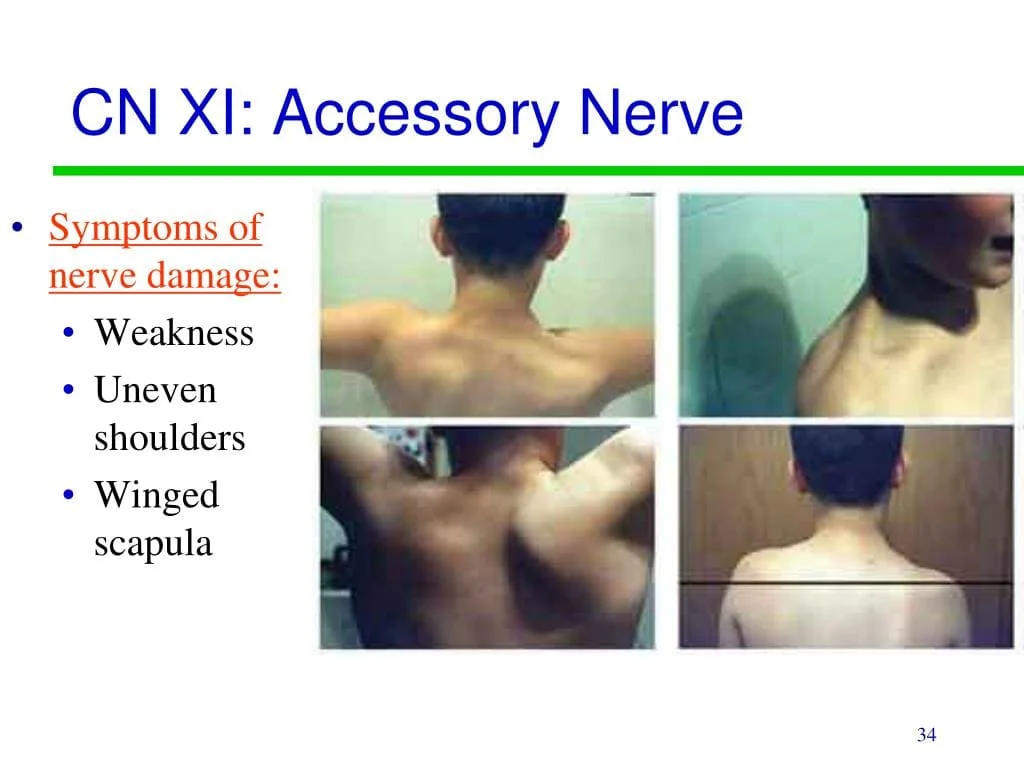
- Injury to the accessory nerve can result in neck pain and weakness of the trapezius muscle. Symptoms will depend on at what point along its length the nerve was severed.
- Injury to the nerve can result in shoulder girdle depression, atrophy, abnormal movement, a protruding scapula, and weakened abduction.
- Weakness of the shoulder girdle can lead to traction injury of the brachial plexus. Because diagnosis is difficult, electromyogram or nerve conduction studies may be needed to confirm a suspected injury.
Palsy of the Accessory Nerve:
- The most common cause of accessory nerve damage is iatrogenic (i.e. due to a medical procedure).
- In particular, operations such as cervical lymph node biopsy or cannulation of the internal jugular vein can cause trauma to the nerve.
- Clinical features include muscle wasting and partial paralysis of the sternocleidomastoid, resulting in the inability to rotate the head or weakness in shrugging the shoulders.
- Damage to the muscles may also result in an asymmetrical neckline.
Physical therapy
The application of electrostimulation to the sternocleidomastoid and trapezius muscles should be part of nerve rehabilitation. Proprioceptive exercises should be combined with specific exercises to actively engage the muscles.
Osteopathy
When there are scars present, an osteopathic method may help the tissues slide more smoothly. Studies in various clinical circumstances suggest that it might be helpful in lowering blood levels of inflammation or pain.




2 Comments