Bursitis and Physiotherapy Treatment
Introduction:
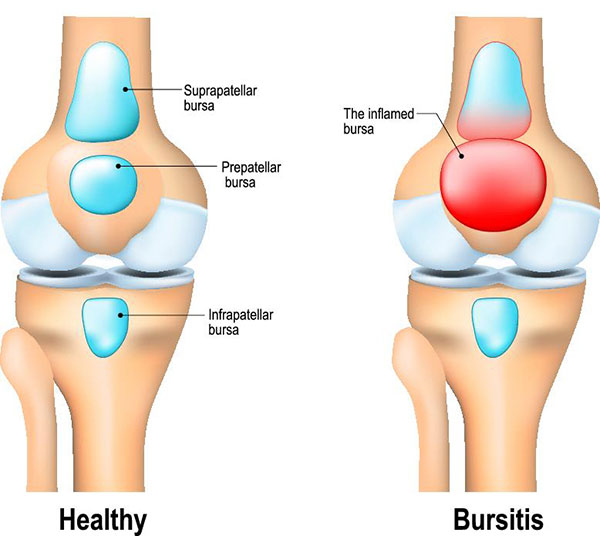
Wherever skin, muscles, or tendons need to slide over the bone is home to bursae. A bursa (singular) is a sac made of thin, slippery tissue. They could be compared to a blister as they are lubricated with a small amount of fluid inside their outer layer. A healthy bursa helps reduce friction created from the sliding parts, such as between tendon and bone.
Bursitis is the inflammation of a bursa. An inflamed bursa, or bursae, can cause the patient pain, swelling, and tenderness around a joint with bursitis. This pain can be mild and bothersome to acute and very problematic. Although it is more common in older adults, the younger population can be affected too.
Bursitis can be developed in many areas, but the focus of this article touch on knee, elbow, hip, and heel bursitis.
Definition:
Bursitis is the inflammation of a bursa, a small fluid filled sac that sits between muscles, tendons and bones to reduce friction.
Types of bursa:
- Synovial bursae, which are located between bones and muscles, tendons, and ligaments.
- Superficial bursa, which are located just below the skin, between skin and bone.
- Adventitious or accidental bursae, which develop because of repeated irritation.For example, a person who regularly wears constricting shoes or has abnormal foot anatomy may develop a bursa on the outside of the big toe joint (a prominent bursa at this location is called a bunion).
Types of Bursitis:
Although bursitis can occur anywhere in the body where bursae are located, there are several specific types of bursitis, including the following:
- Anterior Achilles tendon bursitis : This type of bursitis is also called Albert’s disease. Extra strain on the Achilles tendon, such as injury, disease, or shoes with rigid back support, causes this condition, which is characterized by inflammation of the bursa located in front of the attachment of the tendon to the heel.
- Posterior Achilles tendon bursitis : This type of bursitis, also called Haglund’s deformity, is located between the skin of the heel and the Achilles tendon (which attaches the calf muscles to the heel). Aggravated by a type of walking that presses the soft heel tissue to the hard back support of a shoe, this type of bursitis occurs mostly in young women.
- Hip bursitis : Also called trochanteric bursitis, hip bursitis is often the result of injury, overuse, spinal abnormalities, arthritis, or surgery. This type of bursitis is more common in women and middle-aged and older people.
- Elbow bursitis : Elbow bursitis is caused by the inflammation of the olecranon bursa located between the skin and bones of the elbow. Elbow bursitis can be caused by injury or constant pressure on the elbow (for example, when leaning on a hard surface).
- Knee bursitis : Bursitis in the knee is also called goosefoot bursitis or Pes Anserine bursitis. The Pes Anserine bursa is located between the shin bone and the three tendons of the hamstring muscles, on the inside of the knee. This type of bursitis may be caused by lack of stretching before exercise, tight hamstring muscles, being overweight, arthritis, or out-turning of the knee or lower leg.
- Kneecap bursitis : Also called prepatellar bursitis, this type of bursitis is common in people who sit on their knees a lot, such as carpet layers and plumbers.
common sites of Bursitis :
- Subacromial bursitis
- Olecranon bursitis – students elbow
- Prepatellar bursitis – housemaid’s knee”
- Infrapatellar bursitis – clergyman’s knee”
- Prepatellar bursitis – Baker’s Cyst
- Trochanteric bursitis of hip
- Retrocalcaneal bursitis
- Ischial bursitis – weaver’s bottom”
- Iliopsoas bursitis
Mechanism of Injury / Pathological Process
When a Bursa gets inflamed, it swells, develops friction and starts irritating the muscle tendon it is supposed to protect. This way the bursa and muscle tendon get more and more irritated.
These issues lead to bursitis and tendinitis.
- Overuse of the joint: for example vacuuming for hours on end
- Repetitive strain: for example picking up and lifting heavy loads
- Trauma: by falling on your elbow or bumping it against something
- Pressure: leaning on the elbow at a desk is a common cause of bursitis among students
- Bacterial infection: from an unattended wound (this is called septic bursitis)
- Other inflammatory diseases: Gout for instance:☃☃ the gout crystals can form in the bursa and cause the inflammation.
Epidemiology/Etiology
Bursitis may occur:
- Mainly by constant friction, thumping or pressure
- The inflammation of the bursa frequently appears in combination with tendinitis
- By an overuse injury or a trauma, especially when pulling and pushing heavy items
- After a forced period of rest
- There also can be an underlying rheumatic condition
- Diabetes, osteoarthritis and disability of the thyroid gland can be associated with bursitis.
Symptoms of bursitis :
If you have bursitis, the affected joint might:
- Feel achy or stiff
- Hurt more when you move it or press on it
- Look swollen and red
When to see a doctor
Consult your doctor if you have:
- Disabling joint pain
- Sudden inability to move a joint
- Excessive swelling, redness, bruising or a rash in the affected area
- Sharp or shooting pain, especially when you exercise or exert yourself
- A fever
Risk factors
Anyone can develop bursitis, but certain factors can increase your risk:
Age. Bursitis becomes more common with aging.
Occupations or hobbies. If your work or hobby requires repetitive motion or pressure on particular bursae, your risk of developing bursitis increases. Examples include carpet laying, tile setting, gardening, painting and playing a musical instrument.
Other medical conditions. Certain systemic diseases and conditions — such as rheumatoid arthritis, gout and diabetes — increase your risk of developing bursitis. Being overweight can increase your risk of developing hip and knee bursitis.
Prevention
While not all types of bursitis can be prevented, you can reduce your risk and the severity of flare-ups by changing the way you do certain tasks. Examples include:
- Using kneeling pads. Use some type of padding to reduce the pressure on your knees if your job or hobby requires a lot of kneeling.
- Lifting properly. Bend your knees when you lift. Failing to do so puts extra stress on the bursae in your hips.
- Wheeling heavy loads. Carrying heavy loads puts stress on the bursae in your shoulders. Use a dolly or a wheeled cart instead.
- Taking frequent breaks. Alternate repetitive tasks with rest or other activities.
- Maintaining a healthy weight. Being overweight places more stress on your joints.
- Exercising. Strengthening your muscles can help protect your affected joint.
- Warming up and stretching before strenuous activities to protect your joints from injury.
Treatment of bursitis:
Conservative, nonsurgical care is almost always the treatment for bursitis. Initial treatments can include rest from pain provoking movements, activity/sport modification, and medications. Medications include anti-inflammatories for pain and swelling, or antibiotics for infections.
Physiotherapy treatment:
Physiotherapy treatment is very important in the treatment of bursitis. Modalities such as
- Ice : apply ice to the area to decrease bursa inflammation. We generally recommend that you apply a large ice pack on the affected area for 20 to 30 minutes. You should repeat the ice application 2 to 3 times a day until your physiotherapist advises you to cease.
- ultrasound : Untreated bursitis can result in calcification (bone growing) within the bursa and even nastier pain and disability.
- Iinterferential current
- Acupuncture can help reduce pain and inflammation.
- Do range-of-motion exercises each day. If your bursitis is in or near a joint, gently move the joint through its full range of motion, even during the time that you are resting the joint area. This will prevent stiffness. As the pain goes away, add other exercises to strengthen the muscles around your joint.
- Avoid tobacco smoke. Smoking delays wound and tissue healing.
- Biomechanics of the affected limb are evaluated to identify contributing influences such as postural problems and habits, muscle tightness, muscle weakness and footwear problems. Patient involvement is required as stretching, strengthening and movement retraining exercises are almost always prescribed to improve the function about the joint that has the painful bursitis. Sometimes, a change in shoe or additional arch support such as an orthotic may be required in the case of heel bursitis.
- A cortisone injection into the bursa is ordered by the doctor to “kick start” the improvement cycle, but this tends to be the exception rather than the rule. For the most part, very good results are seen with time and disciplined adherence to activity modifications, exercise prescriptions and physiotherapy treatments.
- R.I.C.E. – Rest, Ice, Compression, and Elevation.
- Aspiration of the bursa fluid for evaluation in the laboratory.
- Splints.
Septic Bursitis
Bursa that becomes infected with bacteria. Treatment may include:
- Antibiotic medications
- Repeated aspiration of the inflamed fluid
- Surgical drainage and removal of the infected bursa sac (bursectomy)
Surgery in bursitis :
Patients who do not respond to nonoperative care may choose surgery to remove the bursa, or bursae. This process is referred to as bursectomy. With surgery there is always a risk of additional problems or complications. As such, it is not the first step in treatment but more of a last resort.
Depending on the location of the bursa other surgical techniques may be required. For example, the hip area may require a portion of the bone to be removed.
In the heel, an osteotomy of the bone may help change the patient’s alignment and remove pressure off the bursa. This process involves the removal of a tiny wedge-shaped piece of bone in the heel in order to rotate it just enough to eliminate pressure from the bone on the bursa.








5 Comments