Anterocollis (AC)
What is a Anterocollis (AC)?
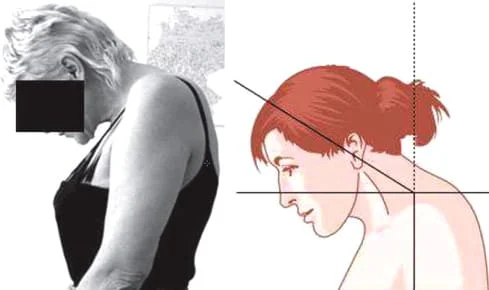
Anterocollis (AC) is a medical term used to describe a specific type of dystonia characterized by involuntary forward flexion of the neck and head.
When compared to anterocaput, anterocollis can be distinguished by the abnormal angle between the thoracic and cervical spines or between the skull base and vertebrum-1.
There are two types of anterocollis/anterocaput: primary (idiopathic) and secondary (caused by a known neurological condition). Complex anterocollis is most usually accompanied by torticollis or laterocollis, two other forms of focal dystonia.
Patients indicate that they periodically release the fixed head position by using a “geste antagonistique” and complain about impaired head movement. A neurological test reveals tonic (anteflexive contractures) or trembling head motions and neck posture. The clinical presentation, a needle-electromyography to identify the affected muscles and rule out other disorders, a cervical/thoracic spine X-ray, and a cerebral MRI are used to make the diagnosis.
In the case of anterocollis, the muscles in the front of the neck contract uncontrollably, causing the head and neck to tilt forward.
Treatment for anterocollis may include medications, botulinum toxin injections to relax affected muscles, physical therapy, and, in some cases, surgical interventions like deep brain stimulation (DBS) to manage symptoms.
Introduction
A neurological disorder called dystonia is characterized by uncontrollable, patterned (stereotypical), persistent (spasmodic), or repetitive muscular spasms that cause unnatural head movements or abnormal postures. Overflow dystonia is the phenomenon in which dystonic contractions start in one part of the body but spread to another.
Muscles in the affected area move more slowly and have a smaller range of motion when acting voluntarily. These strange motions may start off being moderate, but as the condition progresses, they could become more severe and recurring. A localized, segmental, multifocal, or widespread distribution of dystonia is possible. Cervical dystonia (spasmodic torticollis), the most prevalent type of focal dystonia, is a condition.
Torticollis and torticaput are the most frequent abnormal head positions in cervical dystonia, followed by latero-flexion and laterocaput, head extension and retrocaput, and head flexion and anterocollis.
The goal of this article, which focuses on anterocollis/anterocaput, is to give readers an overview of current research and body of knowledge related to the condition’s cause, pathophysiology, symptoms, diagnosis, and management as a subtype of cervical dystonia.
Classification of Anterocollis
A causally diverse abnormality of head posture known as anterocollis/anterocaput manifests as involuntary, non-fixed anteflexion of the head and is commonly accompanied by pain. Either as a descriptive or causative term, anterocollis is utilized. The phrases “anterocollis” and “dropped head” or “head ptosis” are often used interchangeably as descriptive descriptors.
Anterocollis can be either primary or secondary. Primary anterocollis occurs without an underlying cause and is considered idiopathic.
Secondary anterocollis is associated with an underlying condition, such as Parkinson’s disease, certain medications, or other neurological disorders.
Symptoms of Anterocollis
Symptoms, including:
- Forward bending of the neck: The head and neck may be pulled forward, making it difficult for the individual to maintain an upright posture.
- Neck pain: The sustained contraction of neck muscles can lead to discomfort and pain in the affected area.
- Difficulty with activities of daily living: Anterocollis can interfere with tasks like reading, eating, and maintaining eye contact with others.
- Impaired quality of life: This condition can have a significant impact on an individual’s quality of life due to the physical and social challenges it presents.
Later on, patients complain about their inability to extend their neck voluntarily, about slow head motions, or their inability to move. In order to relieve the fixed head posture, a technique known as “geste antagonistique” is used to trick the patients’ senses.
A voluntary maneuver that momentarily lessens the severity of dystonic posture or movements is known as a geste antagonistique.
Course
Most of the time, it is difficult to forecast how an anterocollis will develop naturally. However, in the majority of people, anterocollis deteriorates over the first five years, remains stable for the following five years, and then tends to improve beyond that. Some people may experience dystonic head tremor, which occasionally responds favorably to a geste antagonistic. Dystonia can spread outside the cervical region in some cases.
Epidemiology
There is a lack of information in the literature regarding the incidence and prevalence of cervical dystonia in general and anterocollis/anterocaput in particular. In a retrospective analysis of 399 cervical dystonia patients, 27 patients (6.8%) were found to have anterocollis, without being specific about whether it was pure or complex.
Anterocollis was identified as the primary factor in 1% of 404 people with idiopathic cervical dystonia in research.
Causes of Anterocollis
Anterocollis (AC), a type of dystonia characterized by involuntary forward flexion of the neck and head, can have various underlying causes. Dystonia, in general, is a neurological movement disorder characterized by muscle contractions that cause repetitive or twisting movements and abnormal postures.
Here are some common causes and factors associated with anterocollis:
- Primary (Idiopathic) Dystonia: In many cases, anterocollis occurs as primary or idiopathic dystonia, meaning there is no clear underlying cause. It can be considered a focal or segmental dystonia, primarily affecting the neck muscles.
- Secondary Dystonia: Anterocollis can also be secondary to other medical conditions or factors, including:
- Parkinson’s Disease: Anterocollis can develop as a secondary symptom in some individuals with Parkinson’s disease.
- Medication-Induced Dystonia: Certain medications, particularly dopamine-blocking drugs used to treat psychiatric conditions or nausea, can induce dystonic symptoms, including anterocollis.
- Brain Injury or Trauma: Head injuries or trauma to specific brain regions can sometimes lead to dystonia, including anterocollis.
- Infections: Rarely, infections of the central nervous system, such as encephalitis, can result in dystonic symptoms.
- Vascular Issues: Reduced blood flow to specific areas of the brain can lead to dystonia, although this is less common.
- Genetic Factors: In some cases, genetic mutations have been associated with the development of primary dystonias, including anterocollis.
- Environmental Factors: While not a direct cause, environmental factors, such as stress, fatigue, or exposure to certain chemicals, can exacerbate dystonic symptoms in individuals who already have the condition.
- Unknown Causes: In some instances, despite thorough medical evaluation, the exact cause of anterocollis may remain unknown.
Diagnosis
Based on the normal symptoms and indicators, anterocollis/anterocaput can be diagnosed. Usually, the head is anteflected and the movements are restricted or monotonous.
X-rays of the head, neck, or thoracic spine, needle electromyography (EMG), ultrasound, CT scan, MRI, and PET are all helpful instrumental examinations for the diagnosis of anterocollis.
EMG may be useful to show persistent involuntary contractions, identify the affected muscles (EMG-guidance), and rule out other possible causes.
Differential Diagnoses
When diagnosing medical conditions like anterocollis (AC), healthcare professionals often consider a range of possible differential diagnoses to rule out other conditions with similar symptoms. Differential diagnosis is the process of distinguishing one condition from others that may have overlapping clinical features.
Here are some potential differential diagnoses for anterocollis:
Cervical Dystonia (Primary Anterocollis):
Primary or idiopathic anterocollis is a subtype of cervical dystonia. In this case, the differential diagnosis mainly involves ruling out other types of dystonia and conditions that cause abnormal neck postures.
Secondary Dystonia:
Secondary dystonia can occur as a result of underlying medical conditions or factors. Differential diagnoses may include:
- Parkinson’s disease
- Medication-induced dystonia (due to certain drugs)
- Traumatic brain injury
- Encephalitis or other central nervous system infections
- Vascular lesions in the brain
Muscle Disorders:
Certain muscle disorders can lead to abnormal neck postures. These may include:
Myopathy (muscle diseases)
Muscle spasms or myoclonus
Neuropathies:
Conditions affecting the nerves that control neck muscles can result in abnormal neck postures. Differential diagnoses may include:
- Neuropathies due to diabetes or other causes
- Guillain-Barré syndrome
- Amyotrophic lateral sclerosis (ALS)
Psychogenic Dystonia:
In some cases, psychological factors can lead to abnormal neck postures. Psychogenic dystonia should be considered when there is no clear organic cause.
Structural Abnormalities:
Structural issues in the spine or neck, such as cervical spine deformities, tumors, or herniated discs, can cause neck posture abnormalities. Imaging studies like MRI may be necessary to rule out these causes.
Movement Disorders:
Other movement disorders, such as Tourette syndrome or tardive dyskinesia, can sometimes manifest with abnormal neck movements. Careful clinical evaluation is needed to differentiate them from anterocollis.
Infections and Inflammatory Conditions:
Conditions like rheumatoid arthritis or infections affecting the joints or tissues around the neck may lead to abnormal neck postures.
Autoimmune Disorders:
Certain autoimmune diseases can involve muscle weakness or stiffness, potentially affecting neck posture.
Psychiatric Disorders:
Some psychiatric conditions, such as conversion disorder or somatic symptom disorder, may manifest with physical symptoms, including abnormal neck postures.
Treatment of Anterocollis (AC)
The treatment of Anterocollis (AC) depends on its underlying cause, severity, and the individual patient’s specific needs. Since anterocollis is often a manifestation of dystonia, the treatment approaches may overlap with those used for dystonia in general. Here are some common treatment options:
Medications:
Botulinum Toxin Injections: Botulinum toxin injections, commonly known as Botox injections, can be effective in treating anterocollis. The toxin is injected directly into the affected muscles to temporarily weaken them, reducing muscle contractions and abnormal neck posture. Over time, numerous injections can be necessary.
Oral Medications: Some medications, such as anticholinergics (e.g., trihexyphenidyl), muscle relaxants (e.g., baclofen), or medications that affect dopamine levels (e.g., levodopa), may be prescribed to help manage dystonic symptoms. However, their effectiveness can vary, and they may have side effects.
Physical Therapy: Physical therapy and targeted exercises can help improve posture, alleviate discomfort, and enhance muscle control. A physical therapist can create a tailored exercise program to address specific needs.
Occupational Therapy: Occupational therapists can assist in finding strategies and adaptive devices to help individuals with anterocollis perform daily tasks more comfortably and effectively.
Sensory Tricks (Sensory Gestes): Some individuals with dystonia, including anterocollis, find relief by employing sensory tricks or gestes. These are simple maneuvers or touches that temporarily reduce muscle contractions. For example, lightly touching the chin may briefly alleviate the forward neck flexion.
Deep Brain Stimulation (DBS): In severe cases of anterocollis that do not respond to other treatments, deep brain stimulation may be considered. It involves implanting electrodes in specific brain regions and delivering electrical impulses to modulate abnormal muscle activity.
Alternative Therapies: Some people explore complementary and alternative therapies such as acupuncture, biofeedback, or relaxation techniques to manage dystonic symptoms. Some people may find relief with these strategies.
Psychological Support: Living with a chronic movement disorder like anterocollis can be challenging emotionally and psychologically. Counseling or support groups can offer valuable emotional support and coping strategies.
Surgical Interventions: In very rare and severe cases, surgery may be considered. Surgical procedures like selective peripheral denervation involve cutting specific nerves to reduce muscle contractions. These options are typically considered only when other treatments have been ineffective.
Working closely with a medical team that may include neurologists, physical therapists, and other specialists is crucial for people with anterocollis. To maximize symptom control, treatment programs should be customized to the individual’s specific requirements and frequently reevaluated.
Physiotherapy Treatment
An important part of the treatment for people with anterocollis (AC) or any other type of dystonia affecting the neck and head is physical therapy (PT). Physical therapists can offer specialized care to assist in enhancing muscular control, reducing pain, and maximizing functional abilities.
Exercise to Correct Anterocollis (AC)
Range of Motion Exercises:
Gentle range of motion exercises are used to improve neck mobility and flexibility. These exercises help counteract the forward flexion of the neck.
Neck Flexion and Extension Stretch: Sit or stand with your back straight. Gently tilt your head forward (flexion) to stretch the back of your neck, then tilt your head backward (extension) to stretch the front of your neck. Repeat these movements slowly and smoothly.
Neck Rotation: Turn your head to the right, bringing your chin toward your right shoulder. Hold for a few seconds, then return to the center and repeat on the left side.
Strengthening Exercises:
Strengthening exercises are designed to target the muscles involved in neck flexion and extension. Strengthening the opposing muscles can help balance muscle tone and improve posture.
Chin Tucks: Straighten your back while you stand or sit. Create a “double chin” impression by gently tucking your chin in toward your chest. Hold for a short while, then let go. Repeat several times.
Neck Extension: Sit or stand with your back straight. Slowly and gently lift your head upward, looking towards the ceiling. Hold for a few seconds and then lower your head. Repeat this exercise.
Breathing and Relaxation Exercises:
Deep breathing exercises and relaxation techniques can help reduce muscle tension and promote overall relaxation, which can be beneficial in managing dystonic symptoms.
Postural Training:
Physical therapists work with patients on maintaining correct posture during daily activities. They may use mirrors, cues, or posture braces to help patients develop and maintain proper alignment.
Manual Therapy:
Hands-on techniques such as massage, myofascial release, and joint mobilization may be used to alleviate muscle tension and promote relaxation.
Modalities:
Physical therapists may use modalities such as heat, cold, or electrical stimulation to manage pain and improve muscle function.
Sensory Tricks:
The therapist may teach sensory tricks or gestes that the patient can use to temporarily alleviate muscle contractions and maintain a more normal head and neck position.
Functional Training:
Patients work on functional tasks related to their daily lives. This may include activities like eating, grooming, and getting in and out of chairs, with a focus on improving independence.
Home Exercise Program:
Physical therapists often prescribe a customized home exercise program that patients can perform independently to reinforce the gains made during therapy sessions.
Progress Monitoring:
The therapist will regularly assess the patient’s progress and make adjustments to the treatment plan as needed to optimize outcomes.
Outcome
Patients often have a decent, long-term quality of life in terms of their health. The response to treatment is only bad in a small number of people. Pallidal deep brain stimulation should be taken into consideration, especially in the latter cases.
Anterocollis was discovered as a predictor of spreading in a logistic regression model in a study of 73 cervical dystonia patients.
Summary
Anterocollis (AC) is a type of dystonia characterized by involuntary forward flexion of the neck and head. Treatment options include medications, botulinum toxin injections, physical therapy, and, in severe cases, deep brain stimulation (DBS).
Exercise, tailored to an individual’s needs, can also help improve posture and muscle control, but it should be done under professional guidance. Treatment plans should be personalized, and progress may require ongoing effort and monitoring.
FAQs
What muscles are involved in anterocollis?
The specific muscles affected can vary from person to person, but some of the key muscles that may be involved in anterocollis include:
Sternocleidomastoid Muscles (SCM)
Scalene Muscles: The scalene muscles are a group of three muscles (anterior, middle, and posterior) located on each side of the neck.
Longus Colli Muscles: These deep neck muscles are responsible for flexing and rotating the neck.
Platysma Muscle
Various other smaller neck muscles can also be involved in anterocollis, depending on the specific patterns of muscle contractions and dystonia in each individual.
What is Antecollis in Parkinson’s disease?
Disproportionate antecollis is a term used to describe a forward flexion of the head and neck that is more pronounced than would be expected given the flexed posture of the body’s trunk and limbs in Parkinsonian illnesses.
Is torticollis Antecollis or Retrocollis?
Torticollis (neck rotation), anterocollis (head-ahead flexion or pulled forward), retrocollis (head-posterior extension or pulled backward), or laterocollis (head tilt or lateral flexion) are the four types of Cervical Dystonia that can be distinguished based on head posture.
References
Finsterer, J., & Revuelta, G. J. (2014, December 1). Anterocollis and anterocaput. Clinical Neurology and Neurosurgery; Elsevier BV. https://doi.org/10.1016/j.clineuro.2014.09.020