Heel Fat Pad Syndrome (HFPD)
Introduction
Heel fat pad syndrome is a condition that causes pain and discomfort in the heel. It is caused by the breakdown or loss of the fat pad that cushions the heel bone. This can happen due to a number of factors, including aging, repetitive stress, and injury.
The disorder also occurs due to alterations in the thickness and/or elasticity of the heel fat pad. Fat pad syndrome is a disorder that often affects the middle of your heel and typically comes on by the fat pad’s loss and degeneration.
The loss of the thick, insulating pad on the heel region of your feet’s soles is known as “heel fat pad syndrome.” Due to wear and tear, recurrent activities that put a lot of stress on your heel pad, a heavier body weight, an uneven distribution of your weight as you walk, and other causes, this heel pad loses its density and elasticity.
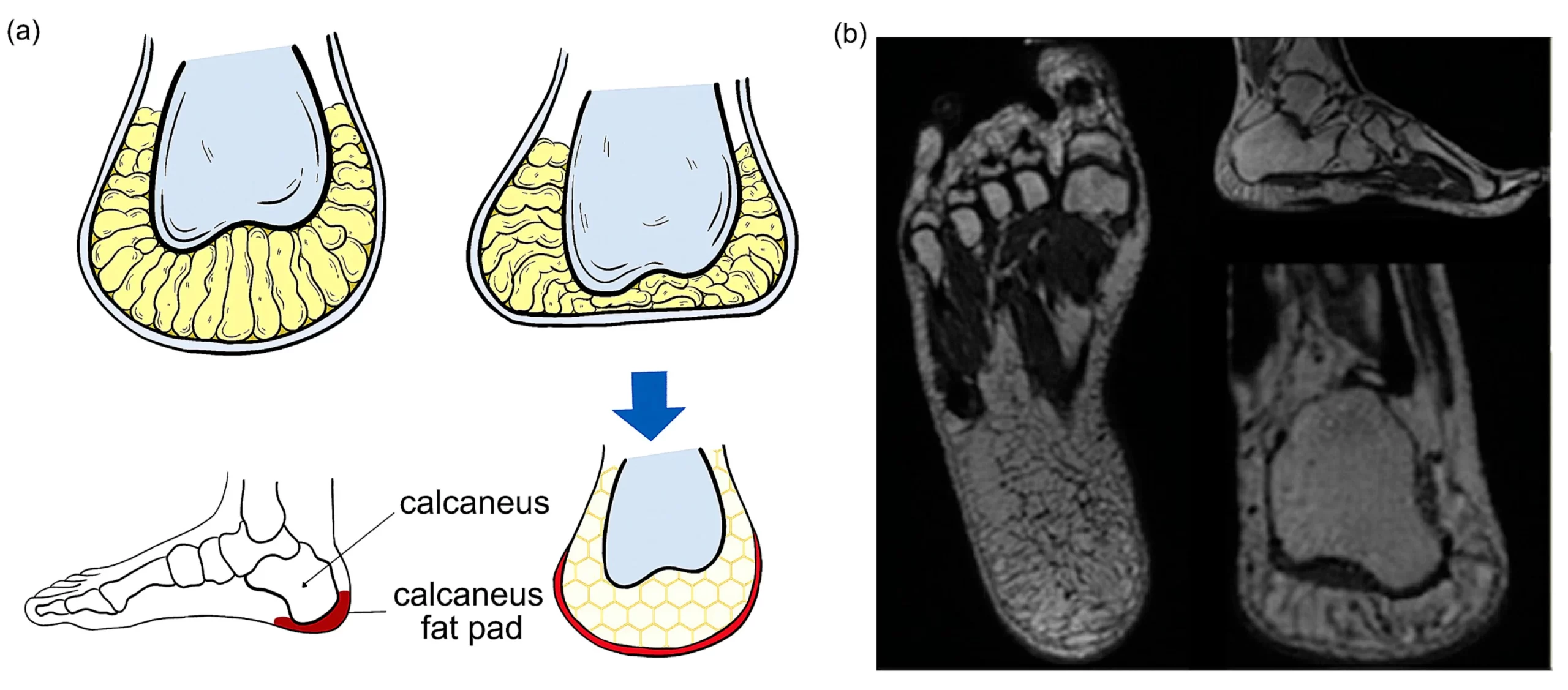
The soft tissue layer between the skin and the heel bone is known as the plantar fat pad. Its honeycomb structure and fibro-elastic chambers filled with fat globules serve to absorb shock and distribute pressure evenly throughout the surface of your heel when you’re moving about. Less shock absorption will increase the heel bone’s susceptibility to recurrent microtrauma. As a result, the heel bone may experience persistent inflammation, bruising, swelling, and pain.
The bursa, which is located beneath the fat pad, may become irritated or inflamed as a result of the increased strain. A bursa is a little sac filled with fluid that lies between the heel bone and soft tissue. The bursa aids in friction reduction and shock absorption.
Anatomy
The calcaneum and proximal plantar fascia, which are covered by the heel fat pad, are specialized adipose structures that are encompassed by ligamentous chambers and act as a cushion against heel strike during movement. Additionally, it acts as a mechanical anchor to distribute body weight properly without placing undue strain on the underlying tissues.
When walking and running, the heel may support 110 and 200 percent of the body’s weight, respectively. Excessive mileage and a sustained rise in pressure striking and load forces may cause the fat pad in the heel to swell, which is a typical cause of heel pain.
Causes of Heel Fat Pad Syndrome (HFPD)
Heel pain that can affect our everyday lives and interfere with our regular activities is frequently brought on by the fatty tissues and muscle fibers that make up the heel pads wearing out over time. Heel pads that have been subjected to excessive wear and strain may shrink or become less elastic. The degradation of the heel pad’s fibrous membrane as well as the loss of moisture and soft tissue flexibility that results from fat pad atrophy restrict the body’s ability to absorb shocks.
It is also termed Fat Pad Atrophy (FPA). After plantar fasciitis, it is regarded as the second most common cause (14.8%) of plantar heel discomfort. Both conditions can cause heel pain, but there are differences in the risk factors, symptoms, and treatments between them. It is frequently mistaken as plantar fasciitis.
It can happen as a result of corpus adiposum strain, atrophy, injury, or misuse. The two main contributing elements to heel fat pad syndrome are the alignment of the foot’s arch and the gait or biomechanics. The foot’s arch serves as a support for the foot’s normal upright alignment. The heel pad is subjected to increased pressure if the arch is damaged or impaired.
After plantar fasciitis, heel fat pad decrease is considered as the main source of plantar heel discomfort. Overweight(from 30+ years old) thinning of the fat pad naturally
wearing the wrong, non-supportive shoes
spending a lot of time walking or standing still, particularly when these activities suddenly increase.
Diabetes
Rheumatoid arthritis, psoriatic arthritis, and other inflammatory diseases.
A weakness in your leg and foot muscles
The muscles in the backs of your legs are tense
not giving enough time for rest between activities
Continual intake of oral corticosteroids
Corpus adiposum inflammation: The fat pad may become inflamed if it is repeatedly or for an extended period of time subjected to force or pressure. Patients who participate in sports like basketball, volleyball, gymnastics, or athletics that demand a lot of jumping frequently experience this. A few people experience displacement or thinning of the corpus adiposum, the fat pad located in the heel. Since the normal aging process causes a decline in the flexibility of the body’s soft tissue structures, this is common among elderly patients. Walking or sprinting barefoot, especially on hard surfaces like concrete or tiles, exerts excessive force on the fat pad, causing the corpus adiposum to shrink and become strained as well as bruising the calcaneus.
Gait imbalance: People who have feet that point inwards or outwards may get heel pad pain because their heels don’t touch the ground as well when they run or walk. In the regions where the heel is making forceful contact with the ground, the corpus adiposum frequently thins down, wears out, or gets inflamed.
Overweight and obesity: Since their excess body weight places greater pressure on their feet, patients who are overweight or obese are more likely to experience heel pad pain. There are a select few medical diseases that are thought to contribute to the atrophy of the heel fat pad, despite the fact that they are less frequent. Lupus, rheumatoid arthritis, and type 2 diabetes are among the illnesses where it is frequently observed.
Plantar fasciitis: In those with plantar fasciitis, the corpus adiposum can thin out significantly faster than it otherwise would. When the plantar fascia is injured or inflamed, it is less able to evenly distribute the forces generated by walking or running. This causes the heel fat pad to be under more strain and wears it down more quickly.
Symptoms of Heel Fat Pad Syndrome (HFPD)
Heel pad syndrome presents with symptoms that are very similar to those of plantar fasciopathy. The fat pad condition, however, is a little different. The soreness is less severe during the first few steps in the morning and during rest intervals; nevertheless, the discomfort becomes more severe when weight-bearing activity increases.
- a dull ache that has been developing under the heel’s core gradually
- When standing or walking for extended periods, pain gets worse with exercise.
- Localized edema that might be uncomfortable when wearing shoes
- When pressed directly, it hurts more and can feel warm or tender.
Walking, standing, or running causes a sharp, bruise-like pain in the middle of your heel.
Deep discomfort that is reproducible by applying pressure to the middle of your heel.
Pain that worsens when standing or moving for extended periods of time, while engaging in high-impact exercises or sports (such as basketball, gymnastics, jogging, or jumping), or when going barefoot and walking on hard surfaces (such as concrete, hardwood floors, or ceramic tiles).
If you walk barefoot or on a hard surface, run, or press your fingers into the middle of your heel, you may only sometimes experience pain in mild cases.
Patients with heel pad syndrome typically experience deep, bruise-like pain in the middle of the heel when they walk, run, or stay still for an extended period of time.
Firm palpation allows for its replication.
Prolonged walking or standing makes this pain worse, especially if you’re barefoot, walking on hard surfaces, or engaging in any high-impact activities.
When aggravated by direct pressure or coming into touch with hard surfaces like hardwood floors, concrete, or ceramic tiles, mild cases of heel pad syndrome may be asymptomatic or only occasionally felt.
ache during sleeping and at night.
Usually, only one side of the heel—one heel, not both—is painful.
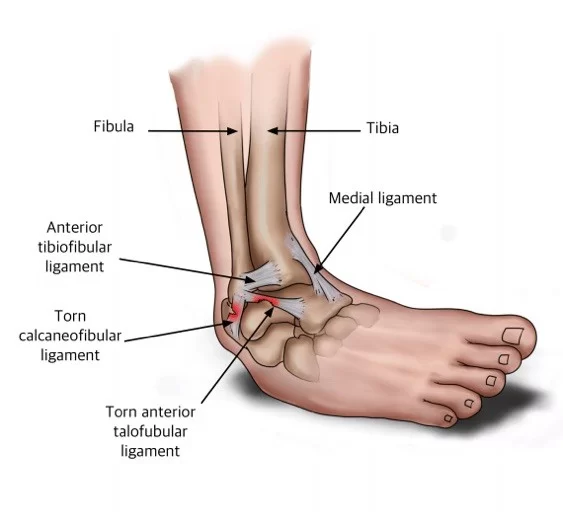
While the two conditions have a similar presentation, Plantar Fasciitis causes pain to be felt in the anteromedial portion of the calcaneus, whereas Heel Fat Pad Syndrome causes pain to be felt in the middle of the heel.
Diagnosis
Based on the symptoms and physical examination, heel pad syndrome can be identified. To identify fat pad atrophy or rule out other potential causes of heel discomfort, a foot X-ray or ultrasound investigation can be carried out. In imaging studies, the heel pad’s thickness is measured. The typical heel pad thickness is 1-2 cm. A fat pad is deemed atrophied if it is less than 1 cm thick. A therapist may compare the heel pad thickness in weight-bearing and non-weight-bearing positions to determine the elasticity.
healthcare provider will ask about your medical history and your present symptoms.
healthcare professional will enquire into your heel discomfort in detail, including:
What kind of discomfort is it?
When did the pain start?
What causes the discomfort?
When did you initially notice the discomfort?
Does resting make the discomfort go away?
healthcare professionals will examine your foot physically to check for structural issues and will apply pressure to the heel’s center in an effort to simulate your pain. Additionally, your healthcare professional will assess the difference in heel pad thickness between when you are standing on one foot and when you are not. The typical heel pad thickness ranges from 0.4 to 0.8 inches or 1 to 2 centimeters. A hard, rigid heel pad could indicate that your heel loses much elasticity.
The diagnosis of heel fat pad syndrome or to rule out other potential reasons for your heel pain may occasionally be assisted by magnetic resonance imaging (MRI).
Treatment of Heel Fat Pad Syndrome (HFPD)
You can move more comfortably and experience fewer symptoms by using pain medication, which will hasten your recovery. Your local chemist can offer advice on particular medications or alternative pain treatment techniques (always read the label and manufacturer’s instructions).
take medicine. Utilize over-the-counter medications to lessen discomfort and inflammation. Naproxen and Ibuprofen are two examples.
Activity Modification: A break from rigorous athletic training, such as long-distance running, should be considered etc.
Mobilization: Mobilization and glides of portions of the foot and ankle, including the plantar fascia, rear foot, and ankle joint directed at increasing motion and restoring normal function.
Custom insoles and taping: Taping techniques try to put the pad under the calcaneus in an ergonomically right position while shoe inserts provide padding in problematic areas. Heel cups, cushioned socks with additional padding, and custom-fit shoes may support the feet and lessen pressure on the heels.
Rest: As much as possible, avoid being on your feet and reduce high-impact activities that can aggravate heel discomfort.
Apply ice: Apply an ice pack to your heel for 20-minute intervals after activities that cause heel pain.
Wear orthopedic footwear: See your podiatrist or visit a shoe store specializing in orthopedic footwear to be fitted with shoes that provide extra heel support.
you tap your heel. Tape your heel so that it shifts and is properly repositioned beneath your heel bone to offer support and the necessary cushioning. You’ll learn how to correctly tape your foot from your doctor.
Utilize heel cups, shoe inserts, and cushioned socks: These items, which are readily accessible online or at your neighborhood pharmacy, offer additional heel cushioning and support.
Exercise plan: With the help of your doctor or a physical therapist, you’ll learn the right stretches to lengthen your calves as well as rehabilitation exercises to address any imbalances or incorrect foot-knee-hip alignment.
Home Exercise Programs (HEP)
Self-stretching and mobilization strategies are included in patient education along with the avoidance of activities that aggravate symptoms (such as high-impact exercises). While mobilizations should include ankle eversion and plantar fascia motions, stretching must focus on lengthening the gastrocnemius and soleus. Improve foot, ankle, and lower leg muscle control: Start with exercises for foot stabilization and weight-bearing calf muscle strengthening. Address any weaknesses that could be related to a change in foot biomechanics.
Address biomechanics foot position and increase neuromuscular control: For assistance in correcting the lower limb, look for muscular imbalances at the hip and knee. increase your proprioception and balance to increase your dynamic control of your foot and ankle.
Increase load on tissue, adding sport-specific/dynamic exercise: To gradually return to full function, get the foot and lower leg ready for more explosive motions. Include plyometric exercise as well; pay attention to alignment and technique when moving; focus on jumping and landing.
Treatments include physiotherapy approaches and more advanced techniques. Reduced pain and inflammation, preservation and protection of the existing adipose tissue, and prevention of additional damage are the main objectives of physical therapy treatments. In more recent treatments, materials are added to the heel to thicken the heel pad.
Physiotherapy
Weight management
Weight gain will increase the strain on your heel and lessen your feet’s capacity to absorb shock. Even a slight weight loss might have a major effect.
Footwear
There will be some swelling and inflammation in the heel with fat pad syndrome. It is best to stay away from footwear with thin, rigid soles. Your foot won’t receive enough cushioning or stress absorption from these shoes. Some people find benefit in wearing a thicker-soled shoe, such as a trainer, that provides more shock absorption and cushioning because the heel’s capacity to absorb stress has decreased.
Injury Management
The first 24 to 48 hours following a moderate sprain, strain, or sports injury are outlined in the P.O.L.I.C.E standards.
For the first 24 to 48 hours following an injury, support or protect the injured body part. For support, wrap the wound in a thin bandage.
Optimal loading promotes early activity and recuperation. Moving the wounded part within a pain-free range to aid in optimal healing is the key to optimal loading.
A prolonged amount of rest may prolong your recovery time and have negative effects on your health and wellness.
If an injury or flare-up occurred within the previous two days, apply ice:
Wrap ice cubes in a wet towel.
Hold it against the sore area of your body for 20 minutes. Place a wet cloth between the ice and your skin to prevent ice burn.
Sports sprays and gel/cool packs are other options that work similarly. Every two to three hours, you can repeat this.
Heet pad: You could discover that heat is more calming after two days. A heating pad or hot water bottle with an insulated cover are both options. Check to make sure it isn’t too hot and isn’t in contact with your skin. Accomplish this for 10 to 15 minutes, three to four times a daytime.
Apply compression using a bandage or support like a tubi-grip until the swelling subsides. Start wrapping the bandage from the end that is farthest from your heart. If the pain worsens or the area starts to feel numb, loosen the bandage.
Avoid making the bandage overly tight and avoid sleeping in bed with a tubi-grip or other compression bandage.
During the first 24 to 48 hours, elevate your foot/ankle as far as you can above the level of your heart, especially when sitting or lying down. Use pillows underneath your foot to provide support.
After 48 hours:
Try to lift the additional weight; in this stage, loading with a limp is typically normal; and exercise can aid with pain relief.
-Continue to act as you normally would at work or go back to work.
-Delay engaging in strenuous activity until your mobility and discomfort are improved.
It is typical to still be in agony 48 hours afterward. It’s crucial to gradually start bearing weight on your hurting foot because too much rest could extend your healing time and have negative effects on your health and wellness.
Do not attempt to complete all of your regular daily tasks, such as housework, at once if you are in pain. Divide the more difficult tasks into smaller ones, and carry out a softer task in between.
Try to raise more weight; loading with a limp is usually normal at this point; and exercise can help with pain alleviation.
-Continue acting normally at work or report back to your position.
-Resist the urge to do anything physically demanding until your mobility and discomfort have improved.
48 hours later, it’s usual to still be in pain. It’s important to gradually resume weight-bearing on your injured foot because prolonged bed rest can delay healing and have a severe impact on your health and well-being.
If you are in pain, avoid attempting to finish all of your typical daily tasks—like housework—at once. Perform a simpler activity in between the more challenging activities, and then break them up into smaller ones.
Stretching exercises
Your foot and ankle flexibility can be increased with stretches for the rear of your legs. Your heel and foot will be able to absorb trauma more effectively as a result. Your podiatrist can provide you with advice on the exercises that are best for you.
Insoles
Investing in a pair of cushioning, shock-absorbing insoles or soft gel heel cups will frequently aid you in relieving your problems. These can be purchased online or in most pharmacies.
Strapping
The fat cushion above the heel bone can be kept in place by strapping or taping. Use this short-term remedy until your symptoms start to get better. You can get advice on this from your podiatrist.
Advanced Treatment:
Injectables. This technique thickens the fat pad by injecting a variety of synthetic or natural filler materials. Hyaluronic acid and poly-L-lactic acid are two components of dermal fillers. Due to its tendency to migrate to other body regions and may produce a mild-to-severe response, silicone is a contentious filler. Dermal fillers can last anywhere between six and twelve months, depending on your age, weight, lifestyle, and hobbies.
Using autologous fat transplants or fat grafting. This technique involves injecting a tiny quantity of fatty tissue into your heel from another part of your body (such as your thigh or abdomen). The outcomes of this outpatient surgery endure longer than those of dermal fillers.
Allografting. This method makes use of fat that has come from another individual. There is no risk of rejection because only fat cells are utilized. Compared to the other procedures, this one requires more recovery time (six to eight weeks for the new and existing tissues to heal together). Up to five years of pain alleviation may be possible with this medication.
Physical deformities in your toes, foot, ankle, leg, knee, or hip that alter your alignment and weight distribution, reduce your quality of life, or restrict your talents may be treated with surgery.
Complications
Untreated heel discomfort can be disruptive, making it challenging to walk, participate in sports, and work effectively. Heel pain can also change the way individuals walk, making them susceptible to falls and injuries.
Complications of untreated heel fat pad syndrome, If you leave heel fat pad syndrome untreated,
Continue to feel pain since it will make your life less enjoyable. Have difficulty walking or playing sports.
To reduce your pain, which might increase your risk of falls and incidents, change the way you walk.
Prevention
You can focus on some lifestyle practices to reduce your risk of getting heel fat pad syndrome even though wear and tear due to advancing age or a family history of this disease cannot be avoided. These consist of:
Always put on correctly padded, sole-supporting footwear. When engaged in high-impact activities, use athletic shoes. Avoid wearing high heels, especially those with sharp heels, as they can unevenly distribute your body weight, placing too much pressure on one part of your foot.
Reduce the amount of time you spend engaging in high-impact, weight-bearing sports (including running, basketball, and gymnastics) to allow your heel pad to recuperate afterward.
keep a healthy weight.
Avoid going barefoot, particularly on uneven and hard surfaces (such as cement, tile, and hardwood).
Check each of your shoes. If you see uneven wear on the soles or interior cushioning that is no longer supportive, change your shoes.
FAQs
Can heel fat pad syndrome be cured?
Heel fat pad syndrome has no surefire long-term solution. Your heel fat pad will shrink slightly as you age normally and experience normal wear and tear. However, you may improve the quality of your life and keep doing the things you enjoy by taking action to lessen heel pain and inflammation as well as stop additional injury.
How can I continue to function and complete the tasks I want and need to complete?
Do not attempt to complete all of your regular daily tasks, such as housework, at once if you are in pain. Divide the more difficult tasks into smaller ones, and carry out a softer task in between. If prolonged standing or walking makes your pain worse, avoid doing it. Modifying activities is advised rather than completely ceasing all sorts of exercise or movement. Running or walking can be substituted with non-weight-bearing exercises like swimming or cycling.
What can I do to reduce it on myself?
Prior to sending a recommendation to your neighborhood podiatry office, we would advise you to attempt some self-help treatments. Painkillers can help you feel less discomfort, move more easily, and speed up your recovery. Speaking with local pharmacists Pharmacists might offer advice on particular medications or other pain-relieving techniques.
What distinguished plantar fasciitis from heel fat pad syndrome?
The connective tissue (the fascia) that supports your foot’s arch weakens as a result of plantar fasciitis. Your plantar fascia runs from the heel to the tips of your toes. A sharp pain in your heel is the primary sign of plantar fasciitis. The discomfort may spread to the arch of your foot but is typically more intense closer to your instep or inner heel. When stretching, you experience tension in the sole of your foot. Additionally, the discomfort is worse when you first get up after a night of rest, gets better after use, but gets worse while you keep putting weight on your foot. If the plantar fascia is pressed on during an examination, the pain is characterized as being severe and stabbing.
The pain from heel fat pad syndrome is felt more in the heel’s middle. Long walks or periods of standing still can cause pain, as can high-impact sports and activities. Walking barefoot on hard surfaces might make the pain worse. In contrast to plantar fasciitis, the pain in your heel may occur more frequently at night and when you are at rest, and it is also more likely to affect both of your feet.
Both circumstances may exist simultaneously. Additionally, heel fat pad syndrome can result from plantar fasciitis. This occurs because a damaged plantar fascia makes it more difficult to distribute your body weight while jogging or walking evenly. This causes your heel fat pad to experience more pressure and wear more quickly.
What is a calcaneal stress fracture?
The middle of the heel is where the pain from heel fat pad syndrome is most noticeable. High-impact sports and activities can also hurt, as can prolonged walking or periods of inactivity. Hard surfaces and barefoot walking might aggravate the discomfort. In contrast to plantar fasciitis, the pain in your heel is more likely to affect both of your feet, occur more frequently at night and while you are resting, and be more common when you are at rest.
Both situations could be present at once. Additionally, plantar fasciitis can lead to heel fat pad syndrome. This happens because it is more challenging to evenly distribute your body weight while jogging or walking when your plantar fascia is injured
Reference
Yi, T. I., Lee, G. E., Seo, I. S., Huh, W. S., Yoon, T. H., & Kim, B. R. (2011). Clinical characteristics of the causes of plantar heel pain. Annals of Rehabilitation Medicine, 35(4), 507. https://doi.org/10.5535/arm.2011.35.4.507Copy to clipboard
Tu, P; Bytomski, JR (15 October 2011). “Diagnosis of heel pain”. American Family Physician. 84 (8): 909–16. PMID 22010770. ^
Rasoulian, McElfresh, Elliott, Rodriguez. “Heel Fat Pad Syndrome – A Clinical Management Guideline” (PDF). PT Coop.org. Archived from the original (PDF) on 2015-06-16. Retrieved 2016-06-03.