Bone Bruise
Introduction
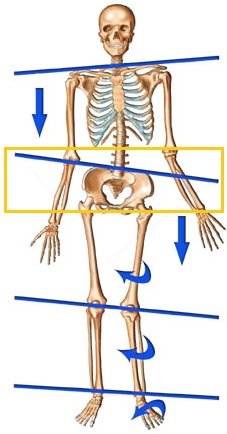
Bone bruises are most common in the lower body, especially in the knees, hips, and ankles. They can also occur in the upper body, such as in the elbows, wrists, and hands.
A traumatic injury to the bone is called a bone bruise. It is not as serious as a fractured bone. When you hear the word “bruise,” you might picture a black and blue stain on your skin, but bruises can also occur in the muscles and bones. This occurs when a tiny blood vessel is injured, allowing blood or other fluid to leak into the surrounding tissues and blood vessels.
Several types of tissue make up bone. The majority of a bone is covered in a thin layer of tissue called the periosteum. There is typically a layer of cartilage at the margins where bones join. This particular bone is known as the subchondral bone. There is a region deep within the bone known as the medulla. It is composed of fibrous tissue known as trabeculae and bone marrow.
When a bone fractures, every trabecula in that area of the bone breaks. However, an injury to a bone bruise only affects a portion of these trabeculae. Another name for it is a microfracture. Blood may accumulate under the periosteum as a result of an injury. A form of bone bruise known as a subperiosteal hematoma is the result. Bleeding and swelling in the space between your cartilage and the bone beneath it could also result from an injury. A subchondral bone bruise results from this. Swelling and bleeding can occur in the bone’s medulla. We refer to this as an intraosseous bone bruise.
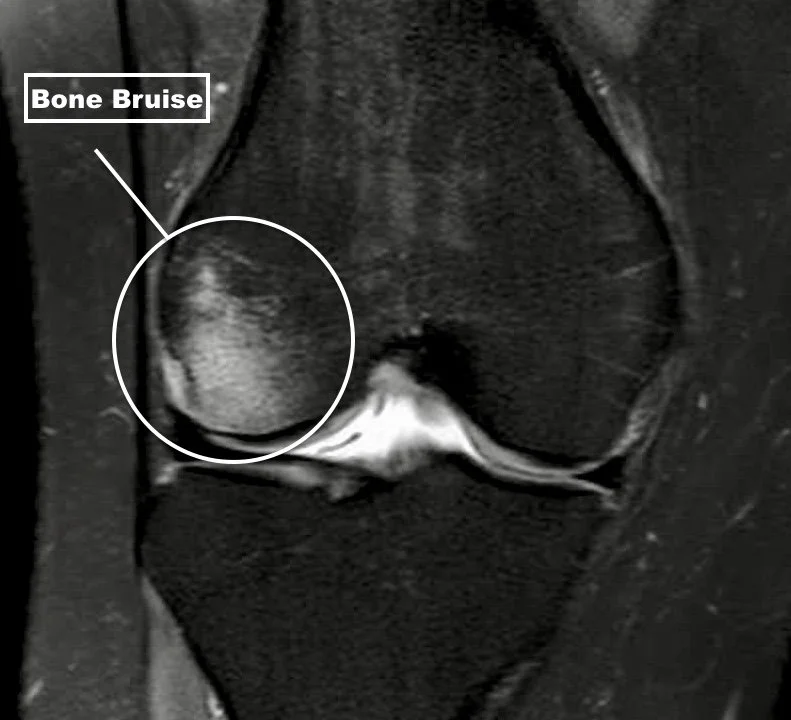
The phrase “bone bruise” is not very old. This is due to the fact that medical professionals only got started to diagnose the injury when magnetic resonance imaging (MRI) started to be used more frequently in recent years. An X-ray fails to show a bone bruise.
Bone bruises occur frequently. All ages are at risk for them. A bone bruise can occur on any kind of bone in your body. A bone bruise is frequently accompanied by additional injuries, such as harm to close ligaments.
After a blow, a blood vessel near the skin’s surface bursts, resulting in bruises. A tiny amount of blood leaks into the tissues beneath the skin from the broken blood vessels.
As the bruise heals, the area will initially appear red before turning blue or purple, green, yellow-brown, and finally returning to the person’s natural skin tone.
In addition to the skin, deeper tissues, organs, and bones can sustain bruises. Even though there may not be any obvious bleeding from these deeper bruises, they can still hurt.
What to Know About a Bone Bruise
Like our skin, our bones can also bruise, and a bone bruise appears like a skin bruise that may appear after a traumatic event. Though less severe than a bone fracture, a bone bruise, also known as a bone contusion, leaves you sore and may hurt.
Understanding Bone Bruises
A visible black-and-blue mark, as you would see with a bruise on your skin, is not always left by bruises to your bone. However, because they both involve injury to the small blood vessels nearby, bruises to the muscle and bone are similar in nature. Your blood penetrates into the surrounding tissue, irritating and inflaming it.
Your body’s bones are composed of three layers:
Periosteum: The hard outer layer of the bone, known as the periosteum, serves to protect the internal structures.
Compact bone: Your body’s second layer provides support and structure. It is smooth, white, and hard.
Spongy bone: Bone marrow is stored in the soft, porous center of your bone.
When you break a bone, the tissue inside your bones is severely damaged, leaving an x-ray-visible crack. A microfracture, in which there is so little tissue damage that it is not visible on an x-ray, is frequently the result of a bone bruise.
Still, the damage results in a subperiosteal hematoma, or blood accumulating around the compact bone beneath the periosteum. Swelling around your bones, cartilage, ligaments, and tendons could result from this. An intraosseous bone bruise is present when bleeding takes place in the middle, softer region of your bone.
Three types of bone bruises are there:
- Subperiosteal hematoma is a condition where blood accumulates beneath the fibrous membrane covering the bone’s surface
- An interosseous bruise is characterized by bleeding and swelling in the bone’s central cavity, which houses the red and yellow bone marrow.
- The subchondral lesion, in which the bone beneath the cartilage swells and bleeds in order to heal
The location of the injury on the bone determines the type of bone bruise.
Most cases of subperiosteal hematoma follow a forceful blow to the bone. In the body’s lower regions, it is typical.
If someone regularly applies excessive pressure to a bone, it may cause interosseous bruising. The majority of athletes who get this kind of bruise are football, basketball, and running players.
Subchondral lesions are caused by either a rotational twisting force or a compressive force that crushes the cells and separates the cartilage and underlying bone. Football and basketball players are also prone to this kind of bone bruise.
Any one of the three types of bone bruises can result from jumping or running on hard surfaces.
Physiology
A specialized type of connective tissue called bone tissue is composed of inorganic minerals (phosphate and calcium) and an organic matrix (collagen and glycosaminoglycans). In an adult human skeleton, 20% is trabecular bone and 80% is cortical bone. Osteons make up both kinds of bone. The solid form of bone is called cortical bone, while the network of trabecular plates and rods that make up trabecular bone resembles a honeycomb. Go here to learn more about the physiology and histology of bone.
Bone Marrow Changes
Changes in the bone marrow in a bone bruise can result from the following:
Increased blood pooling: Severe inflammation results from the blood flow being declined by widened blood vessels.
Fluid inside the bone: When muscles are injured, fluid builds up inside the muscles, causing them to swell. We call this edema. Because bones are hard, they cannot swell. Actually, pressure from fluid in the bones causes pain.
Reactive hyperemia: This is the state in which blood flow returns to normal following a brief disruption.
Fracture: The layer of bone directly beneath the joint cartilage may have a tiny fracture.
The network of fibrous tissues that support trabeculae in a bone. When a bone fractures completely, it means that every single bone trabeculae in that specific region of the bone is broken.
Often, a bone bruise is a warning sign of a fracture. Only a portion of the trabeculae are broken in this specific case.
A bruise can occur on any bone in the body. Bone bruises to the knee, wrist, heel bone, foot, ankle, and hip are common complaints from people.
They frequently occur after a single traumatic incident, like a car accident, sports injury, fall, or strike from a person or object.
Bone bruises and joint sprains can both result from twisting injuries.
Following any of the following trauma types, bone bruises may develop:
- A strike to the bone directly
- The forces resulting from the muscle or skin tearing away from the bone
- Two bones crashed following damage to ligaments
- Harm to adjacent bones
- Every one of these trauma types causes the bone to bruise in a different way.
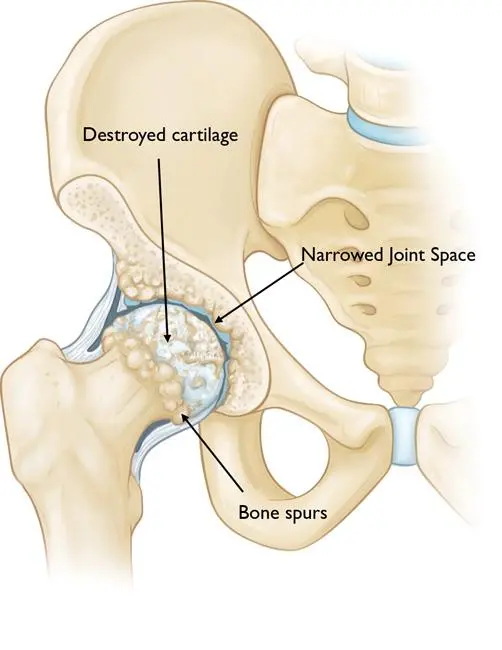
- A bone bruise can also result from medical disorders like arthritis, where the surfaces of the bones may grind against one another
What causes a Bone Bruise?
Although trauma is the most frequent cause of bone bruises, hemophilia A and B and normal stress loading are additionally related to the condition.
The lower limb is the most frequently impacted area.
Patients who sustain a bone bruise typically experience a longer clinical recovery period, greater effusion, and a delayed return to normal function.
There is an 80% chance of concurrently associated bone bruising at the tibial plateau or femoral condyle in patients with ACL rupture. The most significant secondary sign in the diagnosis of ACL injury is the presence of bone bruising in these areas.
MRI showing the presence of bone bruising in (a)the caudal tibia epiphysis and (b) the post-lateral talus region (a, b).
A bone bruise can be caused by any type of injury. They can result from falls from a height, motor vehicle accidents, or sports injuries. a variety of causes, including:
Trauma:
- Direct blow to the bone: This can happen from a fall, being hit by an object, or a car accident.
- Overuse: This can happen from repetitive activities that put stress on the bone, such as running, jumping, or playing sports.
- Twisting injuries: This can happen from activities that involve twisting the joint, such as skiing, snowboarding, or playing sports.
Medical conditions:
- Arthritis: Arthritis can cause inflammation and damage to the cartilage in the joints, which can make the bones more susceptible to bruising.
- Osteoporosis: Osteoporosis is a condition that causes the bones to become weak and brittle, which can make them more susceptible to bruising.
- Hemophilia: Hemophilia is a bleeding disorder that can cause people to bruise more easily than normal.
Other causes:
- Child abuse: Bone bruises can be a sign of child abuse.
- Certain medications: Some medications, such as blood thinners, can increase the risk of bruising.
In some cases, the cause of a bone bruise may be unknown
A bone bruise can be caused by any type of injury. The following are some of the most common causes of bone bruise:
You may be more prone to a bone bruise if you play sports, regularly engage in risky behavior, or are extremely clumsy.
Because bone marrow edema is a traumatic condition, it is now commonly referred to as a “bone bruise.” A bone contusion is another name for a bone bruise.
Anterior cruciate ligament injuries in youth sports
Anterior cruciate ligament (ACL) injuries in athletes have increased as a result of this surge in sports participation.
Rotational stability is provided by the ACL, which crosses the middle of the knee diagonally. The likelihood of an ACL injury is higher among athletes who participate in high-demand sports like basketball, football, and soccer.
observed bone bruises, contusions, or edema following an acute ACL injury. Bone bruises are caused by the forceful impact of the thighbone and shinbone cartilage
What are the symptoms of a bone bruise?
Bone bruise symptoms can include:
- Tenderness and pain where the injury
- Swelling in the affected area and surrounding soft tissues
- A hard lump around
- Change in the color of the damaged region
- Swelling from a joint injury
- Stiffness of a wounded joint
- When compared to a soft tissue injury, this pain is frequently more intense and persistent. The severity of the bone bruise determines the duration and intensity of your symptoms.
Clinical Presentation
| Bone Injury Type | Characteristics | Typical Injury Mechanism |
|---|---|---|
| Sub-periosteal hematoma | A concentrated collection of blood underneath the periosteal of the bone. | Direct high-force trauma to the bone |
| Inter-osseous bruising | Damage of the bone marrow. The blood supply within the bone is damaged, and this causes internal bleeding. | Repetitive compressive force on the bone (extreme pressure on a regular base). |
| Sub-chondral lesion | The lesion occurs beneath the cartilage layer of a joint. | Testing (shearing force) is an extreme compressive force or rotating mechanism that physically crashes the cells. When the energy of the hit penetrates into the bone, the cartilage (or ligament) separates from the underlying bone, causing bleeding. |
Football and basketball players are two examples of athletes who frequently run and jump on hard surfaces and have higher incidence rates of all-bone injuries.
How is a bone bruise diagnosed?
Your physician will inquire about your symptoms and medical background. They’ll inquire as to how you sustained your wound. An examination of the injured area will be performed to check for swelling, bruises, and pain.
Your doctor might be able to determine if you have a bone bruise following the examination. An X-ray does not reveal a bone bruise. However, in order to rule out a bone fracture, you might get an X-ray. A fracture might require a different course of care. A bone bruise can be verified by an MRI. However, your doctor probably won’t order an MRI for you unless your symptoms become more severe.
If someone thinks they may have a bone bruise, it’s critical to seek medical advice.
The illness could be a symptom of something more serious. Seek medical attention if the pain does not get better after taking painkillers if the swelling gets worse, or if it does not get smaller.
Along with a description of the symptoms and a medical history, the doctor will frequently inquire as to how the injury happened. In addition to performing a physical examination, they might look for pain, bruising, and swelling in the injured area.
If the patient’s symptoms do not get better, the doctor might ask for an MRI.
X-rays can be taken to rule out a bone fracture, but they do not show bone bruises. They show up as ill-defined areas in the marrow on MRI scans.
Treatment
medical treatment
Painkillers: Ibuprofen and paracetamol, two over-the-counter pain medications, can help lessen discomfort and inflammation.
Prescription medication: In some cases, your doctor may prescribe stronger pain medication or anti-inflammatory medication.
Surgery: In rare cases, surgery may be necessary to treat a bone bruise. This is usually only done if the bone bruise is very severe or if it is not healing properly.
A physician might advise:
- Putting the injured bone or joint to rest
- Elevating the injured area above the level of the heart reduces swelling.
- Icing the injury multiple times a day
- Using analgesic medications to treat pain and inflammation, such as acetaminophen
- Using a brace to restrict mobility
Undergoing a sub chondroplasty, a procedure in which a physician inserts calcium phosphate, a bone substitute, into the injured area Dependable sources managed by x-ray
To prevent aggravation, avoid applying heavy weights or constant, intense pressure to the affected area. Insufficient rest may delay the healing process and lead to additional harm to the bone or joint.
A medical professional may also recommend a diet. Consuming a diet high in protein, calcium, and vitamin D can aid in the healing process.
avoid smoking; it may delay the healing of broken bones.
Avascular necrosis of the bone may occur in rare instances when the body is unable to restore blood flow to the damaged area. The death of bone tissue from a lack of blood supply is known as avascular necrosis. The damage that results from avascular necrosis in the bone may be irreversible.
The degree of a bone bruise determines how long it takes to heal. Bone bruises can completely heal in as little as three weeks or they can take up to two years.
Although it’s not always possible to avoid bone bruises, maintaining a healthy diet, exercising frequently, giving up smoking, and consuming less alcohol can all help to strengthen and repair bones.
To help protect the bones from additional trauma, it’s also important to play sports while wearing proper safety equipment.
Physical Therapy Management
Depending on the severity of the injury, a doctor’s prescription for pain management and/or anti-inflammatories, load restriction, and RICE are all part of the treatment for a bone bruise. A bone bruise can take a variety of times to heal. After the trauma, the healing period to fully heal this injury can range from three weeks to up to two years.
Physiotherapy plays a significant role in managing bone bruises and promoting recovery. The specific treatment plan will depend on the severity of the injury, the affected area, and individual factors. However, some common physiotherapy interventions for bone bruises include:
- Rest, Ice, Compression, and Elevation (RICE):
This is the cornerstone of initial treatment for bone bruises. Resting the injured area allows for healing, icing reduces swelling and pain, compression helps control bleeding, and elevation promotes fluid drainage.
- Pain Management:
Pain and inflammation can be managed with over-the-counter pain medications such as ibuprofen or acetaminophen. A doctor may prescribe stronger pain relievers in specific circumstances.
- Range of Motion Exercises:
Once the acute pain and swelling have subsided, gentle range of motion exercises can help prevent stiffness and maintain joint flexibility. These exercises should be pain-free and gradually progressed under the guidance of a physiotherapist.
- Strengthening Exercises:
As the healing process progresses, strengthening exercises can be incorporated to restore muscle strength and stability in the affected area. This helps reduce the risk of re-injury and improve overall function.
- Manual Therapy:
Techniques like massage, soft tissue mobilization, and joint manipulation can help relieve pain, improve circulation, and promote healing.
- Hydrotherapy:
Aquatic exercises in a warm pool can provide gentle resistance and support for movement, particularly in weight-bearing joints, while reducing pain and swelling.
- Biofeedback:
This technique helps patients learn to control muscle tension and pain, promoting relaxation and reducing muscle spasms.
- Electrostimulation:
Devices like ultrasound or electrical stimulation can be used to reduce pain, improve circulation, and promote tissue healing.
- Bracing or Taping:
In some cases, a brace or tape may be used to provide additional support and pain relief, especially during activities or movements that aggravate the injury.
- Education and Self-Management:
Physiotherapists educate patients on proper care and rehabilitation techniques, lifestyle modifications to reduce the risk of re-injury, and the importance of monitoring their progress and seeking further medical attention if necessary.
The duration of physiotherapy treatment varies depending on the severity of the injury and individual healing rates. However, most bone bruises resolve within a few weeks with appropriate treatment.
You might receive dietary advice from your healthcare provider. This is due to the fact that consuming a diet high in protein, calcium, and vitamin D can aid in healing. It’s possible that your doctor will advise against using specific over-the-counter pain relievers. Some of these could impede the regular healing of bones. Your healthcare provider will advise you to give up smoking if you currently smoke. Moreover, smoking may interfere with bone repair.
Certain bone bruises on the lower extremities require limited weight bearing. How long you should avoid bearing weight on your bone will be determined by your healthcare provider. Most bone bruises take one to two months to heal gradually. It might take longer for a bigger bone bruise to heal. It might take you weeks or months to be able to resume your sports activities. If you don’t get better, your doctor might order an MRI for you.
What is bleeding into the skin?
Blood may leak into surrounding tissues and areas if a blood vessel bursts. We call this hemorrhaging. Blood can leak into the surrounding skin when bleeding happens right beneath the surface, discoloring it.
This type of skin discoloration usually has a combination of purple, black, blue, and red colors. It can look dark purple, brown, or black on skin that is already dark.
The quantity and kind of blood vessels rupture will determine how much blood is lost as well as how big and ugly the skin discoloration is.
Petechiae, or petechial lesions, are typically caused by breaking just a few small blood vessels or capillaries. These are tiny red dots that appear on the skin’s surface and are less than two millimeters (mm) in width.
Purpura may result from multiple capillaries rupturing in the same location. Small areas of reddish-purple discoloration are the hallmarks of purpura. These patches are bigger than 2 mm and typically have a width of 4 mm to 1 centimeter (cm).
If pressed, neither purpura nor petechiae blanch. This indicates that even after applying light pressure to the area, the discoloration does not go away.
Epichymosis is a collection of blood under the skin’s surface that occurs when numerous capillaries break near to one another. This bruise can vary in size and is either black or bluish-purple in color. But its width is usually more than one centimeter. Unlike most bruises, ecchymosis is not always the result of trauma and may not involve visible swelling.
Trauma-related bruises are typically sensitive to the touch and may have some swelling.
Depending on how bad they are, bruises can take anywhere from a few days to several weeks to heal. Usually, a moderate bruise takes two weeks to completely go away. Lower leg bruises can occasionally take longer to heal.
Hematomas are collections of partially or completely clotted blood. They are also caused by blood vessel breaks. Hematomas can develop in different body parts. A hematoma in an organ or bodily cavity is one example of a serious or possibly fatal event. Some can be minor.
Cause
Most people will occasionally get minor skin bleeding or bruises, usually after an injury where the blood vessels burst. In order to avoid major complications, medical attention is usually required if the bleeding is severe, sudden, or chronic.
Small amounts of bleeding into the skin happen frequently and are usually not disturbing. For a variety of reasons, a person may experience bleeding into their skin.
Most people will bruise and bleed under the skin at some point in their lives. But some individuals are also more prone to bruises than others.
Additionally, there’s a chance of bruising and bleeding into the skin from certain activities. Hematomas and contusions, for instance, are frequent in many sports
Other typical reasons could be:
- Impact wounds
- Wearing shoes, clothes, or glasses that don’t fit well
- Utilizing specific medical equipment, like crutches, casts, or braces
- Aging
- Attempting not to throw up, cough, or cry
- In addition, bleeding into the skin can be a side effect of radiation therapy, chemotherapy, and a host of other medical treatments.
The body’s capacity to form blood clots is also affected by a number of medical disorders and drugs. Excessive or irregular bleeding and bruises may result from this.
The following circumstances could make bleeding and bruises more likely:
- Leukemia
- Tumor
- Histoplasma
- liver or kidney illness
- Aplastic anemia
- Deficiency in vitamin C or vitamin K
- Idiopathic purpura thrombocytopenic
- Vasculitis.
- Tendinopathy
- Throat strep
- Scarlet fever
- Bacterial endocarditis
- Marfan syndrome
- Additionally, some drugs may make bleeding and bruises more likely. These include blood thinners like aspirin (an antiplatelet drug) and warfarin (an anticoagulant), as well as nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen.
However, the a relationship between NSAIDs and increased bleeding. NSAIDs have minimal risk of causing bleeding after some surgical therapies.
Before taking any medication, a person should carefully think about any possible side effects and, if in doubt, seek qualified medical assistance.
Diagnosis
A medical professional will perform a physical examination to determine the cause of bruises if a patient seeks treatment for them. This frequently involves assessing the lesions’ severity and dating them.
It can be more difficult to correctly diagnose bruises on darker skin tones. Alternate light sources have been reported to help detect bruises on dark skin.
- Biofeedback:
This technique helps patients learn to control muscle tension and pain, promoting relaxation and reducing muscle spasms.
- Electrostimulation:
Devices like ultrasound or electrical stimulation can be used to reduce pain, improve circulation, and promote tissue healing.
- Bracing or Taping:
In some cases, a brace or tape may be used to provide additional support and pain relief, especially during activities or movements that aggravate the injury.
- Education and Self-Management:
Physiotherapists educate patients on proper care and rehabilitation techniques, lifestyle modifications to reduce the risk of re-injury, and the importance of monitoring their progress and seeking further medical attention if necessary.
The duration of physiotherapy treatment varies depending on the severity of the injury and individual healing rates. However, most bone bruises resolve within a few weeks with appropriate treatment.
You might receive dietary advice from your healthcare provider. This is due to the fact that consuming a diet high in protein, calcium, and vitamin D can aid in healing. It’s possible that your doctor will advise against using specific over-the-counter pain relievers. Some of these could impede the regular healing of bones. Your healthcare provider will advise you to give up smoking if you currently smoke. Moreover, smoking may interfere with bone repair.
Certain bone bruises on the lower extremities require limited weight bearing. How long you should avoid bearing weight on your bone will be determined by your healthcare provider. Most bone bruises take one to two months to heal gradually. It might take longer for a bigger bone bruise to heal. It might take you weeks or months to be able to resume your sports activities. If you don’t get better, your doctor might order an MRI for you.
What is bleeding into the skin?
Blood may leak into surrounding tissues and areas if a blood vessel bursts. We call this hemorrhaging. Blood can leak into the surrounding skin when bleeding happens right beneath the surface, discoloring it.
This type of skin discoloration usually has a combination of purple, black, blue, and red colors. It can look dark purple, brown, or black on skin that is already dark.
The quantity and kind of blood vessels rupture will determine how much blood is lost as well as how big and ugly the skin discoloration is.
Petechiae, or petechial lesions, are typically caused by breaking just a few small blood vessels or capillaries. These are tiny red dots that appear on the skin’s surface and are less than two millimeters (mm) in width.
Purpura may result from multiple capillaries rupturing in the same location. Small areas of reddish-purple discoloration are the hallmark of purpura. These patches are bigger than 2 mm and typically have a width of 4 mm to 1 centimeter (cm).
If pressed, neither purpura nor petechiae blanch. This indicates that even after applying light pressure to the area, the discoloration does not go away.
Epichymosis is a collection of blood under the skin’s surface that occurs when numerous capillaries break near to one another. This bruise can vary in size and is either black or bluish-purple in color. But its width is usually more than one centimeter. Unlike most bruises, ecchymosis is not always the result of trauma and may not involve visible swelling.
Trauma-related bruises are typically sensitive to the touch and may have some swelling.
Depending on how bad they are, bruises can take anywhere from a few days to several weeks to heal. Usually, a moderate bruise takes two weeks to completely go away. Lower leg bruises can occasionally take longer to heal.
Hematomas are collections of partially or completely clotted blood. They are also caused by blood vessel breaks. Hematomas can develop in different body parts. A hematoma in an organ or bodily cavity is one example of a serious or possibly fatal event. Some can be minor.
Cause
Most people will occasionally get minor skin bleeding or bruises, usually after an injury where the blood vessels burst. In order to avoid major complications, medical attention is usually required if the bleeding is severe, sudden, or chronic.
Small amounts of bleeding into the skin happen frequently and are usually not disturbing. For a variety of reasons, a person may experience bleeding into their skin.
Most people will bruise and bleed under the skin at some point in their lives. But some individuals are also more prone to bruises than others.
Additionally, there’s a chance of bruising and bleeding into the skin from certain activities. Hematomas and contusions, for instance, are frequent in many sports
Other typical reasons could be:
- Impact wounds
- Wearing shoes, clothes, or glasses that don’t fit well
- Utilizing specific medical equipment, like crutches, casts, or braces
- Aging
- Attempting not to throw up, cough, or cry
- In addition, bleeding into the skin can be a side effect of radiation therapy, chemotherapy, and a host of other medical treatments.
The body’s capacity to form blood clots is also affected by a number of medical disorders and drugs. Excessive or irregular bleeding and bruises may result from this.
The following circumstances could make bleeding and bruises more likely:
- Leukemia
- Tumor
- Histoplasma
- liver or kidney illness
- Aplastic anemia
- Deficiency in vitamin C or vitamin K
- Idiopathic purpura thrombocytopenic
- Vasculitis.
- Tendinopathy
- Throat strep
- Scarlet fever
- Bacterial endocarditis
- Marfan syndrome
- Additionally, some drugs may make bleeding and bruises more likely. These include blood thinners like aspirin (an antiplatelet drug) and warfarin (an anticoagulant), as well as nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen.
However, the a relationship between NSAIDs and increased bleeding. NSAIDs have minimal risk of causing bleeding after some surgical therapies.
Before taking any medication, a person should carefully think about any possible side effects and, if in doubt, seek qualified medical assistance.
Diagnosis
A medical professional will perform a physical examination to determine the cause of bruises if a patient seeks treatment for them. This frequently involves assessing the lesions’ severity and dating them.
It can be more difficult to correctly diagnose bruises on darker skin tones. Alternate light sources have been reported to help detect bruises on dark skin.
In order to determine the reason behind bruises, a physician can ask about a patient’s medical history, covering topics such as:
- The possible origins of their bruises or lesions
In order to determine the reason behind bruises, a physician can ask about a patient’s medical history, covering topics such as:
- The possible origins of their bruises or lesions
- Any additional present symptoms
- Usage of medications, particularly NSAIDs and blood thinners
- Previous surgeries or injuries
- Their health history in the family
It’s important to determine as soon as possible whether a person has a history of excessive bleeding. If not, a minor wound might unintentionally turn into an emergency. Early identification of genetic risk factors can help avoid issues and complications in the future.
If the cause is unknown or the doctor suspects an underlying medical condition, they may order additional diagnostic tests. These procedures can take the form of bone marrow biopsies, imaging studies like CT scans, and blood and urine tests.
Treatment and home remedies
Treating minor bruising and bleeding on the skin is not specific. Some home remedies, however, reduce inflammation and aid in the healing process.
Several typical home cures for minor bruises and bleeding into the skin include:
- As soon as possible, apply an ice pack to the affected area for 10 to 15 minutes, and then repeat several times.
- Attempting to keep the wounded area raised
- By applying pressure on the bleeding areas
- For two days after the injury, keep the area away from direct heat sources like saunas, hot tubs, and showers.
- Heating the affected area with a compress for up to 20 minutes, then repeating several times a day
- Consuming a lot of whole fruits and vegetables that are high in antioxidants, including vitamins A, C, D, and E, aids in the healing process.
- Avoid clear of tobacco products and smoking, as these may interfere with the healing process.
- Avoiding alcohol, particularly in the initial two to three days following the injury
- Avoiding vigorous exercise for 24 hours
- Using herbal creams and gels, like vitamin K8 or arnica, several times a day until the bruise goes away
- Taking between 200 and 400 mg Bromelain from a Reliable Source up to three times a day
- Putting the injured bone or joint to rest, avoiding pressure there, and avoiding needless movement
- Using an ice pack all day long to minimize edema
- Resting with your heart above the injured area
- Using medicine to treat inflammation and pain symptoms
- Using a cast or brace to help you limit your movement in order to heal more quickly
A doctor will create a customized treatment plan for more serious cases of bleeding into the skin and bruising, as well as those resulting from an underlying medical condition.
During your visit, your doctor may discuss your diet and lifestyle in order to address any dietary deficiencies that may have contributed to the bone bruise. If you smoke, they might also suggest quitting because it slows down the healing process.
Following an assessment of the extent of your bone bruise, your physician gives you a recovery schedule. It could take two to four months for bone damage to heal. You might want to postpone engaging in physically demanding activities like sports until your bruise fully heals.
Who is at risk for a bone bruise?
Here are some additional factors that can increase the risk of getting a bone bruise:
Here are some of the risk factors that can increase your chances of developing a bone bruise:
- Participation in high-impact sports: Sports like football, basketball, soccer, and rugby involve frequent collisions and falls, making them more likely to cause bone bruises.
- Physically demanding jobs: Occupations that require heavy lifting, repetitive motions, or working on hard surfaces can increase the risk of bone bruises.
- Lack of protective equipment: Neglecting to wear protective gear like helmets, pads, or braces during sports or activities can put you at a higher risk of bone bruises.
- Osteoarthritis: This degenerative joint condition weakens the cartilage in joints, making the bones more susceptible to bruising from impact or stress.
- Osteoporosis: A condition characterized by weak and brittle bones, osteoporosis increases the likelihood of bone bruises, even from minor falls or knocks.
- Hemophilia: This bleeding disorder causes people to bruise and bleed more easily, making them more prone to bone bruises.
- Age: Children and older adults are more likely to develop bone bruises due to softer bones and less joint flexibility. Children and older adults are more likely to get bone bruises than adults in their 20s and 30s.
- Overall health: Individuals with underlying health conditions like autoimmune disorders or bone conditions are more susceptible to bone bruises.
- Certain medications: Blood thinners, corticosteroids, and some other medications can increase the risk of bruising, including bone bruises.
- Genetic predisposition: Some people have a genetic predisposition to bone bruises, meaning they are more likely to develop them than others.
- Overall health: People with other health conditions, such as arthritis or osteoporosis, are more likely to get bone bruises.
- Bone density: People with low bone density are more likely to get bone bruises.
- Activity level: People who are active in sports or other physical activities are more likely to get bone bruises.
If you are concerned about your risk of developing a bone bruise, it is important to talk to your doctor. They can assess your individual risk factors and recommend preventive measures to help reduce your likelihood of experiencing a bone bruise.
If you don’t wear the proper safety equipment for your sport, you could be more likely to sustain a bone bruise. You also face the chance of gaining a bone bruise from other irresponsible activities, such as not wearing your seatbelt.
Prevention
- Wear protective gear: Protect yourself from falls and direct blows to the body by wearing appropriate protective gear during sports or activities. For example, wear helmets, pads, and braces for contact sports like football, soccer, and hockey.
- Warm-up and cool down: Before starting any physical activity, warm up your muscles with light cardio and dynamic stretches. This helps prepare your body for the activity and reduces the risk of injury. After finishing the activity, cool down with gentle stretching to help your muscles recover.
- Maintain a healthy weight: Excess weight puts extra stress on your joints and bones, increasing the risk of bone bruises. Maintain a healthy weight by eating a balanced diet and exercising regularly.
- Get enough calcium and vitamin D: Calcium is essential for bone health, while vitamin D helps your body absorb calcium. Aim to consume adequate amounts of these nutrients through your diet or supplements.
- Strength training: Strengthen your muscles with regular exercise, especially those around the joints that are prone to bone bruises. Strong muscles provide support and stability to the joints, reducing the likelihood of injuries.
- Fall prevention: Falling is a common cause of bone bruises, especially in older adults. Take steps to prevent falls by ensuring your home is free of hazards, using handrails when available, and wearing shoes with good traction.
- Avoid overuse injuries: Overuse injuries are common in activities that involve repetitive motion or high impact. Listen to your body and take breaks when you feel pain or discomfort. Gradually increase the intensity and duration of activities to avoid injury.
- Know your limits: Don’t push yourself beyond your physical limits. Engage in activities that are appropriate for your age, fitness level, and experience. Gradually increase the intensity and duration of activities over time.
- Stay hydrated: Proper hydration is essential for overall health and joint function. Drink plenty of water throughout the day to stay hydrated and support your body’s recovery from activities.
- Regular checkups: If you have underlying health conditions that increase your risk of bone bruises, such as osteoporosis or hemophilia, consult with your doctor regularly to monitor your condition and manage it effectively.
By following these preventive measures, you can significantly reduce your risk of experiencing bone bruises and maintain healthy bones and joints for optimal mobility and quality of life.
Complication
Bone bruises usually heal without any issues. Your body might have problems restoring blood flow to the affected area if your bone bruise is very large. Avascular necrosis of the bone may result from this in rare cases. As a result, that portion of the bone dies.
In the event of a severe bone bruise, the bone may sustain irreversible damage. Larger lesions may make it more difficult for your body to heal entirely. An excessive amount of time without adequate blood flow can cause avascular necrosis or the death of a portion of the bone.
For this reason, you should get medical help as soon as possible if you think you may have bruised a bone. Effective treatment results from early detection.
when blood vessels inside the bone are damaged, causing bleeding and swelling. While most bone bruises heal on their own within a few weeks, there are some potential complications that can arise, particularly in severe cases.
1. Avascular Necrosis (Osteonecrosis):
This is a serious complication that can occur in rare instances when a bone bruise is very large or if there’s significant damage to the blood supply of the bone. Avascular necrosis results from the death of bone tissue due to a lack of blood flow. It is more common in the hip joint but can affect other areas as well.
2. Compartment Syndrome:
This is a dangerous condition that can develop if excessive swelling within a muscle compartment compresses the nerves and blood vessels in that area. Compartment syndrome can lead to permanent nerve damage, muscle damage, or even death of the affected tissue.
3. Joint Stiffness and Pain:
In some cases, bone bruises can cause prolonged stiffness and pain in the affected joint, even after the initial injury has healed. This can be due to inflammation, damage to cartilage, or muscle weakness.
4. Prolonged Recovery Time:
While most bone bruises heal within a few weeks, some can take several months or even longer to fully recover. This is especially true in severe cases or in individuals with underlying health conditions.
5. Recurrence of Bone Bruises:
People who have experienced bone bruises in the past may be more susceptible to developing them again in the same area. This is because the bone may be weaker and more prone to damage.
To prevent complications from bone bruises, it is crucial to seek medical attention promptly if you experience a significant injury, especially if there’s severe pain, swelling, or inability to move the affected joint. Early diagnosis and treatment can help prevent the development of complications and promote faster healing
When to contact a doctor
The occasional minor bruise or bleeding into the skin is rarely a reason for concern.
However, you should see a doctor if you have bruising that lasts more than two weeks or bleeding into your skin without an obvious reason.
Moreover, people using blood thinners who frequently or severely bleed or bruised should also consult a physician.
Additionally, if any of the following symptoms interact with the bruises, it is best to see a doctor:
- Severe suffering
- Blood in the feces or urine
- Gum bleeding
- Swelling in the limbs
- Darkening of the surrounding skin over time around the bruise
- Fever
- Nausea or vomiting
- A big lump where there are bruises
- Fainting or vertigo
- Bone or joint pain
- Repeated bruising in the same location
- Anyone who notices any sudden or severe unexplained bruises should get medical attention right away.
Key points about bone bruise
One type of traumatic injury is a bone bruise. Not as bad as a fractured bone. It results in the accumulation of blood and fluid in and around your fractured bone:
Pain, swelling, and a change in the injured area’s color are possible symptoms.
It is necessary for your healthcare provider to rule out any additional medical issues, like a bone fracture.
An MRI scan is the only way to see a bone bruise. However, an MRI scan is not necessary for its diagnosis or treatment.
In order to prevent the bone from moving, your healthcare provider may treat your bone bruise with rest, ice, pain medication, and a brace.
Avascular necrosis is a rare complication that can arise from a bone bruise. A portion of the bone dies as a result.
Conclusion
Bruising and bleeding into the skin can occur for a number of reasons. Minor wounds, surgical trauma, and certain drugs are among the possible causes.
Meningitis, Marfan syndrome, liver disease, and other illnesses can also cause bleeding into the skin.
Most minor bruises will go away on their own with rest. Supportive measures like elevation and compression, along with drugs like bromelain, can help promote healing.
A person should get medical attention right away if they have severe, ongoing, or unexplained bleeding on their skin.
FAQs
To see a doctor about a bruised bone?
See your doctor right away if you think you may have a bone bruise: Severe bone bruises can impair blood flow if left untreated. Sometimes, this reduction in blood flow can lead to the death of certain bone grafts, which causes any damage done irreversible and permanent.
Does a bone bruise hurt a lot?
In essence, there is some compression on the bone particles, but not enough to result in a fracture. Bone bruises can increase the risk of fracture even though they are less severe than bone fractures. A bone bruise can occasionally be extremely painful, severely restrict range of motion, and require several months to heal.
Is a bruise permanent?
Are bruises ever-lasting? Even though some bruises appear to never go away, they all eventually heal. A bruise that appears to be permanent may indicate one of several possible conditions. It’s a birthmark: Some newborns have marks on their bodies that look like bruises.
Which bone bruise occurs most frequently?
Although trauma is the most frequent cause of bone bruises, hemophilia A and B and normal stress loading are also linked to the condition. The lower limb is the most frequently impacted area. Individuals who sustain a bone bruise typically experience a longer clinical recovery period, greater effusion, and a slower return of motion.
How can one determine whether a bruise is serious?
If the bruise is accompanied by severe pain and swelling, especially if you take medication that thins the blood for a medical condition, make an appointment with the doctor. If you bruise easily or for no apparent reason, get in touch with your doctor. If the bruise is painful and under a fingernail or toenail, get in touch with the doctor.
References
- Bone Bruise – Health Encyclopedia – University of Rochester Medical Center. (n.d.). https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=134&contentid=514
- What to Know About a Bone Bruise. (2021, June 17). WebMD. https://www.webmd.com/a-to-z-guides/what-to-know-bone-bruise
- Nichols, H. (2023, July 27). Everything you need to know about bone bruise. https://www.medicalnewstoday.com/articles/314427
- Bone bruise. (n.d.). Physiopedia. https://www.physio-pedia.com/Bone_bruise
- Understanding Bone Bruise (Bone Contusion). (n.d.). Saint Luke’s Health System. https://www.saintlukeskc.org/health-library/understanding-bone-bruise-bone-contusion



One Comment