BRACHIAL PLEXUS INJURY
INTRODUCTION:
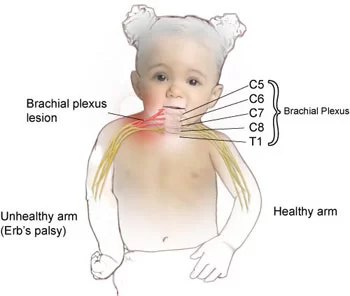
A brachial plexus injury (BPI), also known as brachial plexus lesion, is an injury to the brachial plexus, the network of nerves that conducts signals from the spinal cord to the shoulder, arm and hand.
These nerves originate in the fifth, sixth, seventh and eighth cervical (C5–C8), and first thoracic (T1) spinal nerves, and innervate the muscles and skin of the chest, shoulder, arm and hand.
Brachial plexus injuries can occur as a result of shoulder trauma, tumours, or inflammation.
The rare Parsonage Turner syndrome causes brachial plexus inflammation without obvious injury, but with nevertheless disabling symptoms.
But in general, brachial plexus injury can be classified as either traumatic or obstetric.
Obstetric injuries may occur from mechanical injury involving shoulder dystocia during difficult childbirth.
Traumatic injury may arise from several causes. “The brachial plexus may be injured by falls from a height on to the side of the head and shoulder, whereby the nerves of the plexus are violently stretched.
The brachial plexus may also be injured by direct violence or gunshot wounds, by violent traction on the arm, or by efforts at reducing a dislocation of the shoulder joint”.
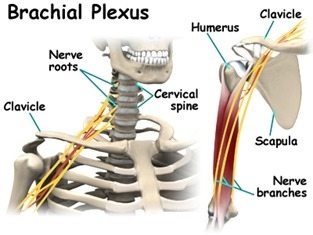
ANATOMY OF BRACHIAL PLEXUS:
The brachial plexus is formed from five nerves that originate in the spinal cord at the neck.
The plexus connects these five nerves with the nerves that provide sensation to the skin and permit movement in the muscles of the arm and hand. There is a brachial plexus on each side of the body.
Each of the five nerves in the brachial plexus has a specific function, such as powering muscles or carrying sensory information from the hand to the brain.
Because each nerve has a function, the location of the nerve injury within the plexus is important for predicting outcomes and for planning treatment.
The brachial plexus has five anatomic sections, and injuries to the brachial plexus can occur in one or more of these areas.
- Spinal nerves
- Trunks
- Divisions
- Cords
- Branches
Clinical Anatomy:
The plexus consists of roots, trunks, divisions, cords and branches.
Roots:
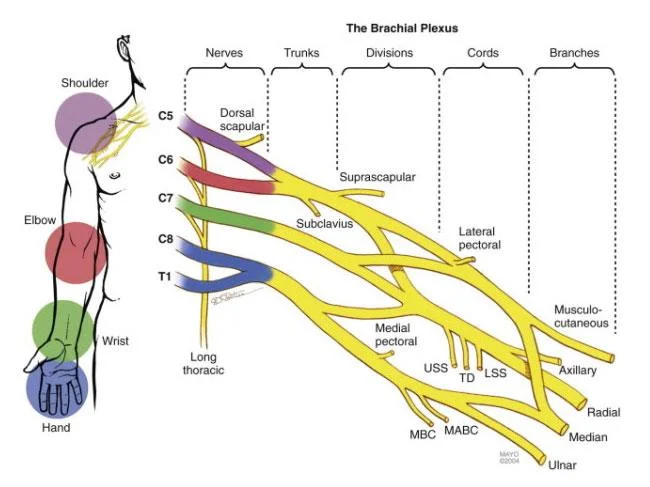
- These are consititued by the anterior primary rami of spinal nerves C5,6,7,8 and T1 with contributions from the anterior primary rami of C4 and T2.
- The origin of the plexus may shift one segment either upward or downward resulting in a pre-fixed plexus or post-fixed plexus respectively.
- In a prefixed plexus, the contribution by C4 is large and in that from T2 is often absent.
- In a post fixed plexus, the contribution by T1 is large, T2 is always present, C4 is absent, and C5 is reduced in size.The roots join to form trunks as follows:
Trunks:
- Upper trunk is formed by C5 & C6
- Middle trunk is formed by C7
- Lower trunk is formed by C8 & T1
Divisions (of the trunk):
- Each trunk divides into ventral and dorsal divisions (which ultimately supply the anterior and posterior aspects of the limb).
- These divisions join to form cords.
Cords (it forms 3 cords):
- The Posterior Cord is formed from the three posterior divisions of the trunks (C5-C8,T1)
- The Lateral Cord is the anterior divisions from the upper and middle trunks (C5-C7)
- The Medial Cord is simply a continuation of the anterior division of the lower trunk (C8,T1)
MECHANISAM OF INJURY:
Injury to brachial plexus can occur in many ways. These include the contact sports, road traffic accident, motor vehicle accident or during birth. Grossly, it can be divided into
Traumatic :
e.g motor vehicle accident, contact sports
Non traumatic :
e.g.obstetric palsy and Parsonage-Turner Syndrome
The network of nerves is fragile and can be damaged by stretching, pressure or cutting.
Stretching can occur when the head and neck are forced away from the shoulder, such as might happen in a fall from a motorcycle. If severe enough, the nerves can actually avulse, or tear out of their roots in the neck.
Pressure could occur from crushing of the brachial plexus between the collarbone and first rib, or swelling in this area from injured muscles or other structures.
The former examples of events are caused by one of two mechanisms that remain constant during the injury. The two mechanisms that can occur are traction and heavy impact.
These two methods disturb the nerves of the brachial plexus and cause the injury.
Traction:
Traction, also known as stretch injury, is one of the mechanisms that cause brachial plexus injury.
The nerves of the brachial plexus are damaged due to the forced pull by the widening of the shoulder and neck.
Traction occurs from severe movement and causes a pull or tension among the nerves.
There are two types of traction: downward traction and upward traction.
In downward traction there is tension of the arm which forces the angle of the neck and shoulder to become broader.
This tension is forced and can cause lesions of the upper roots and trunk of the nerves of the brachial plexus.
Upward traction also results in the broadening of the angle between the arm and chest as occurs when the arm and shoulder are forced upward, this time the nerves of T1 and C8 are torn away.
Impact :
Heavy impact to the shoulder is the second common mechanism to causing injury to the brachial plexus.
Depending on the severity of the impact, lesions can occur at all nerves in the brachial plexus.
The location of impact also affects the severity of the injury and depending on the location the nerves of the brachial plexus may be ruptured or avulsed.
Some forms of impact that affect the injury to the brachial plexus are shoulder dislocation, clavicle fractures, hyperextension of the arm and sometimes delivery at birth.
During the delivery of a baby, the shoulder of the baby may graze against the pelvic bone of the mother. During this process, the brachial plexus can receive damage resulting in injury.
This is very low compared to the other identified brachial plexus injuries.
SYMPTOMS:
Avulsion, stretch and rupture types of nerve injuries
Signs and symptoms of a brachial plexus injury can vary greatly, depending on the severity and location of your injury. Usually only one arm is affected.
Less severe injuries :
Minor damage often occurs during contact sports, such as football or wrestling, when the brachial plexus nerves get stretched or compressed.
These are called stingers or burners, and can produce the following symptoms:
- A feeling like an electric shock or a burning sensation shooting down your arm
- Numbness and weakness in your arm
- These symptoms usually last only a few seconds or minutes, but in some people the symptoms may linger for days or longer.
More-severe injuries :
More-severe symptoms result from injuries that seriously injure or even tear or rupture the nerves.
The most serious brachial plexus injury occurs when the nerve root is torn from the spinal cord.
Signs and symptoms of more-severe injuries can include:
- Weakness or inability to use certain muscles in your hand, arm or shoulder
- Complete lack of movement and feeling in your arm, including your shoulder and hand
- Severe pain
CAUSES:
Damage to the upper nerves that make up the brachial plexus tends to occur when your shoulder is forced down while your neck stretches up and away from the injured shoulder.
The lower nerves are more likely to be injured when your arm is forced above your head.
These injuries can occur in several ways, including:
Contact sports:
- Many football players experience burners or stingers, which can occur when the nerves in the brachial plexus get stretched beyond their limit during collisions with other players.
Difficult births:
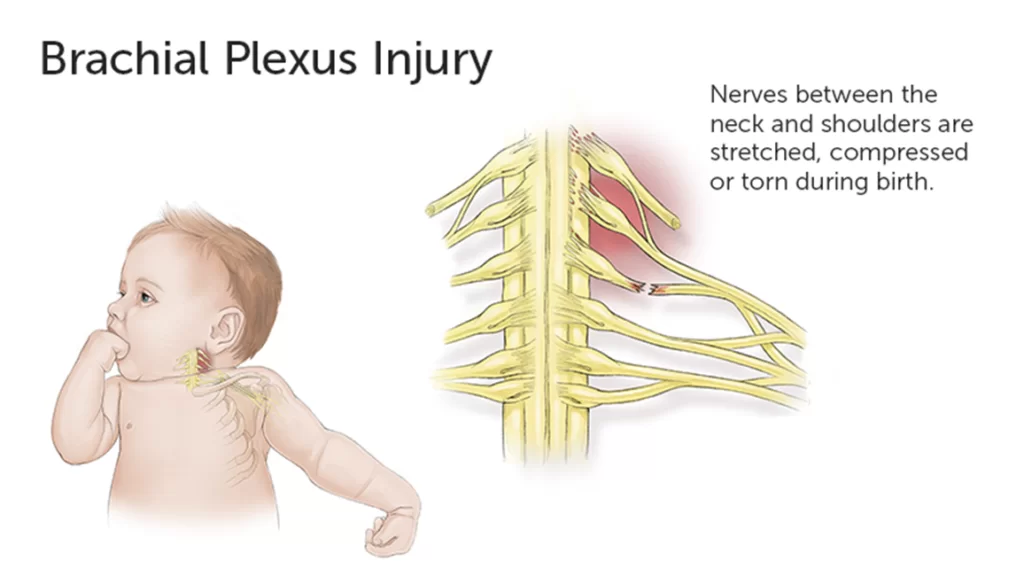
- Newborns can sustain brachial plexus injuries. These may be associated with high birth weight, breech presentation or prolonged labor.
- If an infant’s shoulders get wedged within the birth canal, there is an increased risk of a brachial plexus palsy.
- Most often, the upper nerves are injured, a condition called Erb’s palsy.
Trauma:
Several types of trauma:
Including motor vehicle accidents, motorcycle accidents, falls or bullet wounds — can result in brachial plexus injuries.
Tumors and cancer treatments:
Tumors can grow in or along the brachial plexus, or put pressure on the brachial plexus or spread to the nerves. Radiation treatments to the chest may cause damage to the brachial plexus.
Risk factors :
Participating in contact sports, particularly football and wrestling, or being involved in high-speed motor-vehicle accidents increases your risk of brachial plexus injury.
Complications:
Given enough time, many brachial plexus injuries in both children and adults heal with little if any lasting damage.
But some injuries can cause temporary or permanent problems, such as:
Stiff joints:
If you experience paralysis of your hand or arm, your joints can stiffen. This can make movement difficult, even if you eventually regain use of your limb.
For that reason, your doctor is likely to recommend ongoing physical therapy during your recovery.
Pain: This results from nerve damage and may become chronic.
Numbness: If you lose feeling in your arm or hand, you run the risk of burning or injuring yourself without knowing it.
Muscle atrophy: Nerves regrow slowly and can take several years to heal after injury. During that time, lack of use may cause the affected muscles to break down.
Permanent disability : How well you recover from a serious brachial plexus injury depends on a number of factors, including your age and the type, location and severity of the injury.
Even with surgery, some people experience permanent muscle weakness or paralysis.
Classification of injuries:
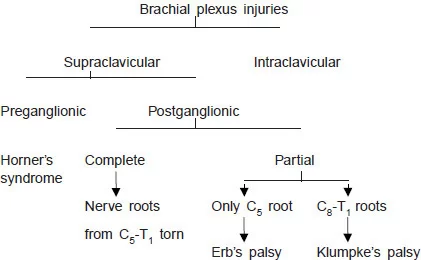
The various classifications of brachial plexus injury are as follows:
- Leffert classification of brachial plexus injury (It is based on etiology and level of injury and is as follows)
- I Open (usually from stabbing)
- II Closed (usually from motorcycle accident)
- IIa Supraclavicular
Preganglionic:
- Avulsion of nerve roots, usually from high speed injuries with other injuries and LOC
- No proximal stump, no neuroma formation (neg Tinel’s)
- Pseudomeningocele, denervation of neck muscles are common
- Horner’s sign (ptosis, miosis, anhydrosis)
Postgangionic:
- Roots remain intact
- Usually from traction injuries
- There are proximal stump and neuroma formation (pos Tinel’s)
- Deep dorsal neck muscles are intact, and pseudomeningoceles will not develop
Infraclavicular lesion:
Usually involves branches from the trunks (supraclavicular) :
Function is affected based on trunk involved
- III Radiation induced
- IV Obstetric
- IVa Erb’s (upper root) – waiter’s tip hand;
- IVb Klumpke (lower root)
Millesi classification of brachial plexus injury:
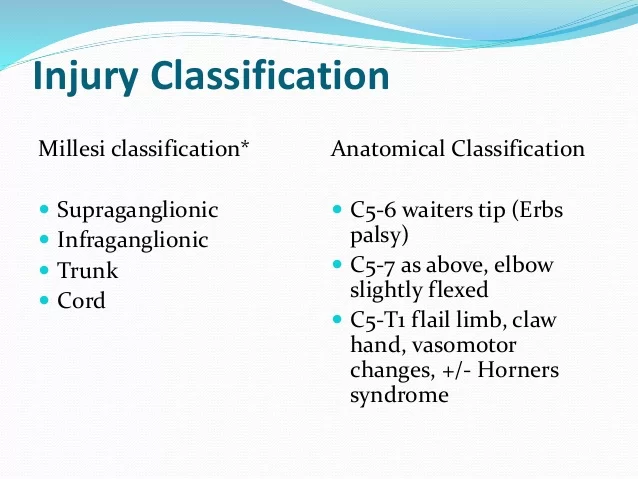
- I: supraganglionic/preganglionic
- II: infraganglionic/postganglionic
- III: trunk
- IV: cord
Classification on anatomical location of injury :
- Upper plexus palsy (Erb’s palsy in the OBPI cases) involves C5-C6+/-C7roots.
- Lower plexus palsy (Klumpke’s palsy) involves C8-T1 roots (and sometimes also C7)
- Total plexus lesions involve all nerve roots C5-T1
- An intermediate type that primarily involves the C7 root.
INJURIES:
Erb’s Paralysis:

Site of injury:
The region of the upper trunk of the brachial plexus is called Erb’s point. Six nerves meet here. Injury to the upper trunk causes Erb’s Paralysis.
Causes of injury:
- Undue separation of the head from the shoulder, which is commonly encountered in
- Birth injury
- Fall on shoulder
- During anaesthesia
- Nerve roots involved:
- Nerve roots involved :
- Mainly C5
- Partly C6.
Muscles paralysed:
- Mainly: biceps, deltoid, brachialis and brachioradialis.
- Partly: supraspinatus, infraspinatus and supinator
Deformity:
- Arm: Hangs by the side, adducted and medially rotated
- Forearm: Extended and pronated
- The deformity is known as “Policeman’s tip hand” or “Porter’s tip hand”.
Disability:
- Abduction and lateral rotation of the arm (shoulder).
- Flexion and supination of forearm.
- Biceps and supinator jerks are lost.
- Sensations are lost over a small area over the lower part of the deltoid.
Klumpke’s Paralysis:
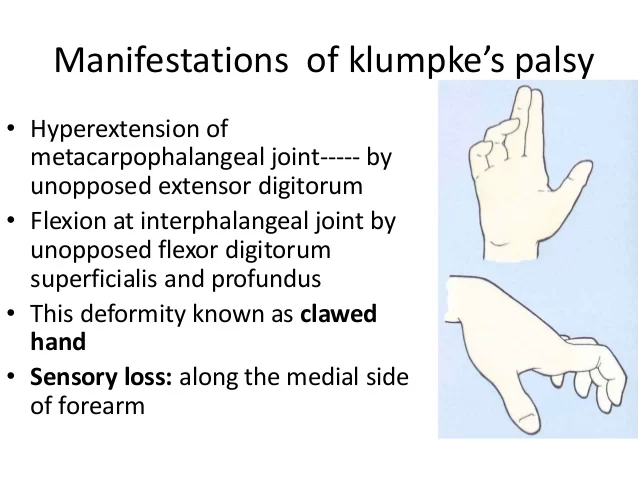
Site of injury: Lower trunk of the brachial plexus.
Cause of injury: Undue abduction of the arm, as in clutching a tree branch with the hand during a fall from a height, or sometimes in birth injury.
- Nerve roots involved:
- Mainly T1
- Partly C8
Muscles paralysed:
- Intrinsic muscles of the hand (T1)
- Ulnar flexors of the wrist and fingers (C8).
Deformity:
(position of the hand) claw hand due to the unopposed action of the long flexors and extensors of the fingers.
In a claw hand there is hyperextension at the metacarpophalangeal joints and flexion at the interphalangeal joints.
Disability:
Claw hand
Cutaneous anaesthesia and analgesia in a narrow zone along the ulnar border of the forearm and hand.
Horner’s syndrome :
Ptosis, miosis, anhydrosis, enophthalmos and loss of ciliospinal reflex- may be associated.
This is because of injury to sympathetic fibres to the head and neck that leave the spinal cord through nerve T1.
Vasomotor changes:
The skin areas with sensory loss is warner due to arteriolar dilation. it is also drier due to the absence of sweating as there is loss of sympathetic activity.
Tropic changes:
Long standing case of paralysis leads to dry and scaly skin.The nails crack easily with atrophy of the pulp of fingers.
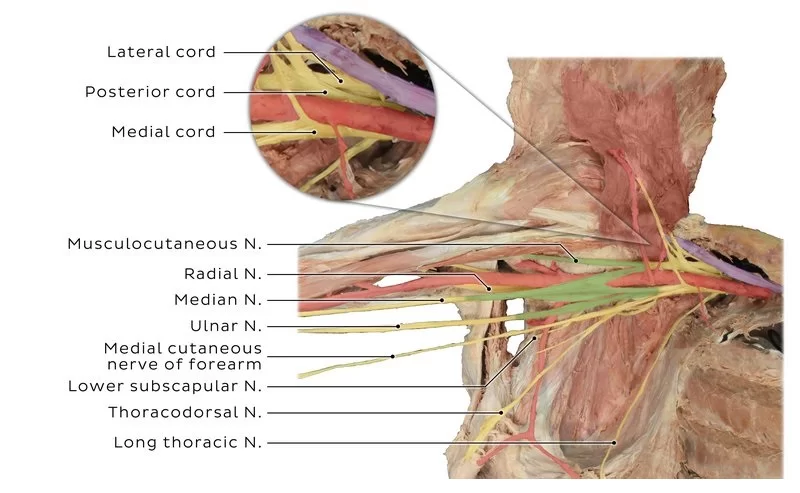
Injury to lateral cord:
- Cause: Dislocation of humerus associated with others
- Nerve involved: musculocutaneous, lateral root of median.
Muscles paralysed:
- Biceps
- Coracobrachialis
- All muscles supplied by the median nerve, except those of hand.
Deformity and disability:
- Midprone forearm
- Loss of flexion of forearm
- Loss of flexion of the wrist
- Sensory loss on the radial side of the forearm
- Vasomotor and trophic changes
Injury to medial cord:
- Cause: Subcoracoid dislocation of humerus
- Nerves involved: Ulnar, Medial root of median
Muscles paralysed:
- Muscles supplied bye ulnar nerve
- Five muscles of the hand supplied bye the median nerve.
Deformity and disability :
Claw hand
- Sensory loss on the ulnar side of the forearm and hand
- Vasomotor and tropic changes as a bone
Diagnosis:
- The most accurate test for diagnosing a brachial plexus injury is operative exploration of the potentially injured segments from the spinal roots to end-organs.
- Nerves should be evaluated under an operative microscope, with or without intraoperative electrical studies (e.g. bipolar stimulation, SEPs or MEPs) to supplement.
- Operative evaluation of the rootlets within the spinal canal and intraforaminal portion of the spinal roots proximal to the dorsal root ganglia (e.g. via hemilamiinectomy or otherwise) is difficult and rarely clinically justifiable, so in the context of an apparently in-continuity root, preoperative imaging studies are the only method of evaluating this section of nerve.
- The best non-invasive test for BPI is magnetic resonance imaging (MRI). MRI aids in the assessment of the injuries and is used to provide information on the portion of the plexus which cannot be operatively explored (the rootlets and roots).
- In addition, assessment of the cervical cord, post-traumatic changes in soft tissues and associated injuries (e.g. fractures, cuff tears, etc) may be appreciated.
- Although superior to nerve conduction studies, ultrasound and other tests, conventional MRI has a poor specificity (72%) meaning that the false-positive rate is high and surgeons can’t rely upon the test to guide treatment.
- Consequently, the future of peripheral nerve MR imaging (including imaging brachial plexus injuries) is likely to be based on diffusion-weighted imaging, such as diffusion tensor techniques.
- Which are of significant potential clinical utility and can enable the production of easily-interpreted 3D reconstructions of the spinal cord and brachial plexus such as this.
- Several weeks/months after BPI, EMG examination can provide additional information about whether the muscle is denervated.
- These examinations are painful, highly user-dependent and lack normal values so cannot be relied upon.
Physiotherapy treatment in Brachial Plexus injury:
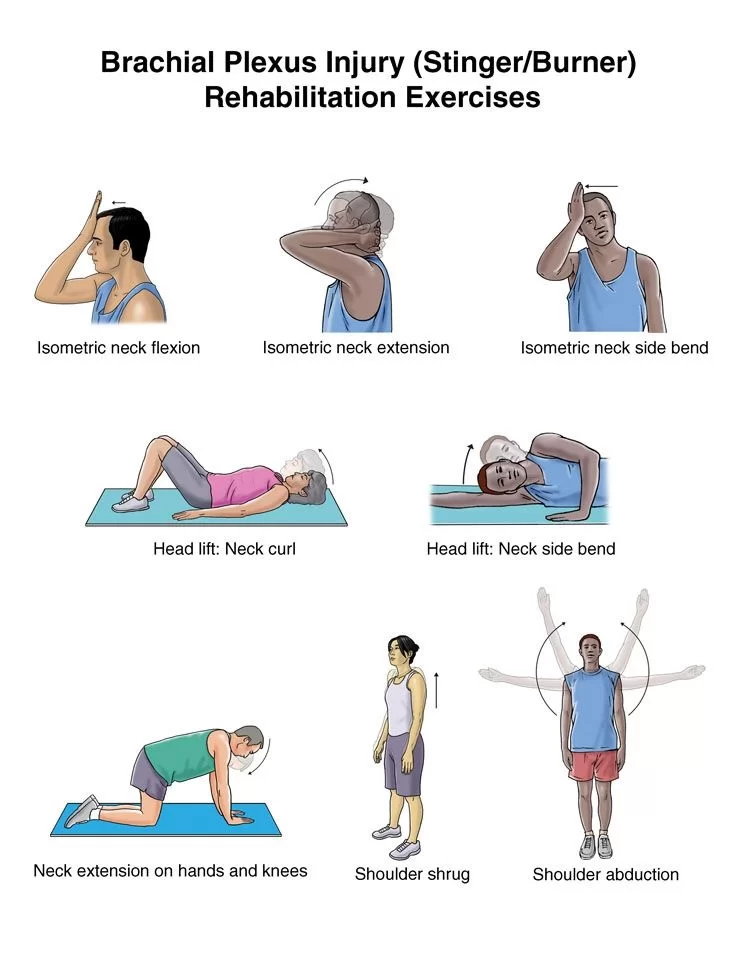
Physiotherapy treatment for BP injury varies significantly according to the type and severity of the injury.
In mild cases physiotherapy and rehabilitation will assist recovery, in more severe cases surgery and bracing may be needed.
Always the goal stays constant ie to return to previous level of function and preventing potential disability.
Physiotherapy treatment aims:
- Development of strength, flexibility, stamina and co-ordination
- Maintaining ROM via passive movements, exercise therapy, splinting and positioning and protection of denervated dermatomes.
- Functional training and adoption adaptive devices if needed.
- Pain control via acupuncture and TENS
- Managing chronic oedema via education, compression garments and massage therapy.




My friends Have Brachial plexus injury and taken Physiotherapy treatment for nearly 10 month long, now he is completely recover!