Basal Ganglia Stroke
Introduction
An uncommon form of stroke known as a basal ganglia stroke can have distinct long-term implications. The lack of spontaneous speech and emotional blunting are only a few of these side effects. Although these severe consequences may follow a stroke in the basal ganglia, recovery is possible with focused therapy.
The possible long-term repercussions of basal ganglia stroke are discussed in this article. We will also talk about how a survivor’s freedom and day-to-day activities may be impacted by these incidental consequences. After that, you’ll discover how healing is achievable and how to get the most out of your rehabilitation process.
What symptoms might indicate a basal ganglia stroke?
The signs of a stroke elsewhere in the brain will be the same as those of a stroke in the basal ganglia. A stroke occurs when blood flow to a portion of the brain is disrupted, either due to an artery being blocked or a blood vessel rupturing and leaking blood into the neighboring brain tissue.
Common stroke signs may include:
- An abrupt and severe headache
- Loss of coordination or balance, numbness or paralysis on one side of the face or body
- Having trouble hearing or understanding what is being said to you having trouble seeing out of one or both eyes
The symptoms of a basal ganglia stroke may also include the following due to the special structure of the basal ganglia:
- Limiting movements with stiff or weaker muscles
- A lack of symmetry in the smile
- Difficulty swallowing
- tremors
Other symptoms may manifest, depending on which side of the basal ganglia is impacted. You could find it difficult to turn to the left, for instance, if the stroke affects your right basal ganglia. It’s possible that you won’t even notice what’s going on to your left. Severe apathy and confusion might result from a stroke that hits your basal ganglia on the right side.
The Effects of a Stroke on the Basal Ganglia
When the brain’s blood flow is impaired, a stroke happens. A hemorrhagic stroke or an ischemic stroke occurs when an artery bursts, which is referred to as an ischemic stroke. Although a blockage and a hemorrhage are two separate types of stroke processes, both result in harm to the brain’s tissue. Any part of the brain, including the basal ganglia, may be impacted by this.
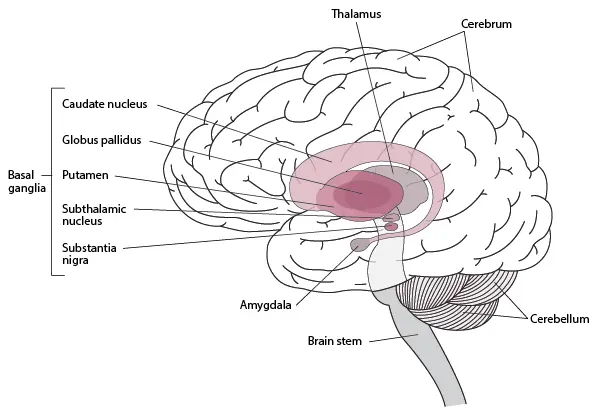
A collection of structures located deep inside the brain are known as the basal ganglia. The cerebral cortex, thalamus, and brain stem are all closely linked to these neural clusters. A lacunar stroke is a specific kind of ischemic stroke that impacts these deep brain regions, including the basal ganglia. The fragile nature of the blood supply deep inside the brain, however, means that many basal ganglia strokes are hemorrhagic even though ischemic strokes are often more prevalent.
Deep in the brain, areas like the basal ganglia receive oxygen-rich blood from a network of arteries known as the circle of Willis.
A rupture in this blood supply brought on by high blood pressure, often known as hypertension, can result in a stroke. Unfortunately, this tissue damage’s effects might have a broad range of unintended consequences. This is due to the fact that these processes are most closely linked to the basal ganglia:
- Voluntary muscle control
- Cognitive function
- Emotion and behavior
- Procedural memory and learning
Any of these activities may be impacted if a stroke damages the basal ganglia. It’s essential to understand that because every stroke is unique, every patient will have unique subsequent effects. In the next part, we’ll go more deeply into the possible side effects of basal ganglia stroke.
Secondary Effects of Basal Ganglia Stroke
The physical, cognitive, and even emotional processes are influenced by the basal ganglia. The results of this kind of stroke are therefore not always obvious. After this kind of stroke, the following consequences are not always present and may not exist at all. Instead, this section offers a broad summary of the basal ganglia stroke’s probable effects.
Motor Impairments
Voluntary muscular control is one of the basal ganglia’s main roles. Compromised control over this might make it challenging to coordinate the motions of the body. As a result, one of the most frequent long-term consequences of basal ganglia stroke is motor disability.
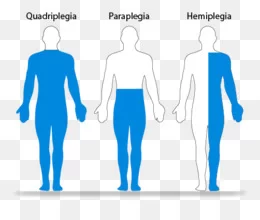
Various motor dysfunctions, such as dystonia and chorea, can happen. These ailments lead a survivor to exhibit unpredictable, fidgety, or irregular movements. Severe basal ganglia stroke can also cause post-stroke paralysis in addition to jerky movements.
The independence, everyday functioning, and even safety of a survivor can all be significantly impacted by these motor impacts. Uncoordinated movements frequently impact a survivor’s balance and ability to walk, which raises the danger of a fall. Furthermore, survivors may be unable to engage in their regular activities, such as activities of daily living, due to weakness or paralysis of certain muscle groups.
Emotional Blunting
After a stroke that affects the basal ganglia, many survivors notice alterations in their emotions or personalities. One research, for example, looked at how basal ganglia problems might affect how you perceive and experience emotion. Particularly, emotional blunting is linked to basal ganglia stroke.
Positive and negative stimuli are evaluated less positively and less negatively, respectively, due to emotional blunting.
A flattened or “blunted” emotional response results from this. Basal ganglia stroke survivors may also struggle more with recognizing faces or names, as well as having issues deciphering others’ emotions.
Post-Stroke Depression
A basal ganglia stroke survivor may not always interpret life after a stroke badly because of emotional blunting, but occasionally it may feel stressful. If so, why is post-stroke depression a frequent long-term complication?
When the left hemisphere of the brain is injured, basal ganglia strokes are more frequently accompanied by depression than other forms of stroke. A key physiologic factor for this is the fact that it happens. Signals that control mood are mostly sent by the basal ganglia but can be disrupted by stroke. An individual who has had these signals interrupted is far more likely to experience depression.
The significant life changes brought on by a stroke may potentially exacerbate this mood disturbance. A survivor could see changes in their physical ability, independence, level of community involvement, or even their housing environment.
For these reasons, a lot of survivors experience post-stroke phases of sorrow, which leads to depression.
Loss of Spontaneous Speech
Multiple functional categories are covered by activities carried out by the basal ganglia. As a result of basal ganglia stroke, many survivors notice alterations in their speech. One research found that basal ganglia stroke victims had sluggish verbal reaction times. When not spoken to, he remained silent. When he did speak, though, his words were clear and concise.
This illustrates how a basal ganglia stroke may affect speech functions, especially with voluntary speech. Basal ganglia stroke sufferers may further have cognitive problems such as impaired attention, memory, or naming skills. However, because each stroke is unique, each survivor will have varied basal ganglia stroke symptoms.
The majority of speech issues following a stroke fall under the category of aphasia. A speech-language pathologist can assist in identifying and treating the specific symptoms of your aphasia because there are many distinct varieties of the disorder.
Changes in Sensation
Some survivors of basal ganglia strokes may have numbness or a loss of feeling in the afflicted body regions. Motor deficits may become even more obvious as a result of this decreased feeling. This is so that the brain can comprehend the position of the body and carry out synchronized actions.
The basal ganglia’s closeness to the thalamus is one potential explanation for sensory problems following basal ganglia stroke. Sensory signals are largely relayed by the thalamus. One of the most frequent post-stroke complications of thalamic stroke is numbness. Reduced feeling can affect a survivor’s safety and danger of subsequent harm in addition to how it affects movement.
No matter what side effects you might have, your healthcare staff is here to assist you in getting better. Your medical and therapeutic team will be able to recognize your particular effects and collaborate with you to develop a successful recovery program. You can recover from a basal ganglia stroke and enhance your function with committed rehab.
How is a stroke of the basal ganglia identified?
Your doctor will want to know your medical history, your symptoms, and when they first appeared when you were in the hospital. They might inquire about you on things like:
- Do you smoke cigarettes?
- Are you diabetic?
- Do you receive high blood pressure treatment?
In order to diagnose the situation, your doctor will also want scans of your brain. They can get accurate images of your brain and its blood arteries through a CT or MRI scan.
The type of stroke you are experiencing can help emergency workers choose the best course of treatment for you.
What is the FAST examination?
Recognizing some of the most apparent stroke symptoms is vital since quick action is the key to a successful stroke response.
The abbreviation for “FAST,” which stands for the following, is recommended by the American Stroke Association:
- Face drooping: Are you unable to smile because one side of your face is numb and unresponsive?
- Arm weakness: Does one arm droop or can you raise both arms high in the air?
- Speech difficulty: Can you comprehend what someone is saying to you and speak clearly?
- Time to call your local emergency services: Call 911 or your local emergency services as soon as you see any of these or other stroke symptoms in yourself or someone close to you.
If you think you could be experiencing a stroke, don’t attempt to drive yourself to the hospital. Make an ambulance call. Let the paramedics examine your symptoms and administer first aid.
Recovery and outlook
People who survive a stroke frequently endure changes that have an impact on their everyday lives. A stroke can be fatal. While some people recover completely, others could have changes that have an impact on practically every part of their lives.
After a stroke, recovery might take some time. Due to the fact that each person is unique and that a stroke can have a variety of effects on a person, it is impossible to anticipate how long it will take or what level of recovery is likely.
It can be exceedingly challenging to anticipate how someone would recover from a basal ganglia stroke, according to experts.
Factors affecting recovery
The consequences on a person and their chances of recovery depend on a number of variables, including:
- How soon the patient receives care
- How targeted their treatment is
- How precisely they treat the area of the brain affected by the stroke
- The degree of the harm
- Permanent consequences: A person may not fully recover from a stroke for months or even years. Strokes can have long-term repercussions. The modifications may become permanent in some persons.
Possible long-term consequences include:
A person’s ability to move may change, and they may have muscular spasms or have trouble regulating movement, such as in their hands.
- Effects on mental health: Mood swings and depression are both mental health disorders.
- Pain: Beginning two to three months following a stroke, a person may begin to experience pain on the afflicted side.
- Changes in thinking: It might be challenging to make judgments and think clearly when you’re confused.
- Bowel and urine incontinence are also possible.
- Speech issues: A person may have trouble comprehending speech, speaking, or both. They might mispronounce or forget words.
Rehabilitation
A person can gain from continuing therapy throughout their recovery, such as:
- Occupational therapy
- Speech therapy
- Physical therapy
Many people may require assistance with everyday tasks, and others may even require a stay in a residential facility. A person can maintain their independence and mobility with the use of walkers, home modifications, and other supports.
Here, brain rewiring is used to demonstrate how a stroke to the basal ganglia can have long-term effects.
In order to encourage neuronal remodelling after a stroke, rehabilitation frequently involves boosting neuroplasticity. Neuroplasticity can be triggered by experience, especially if it is regular and recurrent.
Therapeutic Movement
Different stroke workouts that concentrate on the affected muscles assist in regaining bodily mobility.
It is advised that patients routinely engage in physical therapy to provide their brains with the stimulation it need to recuperate.
Gait modifications are possible with practice.
This therapy restores the ability to walk. Gait treatment attempts to strengthen the legs, feet, and trunk in order to retrain the body to walk more steadily. Physical treatment is frequently to blame for this.
Rehabilitative Occupations
Self-care activities like getting dressed and using the toilet once more will be made much simpler with the help of this assistance. With OT services, coordination may be improved and arms can be strengthened.
Restoring body experience involves engaging in diverse exercises intended to retrain the senses. It is intended to assist your brain in rediscovering how to process tactile information.
Therapy for the Improvement of Speech
Participating in various speech therapy exercises helps with speech restoration. Working with a speech-language pathologist is recommended.
These specialists are skilled in spotting a variety of speech anomalies and creating custom treatment strategies for each patient.
Psychotherapy
For survivors going through emotional changes like depression or emotional blunting, this might be beneficial. Multiple sessions could be necessary to see benefits.
What to anticipate, what to watch out for, and what consequences could result from a basal ganglia stroke?
Investigate the many possible therapy choices.
Risk factors
A basal ganglia stroke is more likely to occur in certain persons than others.
According to research, those who have calcifications on their basal ganglia may be more susceptible to basal ganglia strokes. Those who are older and have a lower body mass index (BMI) tend to be more prone to develop these calcifications.
Other elements that raise the chance of having a stroke include:
- A history of TIA or stroke in one’s family or individually
- High blood pressure
- Heart and blood vascular conditions including high LDL cholesterol and atrial fibrillation
- Diabetes
- Smoking
- A brain aneurysm, which increases the risk of brain bleeding; being under 1 year old or an older adult
- Enduring significant amounts of stress, despair, or anxiety
- Having other health issues, such as kidney or sickle cell disease; taking certain medications, such as blood thinners
- Being obese or having a higher BMI; and using some prohibited substances such as cocaine.
- Heavy alcohol consumption and an unbalanced diet
Prevention
Although a stroke cannot always be avoided, some lifestyle decisions, such as:
- Maintaining a moderate weight
- Eating a balanced diet
- Getting regular exercise
- Controlling diabetes, high blood pressure, and other health issues that raise the risk of stroke
- Avoiding or quitting smoking
- Limiting alcohol use
- Getting enough good quality sleep
- Managing stress
Even while not all risk factors can be avoided, people may start doing things right now to lessen their chance of having a stroke.
Summary
Despite the complexity of basal ganglia stroke, survivors can recover essential skills and perform everyday tasks more effectively. This is especially true if a rehabilitation strategy is followed consistently. You may encourage neuroplasticity, which rewires the brain and helps you restore lost abilities, by exposing the brain to recurrent stimuli.
Even when recuperation has slowed down, gains will resume because the brain still responds to recurrent stimulus. Working closely with your therapy team is of the utmost importance for this reason. Your therapists can assist in customizing your plan to fit your present skills and will work with you to develop meaningful goals. The effort is then up to you to put in.
FAQs
What occurs if a basal ganglia stroke occurs?
A basal ganglia stroke, on the other hand, might result in a rapid loss of balance or coordination, an intense headache, a sudden change in mood and behaviour, or the start of depression.
Can you recover from basal ganglia stroke?
Despite the complexity of basal ganglia stroke, survivors can recover essential abilities and perform everyday tasks more effectively. This is especially true if a rehabilitation strategy is followed consistently.
What type of stroke is a basal ganglia?
The basal ganglia’s blood arteries are very tiny and prone to rupturing. This is why hemorrhagic strokes commonly accompany basal ganglia strokes. Hemorrhagic strokes make for around 13% of all strokes.
What is the recovery time of brain stroke?
Treating and Recovering from a Stroke Everyone’s recovery after a stroke differs; it may take weeks, months, or even years. While some endure a long-term or permanent handicap, others fully recover.
What are the 4 types of strokes?
Types of Stroke
Ischemic Stroke.
Transient Ischemic Attack or Mini-Stroke.
Hemorrhagic Stroke.
Brain Stem Stroke.
References
- Understanding the Consequences & Recovery Process of a Basal Ganglia Stroke. Flint Rehab. https://www.flintrehab.com/basal-ganglia-stroke/
- What to look out for and how to recover from a basal ganglia stroke. NewGait. https://thenewgait.com/blog/basal-ganglia-stroke/
- Basal Ganglia Stroke. Healthline. https://www.healthline.com/health/stroke/basal-ganglia-stroke
- What to know about a basal ganglia stroke. https://www.medicalnewstoday.com/articles/