Cerebellar Ataxia
Definition:
- Ataxia is a neurological sign consisting of a lack of voluntary coordination of muscle movements that includes gait abnormality. Ataxia is a non-specific clinical manifestation implying dysfunction of the parts of the nervous system that coordinate movement, such as the cerebellum.
- Ataxia is a lack of muscle coordination which may affect speech, eye movements, the ability to swallow, walking, picking up objects, and other voluntary movements.
- Many different things can cause ataxia, including multiple sclerosis, head trauma, alcohol abuse, stroke, cerebral palsy, genetics, or tumor. Ataxia may also be a symptom associated with certain infections.
- The co-ordination movement depends on:
- (1) Cerebellum and its connection: Cerebellar ataxia (Ataxia gait, limb in-coordination, tremor, dysarthria, nystagmus).
- (2) Sensory feedback: Sensory ataxia (ataxia of gait and limb at the dark, loss of proprioception, +ve Romberg test).
Cerebellum:
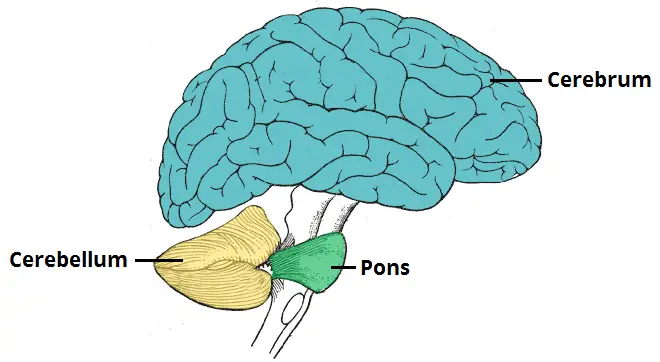
- Role of the cerebellum:
- Initiation & control of voluntary movement.
- Timing of movement/muscle action.
- Moment-to-moment correction of errors.
- Compensating for lesions of the cerebral cortex.
- Motor learning & adaptive adjustments.
- Etiology:
- Developmental abnormality (hydrocephalus or hypoxia at birth).
- Traumatic brain injury.
- Stroke.
- Tumor or other space-occupying lesion.
- Infection (encephalitis).
- Demyelinating disease (Multiple sclerosis).
- Familial or hereditary disease (Friedreich’s ataxia).
- Degenerative disease.
- Metabolic disease (myxoedema, Wilson’s disease).
- Vascular disease (vertebro-basilar artery insufficiency).
- Drug & alcohol intoxications.
- Types of cerebellum:
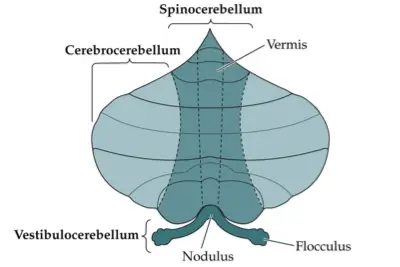
- (1) Vestibulocerebellum:
- Input: Vestibular, visual path.
- Output: Feedback to the vestibular nuclie.
- Lesion: Disturbe equilibrium, wide base gait, nystagmus.
- Vestibulo-cerebellar system modulating vestibular influences on posture & eye movement.
- (2) Spinocerebellum:
- Input: Somatosensory via the spinal cord.
- Output: Brain stems reticular, lateral vestibular nuclie.
- Lesion: Vermis truncal ataxia, lateral limb ataxia.
- Spino-cerebellar system regulating muscle tone, posture & locomotion.
- (3) Cerebrocerebellum:
- Input: Cortico pontine.
- Output: Feedback dentate, thalamus, cortex motor, premotor.
- Lesion: Impair complex voluntary movement, smooth and persize.
- Cerebro-cerebellar system regulating skilled movement.
Causes of Ataxia:
- (1) Acquired:
- (2) Hereditary: (a) Known metabolic defect and (b) Unknown metabolic defect.
- Acquired causes:
- Infection: posterior fosse abscess, cerebellitis.
- Vascular: Hge, infarction, TIA
- Demyelinating: Multiple sclerosis, Sensory PN(Miller Fisher).
- Malignancy: Tumor.
- Toxin and drug: INH, lithium, cyclosporin, cystosine arabiniside, phyntoin, procainamide.
- Paraneoplastic.
- Metabolic: Vitamin E deficiency, hypothyroidism.
- Hereditary causes:
- Ataxia is a prominent feature
- Intermittent:
- Hyperammonimea,aminoacidurea,disorder of pyrvate &lactate
- Progressive:
- Abetalipprotenimea.
- Leukodystrophy: metachromatic.
- Mitochondrial encephalomyopathy.
- Wilson disease.
- Sialidosis.
- Other:hexosaminidase deficiency ,sphingomylein storage disease, ceroid lipofuscinosis,cholstrenolosis.
- Non-inherited ataxia cause:
- Brain surgery.
- Head injury.
- Alcohol abuse.
- Drug abuse.
- Infections, such as chicken pox (usually goes away after infection has cleared).
- Brain tumor.
- Exposure to toxic chemicals.
- Multiple sclerosis, cerebral palsy, and some other neurological conditions.
- Malformation of the cerebellum while the baby is still in the womb.
- Defect DNA repair:
- ataxia telangiectasia.
- Xeroderma pigmentosa.
- Cockayne syndrome.
Signs and Symptoms of Ataxia:
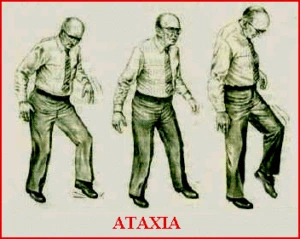
- Initial ataxia symptoms usually include:
- Poor limb coordination.
- Dysarthria – slurred and slow speech that is difficult to produce. The patient may also have difficulties controlling volume, rhythm, and pitch.
- If the ataxia progresses, other symptoms may also appear:
- Swallowing difficulties, may sometimes result in choking or coughing.
- Facial expressions become less apparent.
- Tremors – parts of the body may shake or tremble unintentionally.
- Nystagmus – involuntary, rapid, rhythmic, repetitive eye movement. Movements may be vertical, horizontal, or circular.
- Cold feet – because of a lack of muscle activity.
- Problems with balance.
- Walking difficulties – in severe cases, the patient may need a wheelchair.
- Vision problems.
- Hearing problems.
- Depression – as a result of having to live and cope with the symptoms.
Types of Ataxia:
(1) Cerebellar ataxia:
(2) Sensory ataxia:
(3) Vestibular ataxia:
(4) Frontal ataxia:
(5) Mixed ataxia:
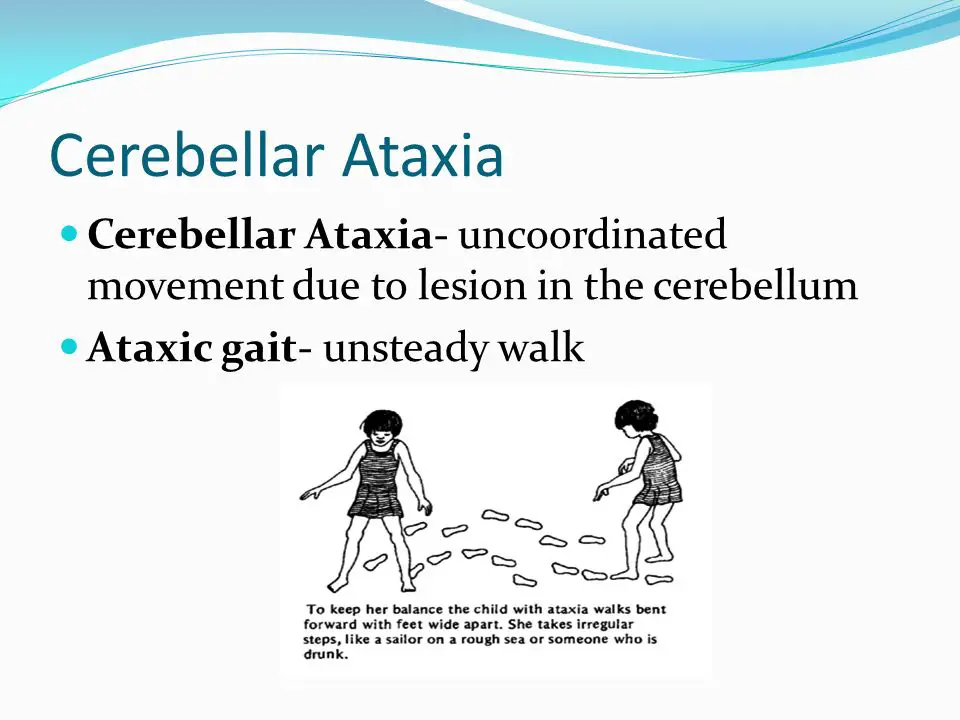
(1) Cerebellar ataxia:
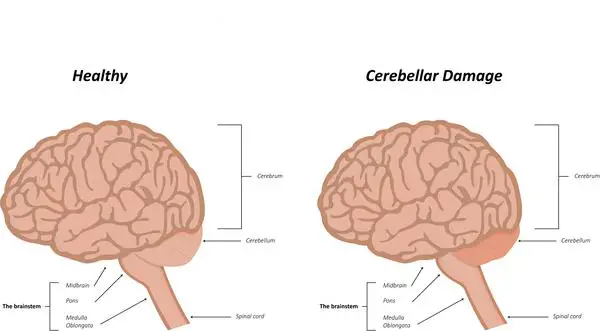
- Cerebellar ataxia develops as a result of lesions to the cerebellum, and/or the afferent and efferent connections of the cerebellum.
- This is ataxia caused by a dysfunction of the cerebellum – a region of the brain involved in the assimilation of sensory perception, coordination, and motor control.
- Early onset cerebellar ataxia usually emerges between the ages of 4 and 26. Late onset ataxia generally appears after the patient is 20. Late-onset ataxias usually present less severe symptoms, compared with early-onset ataxia.
- Head posture: Upright and sometimes fixed.
- Trunk posture: Stooped leans forward.
- Stance: wide-based.
- Initiation of gait: Normal.
- Postural reflexes: +ve/-Ve
- Steps: Stagger-lurching.
- Stride length: Irregular.
- Leg movement: Variable, ataxic.
- Speed of movement: Normal-slow.
- Arm swing: Normal, exaggerated.
- Turning corners: Veers away.
- Heel-toe test: Unable.
- Romberg’s test: +ve/-ve
- Heel-shin test: Usually abnormal.
- Falls: Uncommon.
- Symptoms associated with cerebellar ataxia:
- Dysmetria: This refers to inaccuracy in achieving a final end position (hypermetria equals overshoot; hypometria equals undershoot). This clearly is demonstrated by the patient attempting the finger-nose test.
- Tremor: Kinetic tremor, which is an oscillation that occurs during the course of the movement.
- Intention tremor, which is the increase in tremor towards the end of the movement.
- Postural tremor, which occurs when holding a limb in a given position.
- Titubation, which is a tremor affecting the head and upper trunk typically after a lesion of the vermis.
- Postural truncal tremor, which affects the legs and lower trunk, is seen in anterior cerebellar lobe lesions
- Dyssynergia: is distinct particularly during multi-joint movements. This may have several reasons: agonist-antagonist and synergistic muscles may not be able to contract in correct order during voluntary movement; or antagonist muscle may be failing to control eccentric contraction during the concentric contraction of agonist muscle.
- With the combination of these two factors, the extremity undergoes a sudden velocity resulting in inappropriate and uncontrolled motor movement.
- Dysdiadockokinesia: This is the inability to perform rapidly alternating movements such as alternately tapping with palm up and palm down. The rhythm is poor and force of each tap is variable.
- Hypotonia: This occurs in acute cerebellar lesions, but it is rarely seen in chronic lesions. Hypotonia is distinct particularly in proximal and antigravity muscles.
- Weakness and fatigue: This describes a generalized non-specific weakness as a feature of cerebellar dysfunction. This occurs more often with extensive and deep lesions and is most apparent in the proximal musculature. Fatigue has also been noted as a common feature of cerebellar dysfunction.
- Dysarthria: This occurs due to in-coordination between tongue and lip muscles. The patient speaks like he is drunk.
- Nystagmus: abnormal eye movements that develop in horizontal and vertical directions mostly as nystagmus at the end point (Edwards 1996).
- Deep tendon reflexes are maintained in cerebellar lesions, and gain a pendular characteristic.
- Cerebellar ataxia can be observed in diseases such as spino-cerebellar ataxia among hereditary ataxias, Friedreich’s ataxia, chronic alcoholism, paraneoplastic cerebellar degeneration, pontocerebellar angle tumors, and multiple sclerosis.
- Ataxia telangiectasia:
- ATM gene involved in detecting DNA damage, plays a role in cell cycle progression.
- Small veins appear around the corner of the eyes, cheeks, and ears.
- Physical and sexual development is usually delayed.
- Neurologic effects:
- Progressive cerebellar ataxia (earliest feature; children usually begin walking, then have problems with fluid walking); articulation problems.
- abnormal eye movements – oculomotor apraxia is earliest.
- Can also have dystonia, chorea, and peripheral axonal neuropathy.
- Oculocutaneous telangectasias:
- Oculobulbar, nose, face, ear, neck. Appear age 3-5 yo. Also can have cafe-au-lait macules.
- Immune deficiency: Recurrent sinopulmonary infections.
- Pulmonary disease: Major cause of death – recurrent infections, interstitial lung disease, neuromuscular abnormalities (dysphagia, aspiration, resp muscle weakness).
- Malignancy: 10-20% will develop cancer.
- Friedreich’s ataxia:
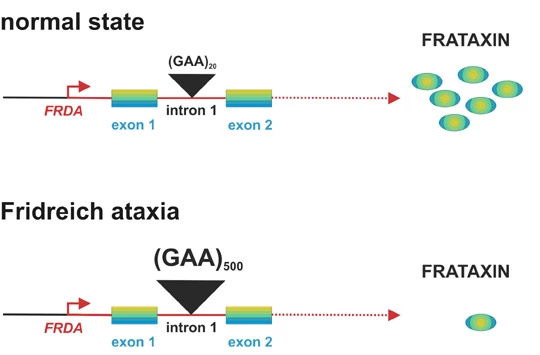
- Most common hereditary ataxia – 1:50,000 Caucasian
- Frataxin gene – 9q13 – trinculeotide repeat
- Affects the brain, heart, and pancreas. The slow onset and progressive.
- Onset before age 25 (often by age 5), ataxia of all 4 limbs, cerebellar dysarthria, absence of LE reflexes, pyramidal signs (weakness, extensor plantars), optic atrophy, brainstem involvement (swallowing dysfunction), early loss of position/vibration without pain/temperature loss, sensineuronal hearing loss
- Cardiomyopathy: 66% of patients – hypertrophic – main cause of death is arrhythmia and heart failure
- Diabetes Mellitus: 33% of patients.
- The spine curves sideways (scoliosis).
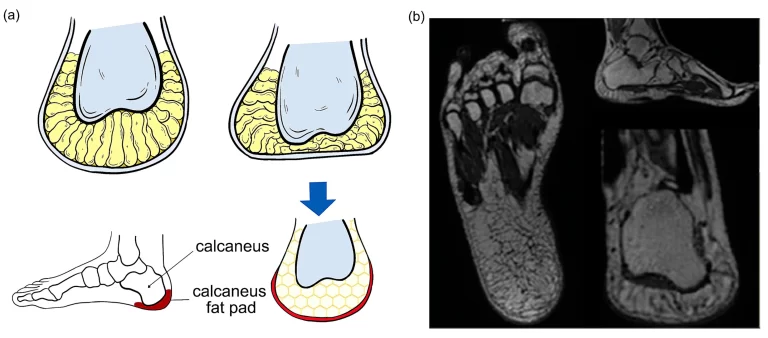
- Pes cavus (high arching feet).
- For patients whose ataxia is caused by injury or illness, symptoms often improve over time and eventually go away completely.
- Causes of cerebellar ataxia:
- Floppiness (hypotonia).
- Lack of coordination between organs, muscles, limbs, or joints (asynergy).
- Impaired ability to control distance, power, and speed of an arm, hand, leg, or eye movement (dysmetria).
- Difficulty in accurately estimating how much time has passed (dyschronometria).
- An inability to perform rapid, alternating movements (dysdiadochokinesia).
- The extent of symptoms depends on which parts of the cerebellum are damaged, and whether lesions occur on one side (unilateral) or both sides (bilateral).
- If the vestibulocerebellum is affected, the patient’s balance and eye movement control will be affected. The patient will typically stand with feet wide apart in order to gain better balance and avoid swaying backward and forward (posterior-anterior oscillations).
- Even when the patient’s eyes are open, balance may be difficult with feet together. If the spinocerebellum is affected, the patient will have an unusual gait with unequal steps, sideways steps, and stuttering starts and stops. The spinocerebellum regulates body and limb movements.
- If the cerebrocerebellum is affected, the patient will have problems with voluntary, planned movements. The head, eyes, limbs, and torso may tremble as voluntary moves are carried out. Speech may be slurred, with variations in rhythm and loudness.
- Clinical assessment, measurement, and evaluation:
- Finger-to-finger & finger-to-nose.
- Heel-to-shin test.
- Rebound test.
- Rapid alternating movement.
- Romberg test for postural sway.
- Tests of motor performance:
- Gait: Timed walking test, cadence & stride length measures.
- Balance: FRT, Standing balance, TUG.
- Spiral test
- Nail test.
- Causes of motor impairment:
- Individual’s voluntary restriction of activity as an adaptation to motor control deficit.
- Motor control.
(2) Sensory ataxia:

- This is ataxia due to loss of proprioception. Proprioception is the sense of the relative position of neighboring parts of the body. It is a sense that indicates whether the body is moving with the required effort and gives feedback on the position of body parts relative to each other.
- A patient with sensory ataxia typically has an unsteady stomping gait, with the heel striking hard as it touches the ground with each step. Postural instability becomes worse in poorly lit environments. If a doctor asks the patient to stand with eyes closed and feet together, their instability will worsen. This is because loss of proprioception makes the patient much more reliant on visual data.
- The patient may find it hard to perform smoothly coordinated voluntary movements with the limbs, trunk, pharynx, larynx, and eyes.
- Head posture: Leans forward.
- Trunk posture: Stooped-upright.
- Stance: Wide-based.
- Initiation of gait: Normal wariness.
- Postural reflexes: Intact.
- Steps: High-stepping.
- Stride length: Regular.
- Leg movement: Variable-hesitant and slow.
- Speed of movement: Normal-slow.
- Arm swing: Normal.
- Turning corners: Minimal effect.
- Heel-toe test: +ve/-ve.
- Romberg’s test: Increased unsteadiness.
- Heel-shin test: +ve/ve.
- Falls: yes.
(3)Vestibular ataxia:

- The vestibular system is affected. In acute (sudden) unilateral cases, the patient may experience vertigo, nausea, and vomiting. In slow-onset chronic bilateral cases, the patient may only experience unsteadiness.
- Head posture: Upright and definitely fixed.
- Trunk posture: Upright.
- Stance: Wide based.
- Initiation of gait: Normal.
- Postural reflexes: +ve/-ve.
- Steps: Normal.
- Stride length: Normal.
- Leg movement: Normal.
- Speed of movement: Normal-slow.
- Arm swing: Normal.
- Turning corners: Dysequilibrium.
- Heel-toe test: Unable.
- Romberg’s test: -ve.
- Heel-shin test: Normal.
- Falls: Common.
(4)Frontal ataxia:
- Frontal ataxia (also known as gait apraxia) is observed when tumors, abscesses, cerebrovascular accidents, and normal pressure hydrocephalus affect the frontal area. It has the below-listed features:
- A patient has difficulties standing erect.
- Even with the use of support, the patient tends to lean towards hyperextension
- The patient’s legs are in a scissors-cross position during walking and there is incoordination between the legs and trunk
- Ataxia is accompanied by frontal dementia, urinary incontinence, frontal release signs, and perseveration (jeffmann.net/NeuroGuidemaps/gait).
- Head posture: Leans forward.
- Trunk posture: Upright.
- Stance: Wide-based.
- Initiation of gait: Start hesitation.
- Postural reflexes: May be absent.
- Steps: Small-shuffling.
- Stride length: Short.
- Leg movement: Stiff, rigid.
- Speed of movement: Very slow.
- Arm swing: Exaggerated.
- Turning corners: Freezing-shuffling.
- Heel-toe test: Unable.
- Romberg’s test: +ve/-ve.
- Heel-shin test: Normal.
- Falls: Very common.
(5)Mixed ataxia:
- Mixed ataxia refers to the type of ataxia when symptoms of two or more types of ataxia are observed together, such as occurrence of sensory and cerebellar ataxia symptoms. In some diseases, mixed ataxia may be observed frequently.
- For instance, in Multiple Sclerosis, cerebellar, vestibular, and sensory ataxia may be observed together; whereas in cases of spino-cerebellar ataxias, cerebellar and sensory ataxia may be seen.
Diagnosis of Ataxia:
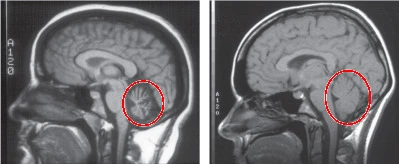
- MRI or CT scan: To determine whether there is any brain damage.
- Genetic tests: To determine whether the patient has inherited ataxia.
- Blood tests: Some types of ataxia affect the make-up of blood.
- Urine tests: Urinalysis may suggest specific systemic abnormalities that are linked to some forms of ataxia. If the specialist suspects Wilson’s disease, the patient may be asked for a 24-hour urine collection to determine how much copper is in the system.
Physiotherapy Treatment and Rehabilitation of Ataxia:
- The goal of the physiotherapist in the rehabilitation of ataxia resulting from defects in neurological structures and affecting the functions of the patient is to improve the functional level of the patient through restorative techniques. When this is not possible, the therapist makes use of compensatory strategies to make the patient perform as independently as possible within the present functional level. The goals of restorative physical treatment can be briefly described as:
- Improving balance and postural reactions against external stimuli and gravitational changes.
- Improving and increasing postural stabilization following the development of joint stabilization.
- Developing upper extremity functions.
- Through developing an independent and functional gait, improving the life quality of the patient by increasing the patient’s independence while performing daily life activities.
- Main principles of training:
- Throughout the whole training program, exercises should be practiced consciously at first, and in later stages should be followed by automatic exercise activities.
- Exercises should progress from simple to complex.
- Activities should be practiced first with the eyes open and later with the eyes closed.
- After achieving proximal tonus and stabilization, the coordinated movement of the distal segments should be taken into consideration.
- Compensation methods and supportive aids and equipment should be employed when necessary.
- Treatment should be supported by an appropriate home exercise program and sports activities.
- Measurement and assessment:
- In the treatment of ataxia, it is essential to determine treatment programs suitable for the patient and his/her needs in order to attain the desired goal of the physiotherapy and rehabilitation program.
- This can be achieved through the use of appropriate measurement and assessment methods, and the interpretation of the findings.
- Measurement and assessment are not only in terms of preparing a suitable treatment program but also in the follow-up of the changes in the patient’s condition over a period of time and the observation of the effects of the treatment.
- Standardization problems in measurement and assessment which are one of the most distressing aspects of neurological rehabilitation applications become more troubling in cases of ataxia.
- In the literature, there are more scales, observational methods, and computerized systems developed to assess balance than to evaluate in-coordination.
- Although the observational methods and scales mostly designed to assess balance are easy to use and can be readily utilized in the clinic, their ability to provide standardized measurements is limited, and the results can vary depending on the person who has done the observation.
- Though computerized systems are highly reliable, they are costly systems that require working within the laboratory environment. Balance assessment tools are frequently used by physiotherapists.
- Methods of balance assessment:
- External Perturbation Test – Push and Release test: Purpose of static balance.
- External Perturbation Test – Pull test: Purpose of static balance in different sensory conditions.
- Clinical Sensory Integration Test: Purpose of Dynamic balance in different sensory conditions.
- Sensory Integration Test of Computerized Dynamic Posturography: Purpose of static and dynamic balance.
- Static and Dynamic Posturography: Purpose of Static balance.
- Single Leg Stance Test: Purpose of static balance.
- Functional Reach Test: Purpose of functional static and dynamic balance.
- Berg Balance Scale: Purpose of functional static and dynamic balance.
- Five Times Sit to Stand Test: Purpose of functional dynamic balance and gait.
- Time Up and Go Test: Purpose of Gait and Functional Dynamic Balance.
- Dynamic Gait Index: Purpose of dynamic balance and gait.
- Tandem Walking: Purpose of dynamic balance.
- Four Square Step Test: Purpose of dynamic balance.
- Measurements such as gait duration, step length, and step width can be used apart from these tests. Moreover, self-perception scales filled in by the patient such as the Dizziness Handicap Inventory, Activity Specific Balance Confident Scale, and scales for daily living activities such as FIM™ and Barthel Index can be employed to assist in assessment methods.
- There are a limited number of scales that have been developed to assess truncal ataxia and extremity ataxia together, and tested for validity and reliability.
- Scales of ataxia:
- International Cooperative Ataxia Rating Scale: Evaluating truncal and extremity ataxia, gait ataxia, nystagmus, and talking.
- Scale for Assessment and Rating of Ataxia: Evaluating truncal and extremity ataxia, gait ataxia, and talking.
- Ataxia Functional Composite Scale: Evaluating gait speed, upper extremity ataxia, and visual acuity.
- Nine Hole Peg Test: Evaluating upper extremity ataxia.
- Computer Graphics Tablet: Evaluating upper extremity ataxia.
- Brief Ataxia Rating Scale: Evaluating truncal and extremity ataxia, gait ataxia, nystagmus, and talking.
- Friedreich’s ataxia impact scale: Speech, upper limb functioning, lower limb functioning, body movement, complex tasks, isolation, mood, self-perceptions.
- Composite cerebellar functional severity score: Upper limb functions.

- Physiotherapy approaches:
- A physical treatment program is prepared from the interpretation of the measurement and assessment results.
- The contents of the treatment program can vary depending on the type and characteristics of ataxia.
- For instance, while approaches that improve proprioception and incorporate visual aids are used more commonly in patients with sensory ataxia, stabilization training is more important to reduce truncal and extremity ataxia in patients with cerebellar ataxia.
- The patient with vestibular ataxia should be given habitation exercises in order to reduce vertigo, and vestibulo-ocular, and vestibulo-spinal reflexes should be stimulated to improve balance.
- In some cases, a problematic condition that requires the use of a number of approaches, such as mixed ataxia, may arise.
- In such cases, the experience of the physiotherapist and the patient’s effort play an important role in determining the program.
- When preparing the treatment prescription, it should be kept in mind that the proprioceptive, vestibular, and visual systems, and the cerebellum are in close relation, and that balance and coordination result from this relation.
- For example, proprioceptive exercises contribute to balance while improving proprioception. The opposite of this is also true. Approaches in the treatment of extremity ataxia may enable proprioceptive input to increase and the balance to develop by establishing stabilization.
- Therefore, it is not possible to classify the methods used in the rehabilitation of ataxia as approaches directed merely towards proprioception or balance, since all of these interact with each other.
- The classification of treatment applications can be briefly described as follows:
- Approaches for improving proprioception:
- The aim is to increase proprioceptive input by mechanically stimulating the joint surfaces, muscles and tendons, and decreasing postural instability by improving body awareness.
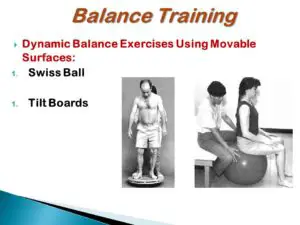
- There are many approaches that can be used for this purpose. These are: Proprioceptive Neuromuscular Fascilitation (PNF), rhythmic stabilization, slow reversal techniques, resistive exercises, use of Johnstone pressure splints, gait exercises on different surfaces (hard, soft, inclined surfaces) with eyes open and closed, plyometric exercises, balance board-ball and minitrampoline exercises.
- Recently, vibration has been a frequently used application. Vibration can directly be applied to the muscle and tendon, and also is applied by exposing the whole body to vibration.
- Another method is the suit therapy. The suit is made up of a vest, shorts, knee pads and special shoes attached by using bungee type bands that are used to correctly align the body and provide resistance as movements are performed.
- Its major goals are to improve proprioception (sensation from joints, fibers, and muscles), and to increase weight-bearing for normalized sensory input regarding posture and movement.
- In addition, methods which develop body awareness, such as the Feldenkrais and Alexandre Techniques, yoga, and body awareness exercises can be included in the program.
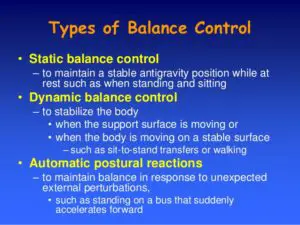
- Activities for improving balance:
- Firstly, the proximal muscles and stabilization of the trunk should be improved. For this purpose, it is appropriate to use the mat activities of the PNF techniques.
- Following the neuro-developmental order, the patient should be trained to come to the bridge position from lying on the back, onto the forearms from lying face down, to crawl, and to come onto the knees, half knees, and into a sitting position, and to establish static and dynamic stability in these positions.
- Initially, the patient should be maintained in the required position by approximation and verbal directions, and then static stabilization should be strengthened through external perturbation (pushing and pulling in different directions).
- Afterward, the patient should be trained in these positions for weight transferring and functional extension so as to be prepared for dynamic stabilization.
- Subsequently, the patient should be trained in positions in which the support surface is narrowed or the center of gravity is changed in order to make the balance activities difficult. (e.g. establishing balance on two or three extremities in the crawling position or shifting the center of gravity upwards by the elevation of the arms in the sitting-on-the-knees position).
- In the standing position, following the transferring of weight onto the front, back, and sides, narrowing the support surface, and balance training in tandem position, balance training on one leg should be performed. This is a position with which ataxic patients have great difficulty.
- Another option is to perform balance training on the posturography device in order to benefit from visual feedback obtained from observing the patient’s ability to sustain his/her postural oscillation in the center of gravity.
- The best indicator of dynamic stabilization/balance is gait. Therefore, gait training should be given including the following applications: walking on two narrow lines, tandem gait, backward gait, slowed down gait (soldier’s gait), stopping and turning in response to sudden directions, flexion, extension, and left-right rotations of the head.
- Disciplines such as Tai Chi and Yoga consist of activities that develop balance.
- Vestibular exercises:

- Since dizziness accompanies balance dysfunction in vestibular problems, repetitive head movements and Cawthorne and Cooksey exercises are of great importance.
- A vestibular exercise program consists of repetitive, progressively more difficult, eye, head and body movements designed to encourage movement and facilitate sensory substitution. Many components of this exercise program are used by physical and occupational therapists today.
- Approaches to extremity ataxia:
- Exercises designed for the treatment of extremity ataxia are utilized to provide fixation by establishing a balance between the eccentric and concentric contractions within the multi-joint movements of the lower extremities and the upper extremities in particular.
- During the performance of these exercises, it is important to establish slow, controlled, and reciprocal multi-joint movement and stabilization. Freenkel’s coordination exercises were developed for this purpose. Actively repeated contractions similar to PNF can be utilized on their own or by combining them with Freenkel’s coordination exercises.
- While these two types of exercise are effective in cases with mild extremity ataxia, they can be insufficient in severe cases. In such cases, rhythmic stabilization and a combination of isotonic techniques are more effective than PNF.
- Coordination Dynamics Therapy (CDT) was developed by Dr. Giselher Schalow. This therapy, he says, “improves the self-organization of the neuronal networks of the CNS for functional repair by exercising extremely exact coordinated arm and leg movements on a special device (GIGER MD) and, in turn, the coordinated firing of the many billions of neurons of the human CNS”.
- Use of supportive aids:
- In cases in which restorative physical treatment applications are insufficient, the use of supportive devices enables the patient to function more easily within his present functional level. In cases of severe ataxia, suspending weights from the extremities and the use of weighted walkers can be preferred.
- Sports activities:
- Horse riding, swimming, playing billiards, golf, and darts are suitable for this type of patient.
- Counseling:
- Patients with ataxia commonly become frustrated and depressed; this usually results from having to cope with some symptoms that affect physical mobility and coordination. Talking to a well-qualified counselor, such as a psychotherapist, can help.
- Supplements and nutrition:
- Some patients with ataxia have very low levels of vitamin E and require supplements and/or a special diet. As sensitivity to gluten may occur among some patients with ataxia, a gluten-free diet may help.
- Medication:
- Some patients with ataxia telangiectasia are prescribed gamma-globulin injections to boost their immune systems. There are also drugs for muscle spasms and uncontrollable eye movements.




my uncle suffering from cerebellar Syndrome and i have searched related detail and i see this article about ataxia , very good detail of cerebellar syndrome, she is doing physiotherapy treatment regularly and get good balance and co-ordination
Very helpful article.. Thanks…
Hi,
I have 2 boys with mixed cerebellar hypoplasia and I have never read a post better than this. I would really like to get in contact with you and discuss some approaches for their therapy.