Upper Abdominal Pain
Introduction
- Upper abdominal pain or discomfort is a frequent symptom of dyspepsia, also known as indigestion.
- Abdominal pain or discomfort can range from moderate to severe. It could be an intermittent problem that strikes sometimes (recurrent); it could manifest abruptly (acute); it could be a chronic condition that lasts longer than three months.
- Additionally, it may begin mildly and progressively get worse. Colicky pain is defined as pain that waves in and out of perception
What is Upper Abdominal Pain?
- The region of your belly that lies approximately between your ribs and belly button is known as your upper abdomen. To reduce the multitude of potential causes of abdominal discomfort, medical professionals categorize the abdomen into areas. The organs in your upper abdomen are more likely to be the source of your pain. It might feel like a stomachache. It might also affect your muscles or biliary system.
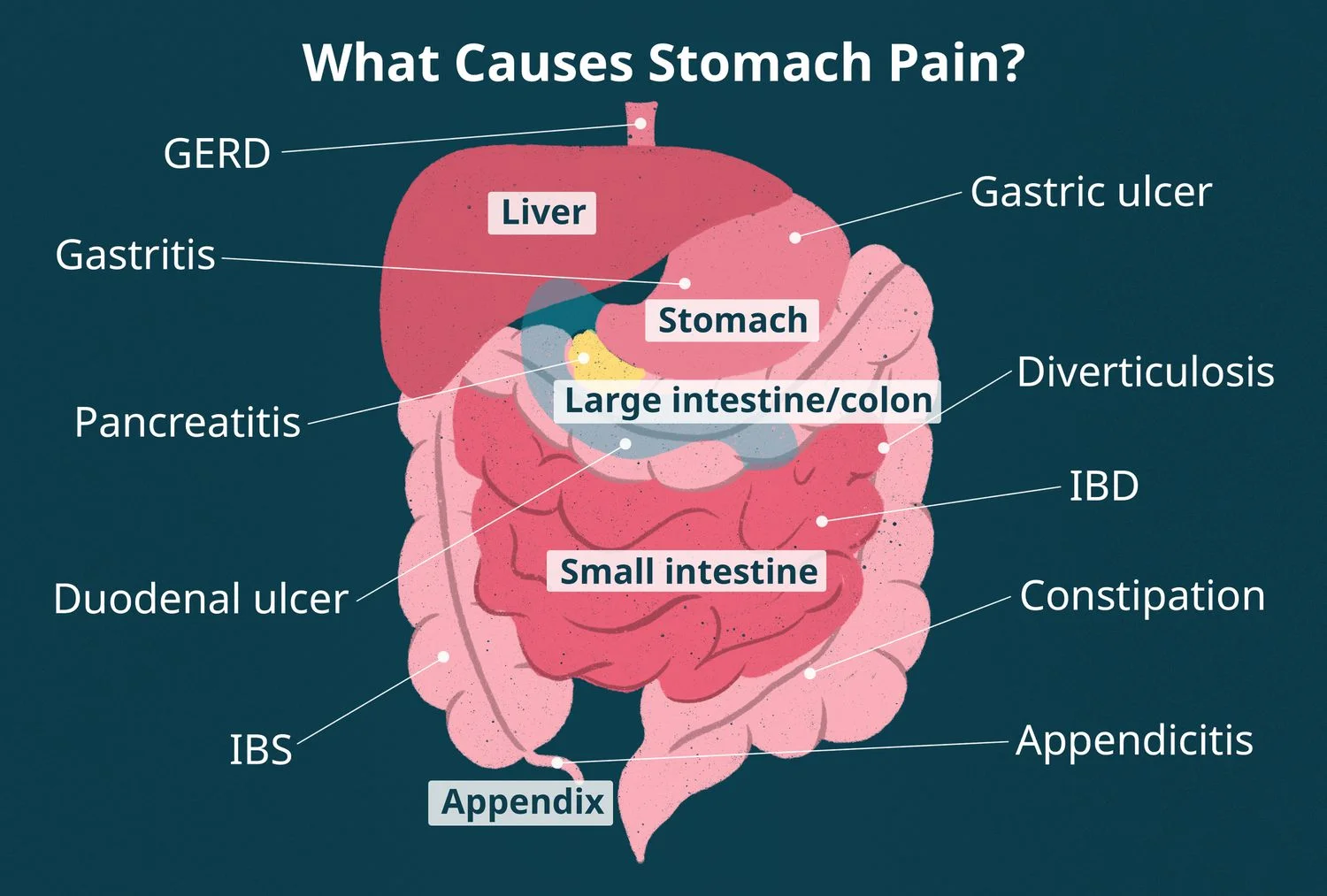
Which organs have Pain in the Upper Abdomen?
- Stomach.
- Spleen.
- Liver.
- Pancreas.
- Gallbladder.
- Bile ducts.
- Other tissues and organs that could be affected are your:
- muscles of the abdomen. Upper abdominal discomfort may result from an injury to one of the major abdominal muscles that meet in your upper abdomen.
- the peritoneum. The tissue that encircles your organs and lines the top chamber of your abdomen is called the peritoneum. The area within is known as the peritoneal cavity. Upper abdominal pain may be brought on by conditions that damage your peritoneum and peritoneal cavity.
- stomach. The bottom portion of your upper abdomen is where the top sections of both of your intestines—your duodenum and transverse colon—pass through. Problems with these areas may result in pain in the upper abdomen.
- Ureters and kidneys. Your kidneys are located near your back, behind your abdominal organs. Your kidneys and urinary tract are connected by your ureters. Pain in these organs may feel as though they are in your front, back, or both.
- Lungs or the heart. Occasionally, chest pain may be indicative of upper abdominal pain.
Pathophysiology
- Other names for stomach pain are visceral or peritoneal pain. The abdomen is divided into three sections: the foregut, midgut, and hindgut. The foregut contains the pharynx, lower respiratory tract, stomach, proximal duodenum, liver, biliary tract (which includes the gallbladder and bile ducts), and pancreas.
- The midgut contains portions of the distal duodenum, ascending colon, appendix, cecum, and first half of the transverse colon.
- The hindgut contains the distal sections of the rectum, sigmoid colon, descending colon, transverse colon, and superior anal canal.
- There is a visceral afferent neuron linked with each segment of the gut that travels alongside the autonomic sympathetic nerves to carry sensory data from the viscera to the spinal cord.
- The term “visceral afferent” refers to the non-specific visceral sensory information that travels from the gut to the spinal cord and overlaps with the very particular somatic afferent nerves.
- Because of this, the distribution of the somatic afferent nerve may exhibit visceral afferent information that flows to the spinal cord.
- For this reason, appendicitis first manifests as T10 periumbilical pain before developing into T12 pain when the abdominal wall peritoneum—which is densely packed with somatic afferent nerves—is affected.
What kinds of upper abdominal pain are there?
- Upper left: The upper left and upper right quadrants are separated by your sternum. This is where your stomach resides. Your pancreas is behind your spleen, which is located on the far left.
- Upper right: The upper right quadrant contains the majority of your biliary system. This comprises half of your pancreas, your gallbladder (on the far right), and most of your liver and bile ducts.
- Upper middle: In the center of your upper belly, your pancreas, liver, and stomach meet. This region is known by doctors as the epigastric region.
- Your digestive system or biliary system may be the cause of your epigastric pain.
- You could be asked to describe the kind of pain you are experiencing by your healthcare professional. If it feels mild, moderate, or severe, they might inquire.
- drab
- or pointed.
- either widespread or specific.
- Gnawing or burning.
- tense or achy.
- Consistent, advancing, or selective (occurring in phases).
- Additionally, you ought to let them know if you experience recurrent bouts of the same discomfort on particular occasions or situations.
- You might sense it more, for instance:
- following a meal.
- following a supine position.
- as you stoop.
- when an object is lifted.
Symptoms
- Early fullness after eating: Even though you haven’t consumed much of your food, you feel stuffed and might be unable to finish it.
- Uneasy satiety following a meal: The sensation of being fuller than usual persists.
- Upper abdominal pain: can range from mild to severe and is felt in the area between your belly button and the base of your breastbone.
- Upper abdomen burning: An excruciating burning or heat sensation is between your belly button and the base of your breastbone.
- Stomach bloating in the upper region: It hurts when your upper abdomen feels restricted.
- Nausea: It would help if you threw up.
Causes of the Upper Abdominal Pain?
- Indigestion: One of the hallmarks of indigestion is epigastric pain following meals, especially if it has a burning sensation. Usually, during digestion, stomach acid is linked to that quality. Heartburn and gastroesophageal reflux disease (GERD) may accompany it.
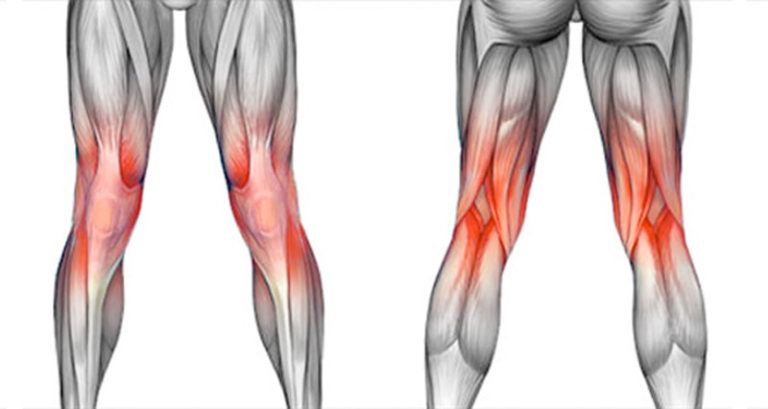
- Straining of the abdominal muscles: An often-occurring injury is a pulled stomach muscle. It can spread through lifting, playing sports, exercising, or even just coughing. Upper abdominal pain is frequently caused by tension in the muscles of the upper abdomen. Pain in the muscles is usually achy.
- Ulcerative stomach illness: Your stomach and duodenum can develop ulcers (sores) due to erosion brought on by stomach acid or a frequent bacterial infection. Stomach pain that is piercing, gnawing, and searing is usually the result of a stomach ulcer.
- Hernias: A hernia develops when a tissue or organ inside of you pushes through a hole in the muscular wall that normally surrounds it. When a hernia pokes through the incision and becomes squeezed or lodged, it may hurt. Abdominal hernias predominate.
- Stones in the kidneys: Gallstone pancreatitis, or pain and inflammation in the gallbladder, is frequently caused by a gallstone that has become lodged in the biliary tract.
- It results in biliary colic, which is characterized by severe abdominal discomfort that peaks and then gradually passes. It happens in spurts, usually right after eating.
- When your fetus grows and starts to press against your upper abdominal organs, you may have upper abdominal pain during pregnancy.
- Growing pains from stretching ligaments, muscles, and tissues are also typical. Sharp, intense, or persistent pain could be a sign of pregnancy problems.
Diagnosis
- Several tests and an open discussion about your symptoms with your doctor can help determine the source of your abdominal discomfort.
- Your doctor will perform a physical examination before recommending tests. To check for soreness and swelling, gently press on several parts of your abdomen.
- It’s also possible to inquire about a person’s past menstrual and sexual experiences from those of reproductive age who were assigned the gender “female” at birth.
- This information will assist your doctor in deciding which tests to order based on the location and degree of the pain within the abdomen.
- Anatomical views of the organs, tissues, and other structures in the abdomen can be obtained through imaging procedures such as MRI scans, ultrasounds, and X-rays. These examinations can aid in the diagnosis of inflammation, fractures, malignancies, and ruptures.
- Additional testing consists of a colonoscopy, which looks into the intestines and colon.
- endoscopy (to find abnormalities and inflammation in the stomach and esophagus)
- upper GI (a specialized X-ray test that looks for growths, ulcers, inflammation, obstructions, and other abnormalities in the stomach by using contrast dye)
- Samples of blood, urine, and feces may also be taken to search for signs of parasite, viral, and bacterial illnesses.
- obtaining a history of the current sickness, or a description of the current symptoms, including the onset, location, length, type, aggravating or relieving causes, and temporal nature of the pain, to learn more about the primary complaint.
- Finding additional potential causes of stomach pain, such as recent travel, recent contact with sick people, and for women, a complete gynecologic history, may help diagnose the underlying cause of the pain.
- finding information about the patient’s previous medical history, paying particular attention to any problems or surgeries.
- Providing the patient’s current medication schedule in detail, including the supplements, OTC drugs, and prescriptions.
- Verifying medication and food allergies of the patient.
- talking to the patient about any family history of illness, with an emphasis on ailments that could be similar to the way the patient is currently presenting.
- talking with the patient about any health-related habits (such as drug and alcohol abuse, tobacco use, and sexual activity) that could increase the likelihood of a certain diagnosis.
- examining the existence of non-abdominal symptoms that might help to further clarify the diagnosis, such as fever, chills, chest pain, shortness of breath, and vaginal bleeding.
- women, a genitourinary examination
Differential diagnosis
Acute abdomen
- A condition in which there is an abrupt onset of intense stomach discomfort for which the underlying reason needs to be identified and treated right away.
- Bowel obstruction, vascular occlusion, infection, or inflammation could be the underlying cause.
- Abdominal distention, fever, shock symptoms, and nausea and vomiting are possible reactions to the pain. Appendicitis is a common illness linked to sudden stomach pain.
By system
- Gastrointestinal
GI tract
gastroenteritis (13%), irritable bowel syndrome (8%), urinary tract issues (5%), stomach inflammation (5%), and constipation (5%), are the most common causes of abdominal pain. Thirty percent of cases have an unidentified cause. - More serious causes account for about 10% of instances, such as pancreas issues (4%), diverticulitis (3%), appendicitis (2%) and cancer (1%).
- Gallbladder issues include gallstones or biliary dyskinesia. Other significant causes include mesenteric ischemia, abdominal aortic aneurysms, and ischemic colitis, which are more common in the elderly.
- Inflammatory conditions include diverticulitis, esophagitis, appendicitis, gastritis, ulcerative colitis, Crohn’s disease, and microscopic colitis.
- Hernia, intussusception, volvulus, tumors, post-surgical adhesions, extreme constipation, and hemorrhoids are examples of obstructions.
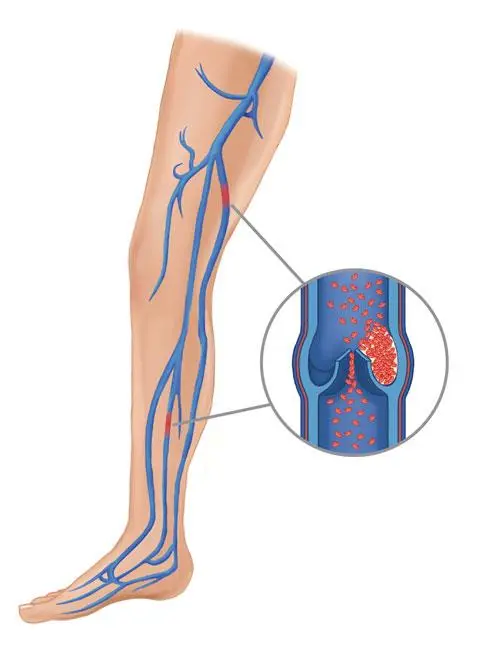
- Vascular conditions include postural orthostatic tachycardia syndrome, embolism, thrombosis, bleeding, sickle cell disease, abdominal angina, and blood vessel compression (such as celiac artery compression syndrome).
- digestive issues include indigestion, food allergies, celiac disease, peptic ulcers, and lactose intolerance.
- Bile system
- Inflammatory: cholecystitis, cholangitis
- Obstruction: cholelithiasis
- Liver
- Inflammatory: hepatitis, liver abscess
- Pancreatic
- Inflammatory: pancreatitis
- Renal and urological
- Inflammation: pyelonephritis, bladder infection
- Obstruction: kidney stones, urolithiasis, urinary retention
- Vascular: left renal vein entrapment
- Gynecological or obstetric
- Inflammatory: pelvic inflammatory disease
- Mechanical: ovarian torsion
- Endocrinological: menstruation, Mittelschmerz
- Tumors: endometriosis, fibroids, ovarian cyst, ovarian cancer
- Pregnancy: ruptured ectopic pregnancy, threatened abortion
- Abdominal wall
- muscle strain or trauma
- muscular infection
- Herpes zoster, radiculitis in Lyme disease, abdominal cutaneous nerve entrapment syndrome (ACNES), and tabes dorsalis are examples of neurogenic pain.
- Pain that is sent from the thorax and includes pericarditis, pneumonia, pulmonary embolism, and ischemic heart disease
- from the spine: radiculitis
- from the genitals: testicular torsion
- Metabolic disturbance
- Lead poisoning, uremia, diabetic ketoacidosis, porphyria, insufficiency of C1-esterase inhibitor, insufficient adrenal glands, bite from a black widow spider, withdrawal from drugs
- Blood vessels
- aortic dissection, abdominal aortic aneurysm
- Immune system
- sarcoidosis
- vasculitis
- familial Mediterranean fever
- Idiopathic
- irritable bowel syndrome (IBS) (affecting up to 20% of the population, IBS is the most common cause of recurrent and intermittent abdominal pain
By Location:
What may be causing the abdominal pain can be inferred from its location.
Four areas on the abdomen are referred to as quadrants. Locations and related circumstances consist of
Right upper quadrant
- Liver: abscess, hepatitis, fatty liver, hepatomegaly, and liver cancer
- Gallstones, worm infection, cholangitis, and inflammation of the gallbladder and biliary tract
- colon: inflammation, spasm, gas buildup, functional abnormalities, intestinal blockage, and colon cancer
- Other: pneumonia, Fitz-Hugh-Curtis syndrome
Left upper quadrant
- Splenomegaly
- Bowel: small bowel obstruction, inflammation, intestinal spasm, Celiac disease, mesenteric ischemia, and functional abnormalities
- Lower abdominal pain
- Diarrhea
- Colitis
- Crohn’s
- Dysentery
- Hernia
Right lower quadrant
- Colon: intussusception, bowel obstruction, appendicitis (McBurney’s point)
- Renal: kidney stone (nephrolithiasis), pyelonephritis
- Pelvic: pelvic inflammatory illness, pelvic pain syndrome, bladder cancer, cystitis, and bladder stones
- Gynecologic: endometriosis, ovarian cyst, ovarian torsion, fibroid (leiomyoma), abscess, ovarian cancer, endometrial cancer, intrauterine pregnancy, ectopic pregnancy
Lower left quadrant
- Bowel: gas buildup, sigmoid colon volvulus, diverticulitis, bowel obstruction, and toxic megacolon
Treatment of Upper Abdominal Pain
Medical Treatment
- The treatment of the pain is one of the factors that affect how abdominal pain is managed. Some dietary adjustments that people may make include: taking a nap after a meal, chewing food thoroughly and slowly, and steering clear of high-stress or high-excitation circumstances right after.
- To treat the pain, your doctor may recommend a pain-modifying medication like trazodone or amitriptyline. These could assist in altering the manner. Pain signals are processed by the brain.
- When someone arrives at the emergency room complaining of stomach discomfort, they might first need IV fluids because their intake may have reduced as a result of the pain and could even be vomiting or emesis.
- OTC antacids can help ease indigestion if it appears to be a straightforward case. NSAIDs (nonsteroidal anti-inflammatory medicines) like ibuprofen or aspirin may be helpful for general pain and inflammation.
- Analgesia, which includes non-opioid drugs like ketorolac and opioid drugs like morphine and fentanyl, is a treatment option for stomach discomfort.
- Since ketorolac can exacerbate certain intra-abdominal processes, the choice of analgesia depends on the underlying cause of the discomfort.
- Individuals arriving at A “GI cocktail” consisting of lidocaine plus an antacid (such as omeprazole, ranitidine, magnesium hydroxide, and calcium chloride) may be given to patients experiencing abdominal pain in the emergency room.
- In certain cases of stomach pain, antimicrobial therapy may be useful after pain management. Some people find relief using butylscopolamine, often known as Buscopan, to relieve cramping stomach pain.
- However, more rigorous treatments like shock wave lithotripsy may be necessary for other disorders including kidney stones. Surgery to remove gallbladder inflammation may be necessary.
- To treat the pain, your doctor may recommend a pain-modifying medication like trazodone or amitriptyline. These could assist in altering the manner. Pain signals are processed by the brain.
- An experienced medical practitioner would probably test you about your symptoms and the type of pain you are experiencing if you are experiencing severe stomach pain and need to be seen. They will use your responses to determine the appropriate course of tests and diagnosis.
- The surgical treatment of appendectomy, exploratory laparotomy, and cholecystectomy are among the procedures used to treat abdominal pain
Surgery
Types of upper abdominal surgery
- Segmental colectomies
- Usually, the diseased region of the bowel is covered by a vertical incision made in the middle of the belly. The diseased section of the colon is excised.
- If the excision is for cancer, an attempt is made to remove more tissue, including lymph nodes. To make the bowel watertight and promote healing, the ends are linked together (anastomosis).
- Abdominoperineal resection
- The purpose of this procedure is to treat rectal cancer, both anal and distal. The accompanying vessels and lymph nodes are removed together with the anus, rectum, and a portion of the sigmoid colon.
- The colon’s end is then introduced through a hole created in the abdominal wall. We refer to this as a colostomy.
- Small bowel resection
- The purpose of this procedure is to remove polyps, benign tumors, ulcers, malignancy, and Crohn’s disease.
- A section of the small intestine is removed. The small intestine’s damaged sections will be removed by the surgeon, who will then suture the good sections back together.
- An ostomy—an opening to the exterior of the body—is made if necessary.
- Repair of parastomal hernias
- A hernia is the most typical issue with an ostomy. An ostomy is an incision made in the abdominal wall to expose the bowel to the skin. Fat or another bowel loop can enter the gap in the abdominal wall next to the colon.
- Using mesh or sutures, the hernia is repaired; occasionally, the ostomy is relocated to a different location on the abdominal wall.
Effects of Surgery
- You can have several attachments after the procedure, including an IV, a catheter, drainage, and oxygen. This may make mobilization challenging.
- After surgery, you must be able to manage your pain well enough to facilitate your recovery. Throughout your stay, daily painkillers will be provided to you.
- You should expect some degree of pain because you underwent a significant surgical procedure. If, however, your pain is not adequately managed, do let the physicians or nurses know.
- You might be tempted to breathe more shallowly after your abdominal surgery because of your immobility and pain, but doing so increases your risk of getting a chest infection.
- Therefore, the physiotherapist can instruct you in breathing techniques to assist in getting rid of any mucus on your chest.
Physiotherapy Treatment
Goal: This Article’s objective is to give you knowledge and suggestions that will maximize your recovery. Patients who have undergone abdominal surgery are the target audience. The physiotherapist’s job is to help you get back on your feet and ensure your discharge home is safe.
Breathing Exercises
Position: Either on a chair or on the bed, sit as straight as you can.
- Method: 1) Let your shoulders and upper chest drop.
- 2) inhale deeply and slowly via your nose.
- 3) Take a three-second breath hold.
- 4) Exhale deeply through your lips you can.
Circulation Exercises that improve circulation are essential for reducing swelling, avoiding blood clots, and improving circulation.
- Every thirty minutes, quickly raise and lower your feet ten to twenty times.
- Make circles with your ankles.
- Put your buttocks together tightly exercises.
- Bed mobility and sitting out of bed
- When: After your procedure, it’s critical to get out of bed and sit as soon as feasible.
- Why: Staying upright will help you breathe easier and feel better overall. It is also the ideal posture for your lungs.
- Who: The nursing staff or the physiotherapists on the ward can assist you with this.
- How to exit the bed: As you roll onto your side, flex your knees. To get into a sitting posture, cross your legs over the edge of the bed, drop your feet to the floor, and use your elbow to push yourself up.
- You must spend as much time as you can manage sitting out of bed the day after your operation. Make an effort to spend more time outside each day.
Walking
- Boosts stamina, strength
- Enhances self-reliance
- Prevents chest infections
- Lowers blood clot risk
- endurance
- How much: Make an effort to walk more each day, little by little.
- Short walks are advised.
- Take a few steps, for instance, to the bathroom, around the bed, and to the window.
- Depending on your prior degree of movement and the number of attachments you have, you might first need assistance from the staff.
Abdominal exercises
- Start: Two days following surgery.
- Why: Strengthen the muscles in your deep abdomen, improve blood flow there, and aid in the healing process.
- Try these three exercises twice a day for about three months. as many repetitions as possible
- Position: Head resting on a pillow, knees bent, feet flat on the bed, lying on the bed.
Static abs
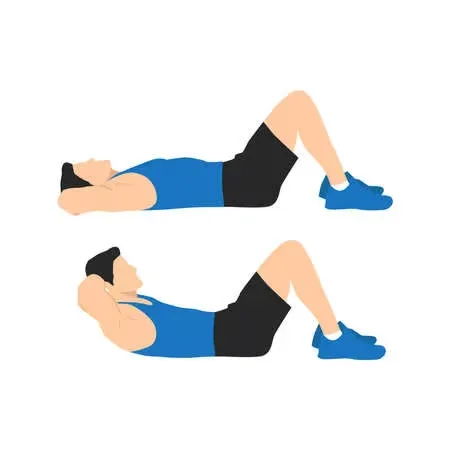
- Press your hands against your lower abdomen.
- Pull your belly button gently down towards your spine as you exhale through your nose. Try to maintain this for five seconds.
- Five times over, repeat.
Pelvic Tilting
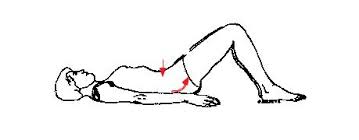
- Contract the muscles in your abdomen.
- Then curve your buttocks up and press the base of your spine into the bed.
- Hold for three seconds.
- then gently let go.
- It would help if you repeated each side five times.
Knee rolling
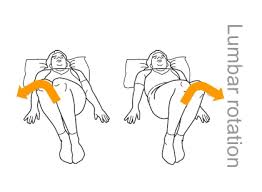
- As far as is comfortable, slowly roll your knees down each side while keeping them together
- Each side should be repeated five times.
Recovery
- Week 1:Frequently take quick strolls
- Exercises for the abdomen
- Take breaks during the day.
- Refrain from heavy lifting
Weeks 2 through 5:Keep up the exercises and walking; go farther as you can and as feels comfortable; - Take regular breaks; be sure to pace your activity
- Light housekeeping, such as cooking and cleaning
- No heavy lifting yet
Week 6: Low-impact aerobics; flat-surface cycling; driving (practice emergency stop
Week 12: Regular business as usual - Resuming preferred exercise gradually is advised, especially for competitive or high-intensity sports like tennis, running, and cycling up hills.
Summary
- upper abdominal symptoms accompanied by duodenal or stomach ulcers include neoplasms (primary tumor or metastatic illness), infections (e.g., TB, Mycobacterium avium intracellulare, cytomegalovirus, herpes simplex virus), and infiltrative disorders.
- Another cause of severe upper abdominal pain is acute pancreatitis; globally, the most prevalent causes are gallstones and alcohol, while infectious etiologies are significant in immunocompromised patients. Diabetes mellitus, steatorrhea, and stomach discomfort are the hallmarks of chronic pancreatitis.
- Most occurrences of chronic pancreatitis globally are caused by alcohol misuse; however, in many tropical regions, tropical calcific pancreatitis is the most prevalent cause of the condition.
- Generalized abdominal pain and tenderness may be caused by peritonitis, which can develop as a result of perforated peptic ulcer, ileal perforation in typhoid fever, colonic perforation in amebic colitis, or rupture of a hydatid cyst. Acute mesenteric ischemia is characterized by severe stomach discomfort and little to no tenderness in the area.
- Apart from surgical situations, it’s crucial to take into account “medical” reasons for stomach discomfort. Vaso-occlusion in sickle cell disease patients can induce acute painful episodes that are hard to differentiate from other causes of an acute abdomen.
- One of the most prevalent symptoms of many infectious disorders, including malaria, is abdominal pain.
FAQ
What is causing the upper abdominal pain?
Temporary inflammation of the stomach and occasionally the intestines can be brought on by a transient stomach virus or bug (gastroenteritis). Long-lasting stomach discomfort and inflammation might be brought on by other illnesses.
Among these less frequent reasons are autoimmune diseases, bile reflux, and stomach cancer.
When might upper abdominal pain cause me concern?
If upper abdomen discomfort becomes severe, persistent, or occurs after direct damage to the region, get medical attention right away.
It’s especially imperative to visit the ER if upper abdominal pain is accompanied by changes in stool color, exhaustion, or severe dehydration.
Which three categories of stomach pain exist?
Visceral, parietal, and transferred pain are the three primary categories of stomach pain. Stretching of the nerves passing through an organ’s walls results in visceral pain. The discomfort usually feels like a dull ache or cramp and is not very localized.
How does the ache in the upper stomach feel?
Indigestion is a gnawing or searing ache or pain in your upper belly that may get better or worse after you eat
What is the duration of upper gas pain?
Chest ache from gas should go away really quickly. Within 30 to 45 minutes of using natural therapies, it should begin to go away.
References
- Watson, K. (2023, February 14). Inconsistent Sharp Abdominal Pain Causes and Treatment. Healthline. https://www.healthline.com/health/sharp-stomach-pain-that-comes-and-goes#diagnosis
- Professional, C. C. M. (n.d.). Upper Abdominal Pain. Cleveland Clinic. https://my.clevelandclinic.org/health/symptoms/24736-upper-abdominal-pain
- Abdominal pain. (2023, November 29). Wikipedia. https://en.wikipedia.org/wiki/Abdominal_pain#cite_note-Vin2014-2
- Types of Abdominal Surgery | MedStar Health. (n.d.). https://www.medstarhealth.org/services/abdominal-surgery
- McKechnie, D. (2023, July 4). Abdominal Pain. https://patient.info/signs-symptoms/abdominal-pain-leaflet
- Indigestion – Symptoms and causes – Mayo Clinic. (2023, July 7). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/indigestion/symptoms-causes/syc-20352211