Calcaneal Fracture
Introduction
A calcaneal fracture refers to a break or cracks in the heel bone, known as the calcaneus. The calcaneus is the largest bone in the foot and plays a crucial role in weight-bearing and walking.
Calcaneal fractures often result from high-energy injuries, such as falls from heights or automobile accidents, and can cause significant pain, swelling, and difficulty in walking.
Epidemiology
- Accounts for 60-75% of all major tarsal bone fractures
- The most common fracture of the tarsals
- Bimodal distribution – most commonly affects males aged 20-29 (high energy trauma) or elderly women over 60 (low energy trauma, osteoporosis)
- Annual incidence estimated at 10.3 per 100,000
- Economic impact: Calcaneal fractures carry a high economic burden given the associated treatment costs and time off work during recovery
- Etiology: Most commonly caused by a fall from height or motor vehicle accidents, resulting in an axial compressive load on the heel
Mechanism of Injury / Pathological Process
- The majority of calcaneal fractures are caused by high-energy events that cause the bone to be loaded axially.
- The talus working as a wedge induces depression, which flattens, widens, and shortens the calcaneal body. Common sources of injury include falls from heights and automotive accidents (a foot compressed against an accelerator, stop, or floorboard).
- In less serious incidents, such as an ankle sprain or a stress fracture in a runner, calcaneal fractures can also happen.
- A calcaneus fracture can also result from jumping onto hard surfaces, blunt or penetrating trauma, and twisting or shearing incidents.
- Most injuries happen one after the other. Lower limb (13.2%) and spinal (6.3%) injuries are the most common concurrent injuries.
- Because the sustentaculum tali protects the posterior tibial neurovascular bundle, neurovascular injuries associated with calcaneal fractures are rare. The neurovascular bundle extends along the medial portion of the calcaneal body.
Anatomy & Biomechanics
Anatomic Features
Location: posterosuperior aspect of the foot; forms the bony prominence of the heel
Articulations:
- Superiorly: articulates with the talus in the subtalar joint
- Anteriorly: articulates with the cuboid bone
- Posteriorly: provides insertion for the Achilles tendon
Surfaces:
- Superior surface: covered with articular cartilage for the subtalar joint. Anterior, middle, and posterior facets articulate separately with the talus
- Inferior surface: largely occupied by the fat pad of the heel
Processes:
- Sustentaculum tali: projects medially; supports the head of the talus
- Anterior process: forms the forefoot articulation with the cuboid
- Posterior tuberosity: projects posteriorly; serves as the insertion point for the Achilles tendon
Biomechanical Function
- Shock absorption: disperses significant compressive loads during heel strike while walking
- Lever arm: extends the moment arm for inversion/eversion by the pull of muscles on the Achilles tendon insertion
- Stability: Forms a stable, rigid lever for propulsion at the terminal stance phase of gait
- Weight-bearing: bears total body weight with the talus during the stance phase
- Muscle function: allows major muscles like the calves and foot intrinsics to act effectively on the ankle and foot skeleton
In summary, the calcaneus plays integral biomechanical roles in stabilizing the foot and ankle, enabling locomotion, and supporting our body weight. Fractures severely impair these functions.
Types of Calcaneus Fractures
Intra-articular
- The fracture line extends into the posterior subtalar joint surface
- Involves one or more of the joint facets that articulate with the talus bone – posterior, middle, and anterior
- Leads to joint incongruity after fracture
- At higher risk of developing post-traumatic arthritis
- Generally more difficult to accurately reduce and fixate
- Require anatomic joint reconstruction to restore biomechanics
Extra-articular
- The fracture line does not extend into the subtalar joint surface
- The articular surface remains intact
- Considered more stable injuries
- Minimally invasive fixation techniques can be used
- Rarely leads to joint arthritis
Displaced
- The main fracture fragments are significantly separated – more than 2 mm displacement
- Loss of anatomical alignment
- -require open reduction and internal fixation to restore congruent joint surfaces and alignment
Non-displaced
- The main fracture line is visible but the fragments maintain alignment within acceptable limits
- Can often be managed non-operatively with good functional outcomes
Tongue Type Fracture
- Primarily an intra-articular fracture pattern
- The primary fracture line splits the posterior facet from front to back
- This fragment is markedly depressed, taking the shape of a ‘tongue’ impressed into the calcaneal body
- High risk of sub-fibular impingement if the depressed fragment is not elevated adequately
- Sanders type II fracture
Joint Depression Fractures
- The subtalar joint surface is fragmented and axially loaded, resulting in a compression-type injury
- The articular surface collapses upon itself in a confused, non-anatomic position
- Significant cartilage injury that predisposes to arthritis
- Difficult to reconstruct due to small comminuted articular fragments
- Also called compression fractures or Sanders type III fractures
Comminuted Fractures
- The calcaneus is shattered into more than three distinct fragments
- Typically follow high-energy axial trauma such as falls from height
- The smaller pieces may come from the tuberosity, the sustentaculum tali, the body or be dispersed intra-articular fragments
- Very difficult to perfectly reduce and fixate all pieces anatomically
- Prone to loss of reduction post-fixation and may require bone graft
- Associated with the worst long-term outcomes
Signs and Symptoms of Calcaneal Fracture
Pain
- Typically severe pain in the hindfoot/ankle after an injury
- The patient is not able to bear weight due to pain.
- Local swelling and tenderness over the heel area
- Pain worsens with ankle motion or walking
Bruising and Swelling
- Rapid onset of bruising and swelling around the hindfoot and ankle
- Tense edema develops along the lateral ankle and hindfoot
- The posterior heel fat pad is obliterated
Deformity
- Loss of the normal shape of the heel/hindfoot
- Widening of the heel due to displacement of fracture fragments
- The Achilles tendon may bow out laterally if the tuberosity fragment is displaced
Inability to Weight Bear
- Patients are unable to bear weight due to intense pain
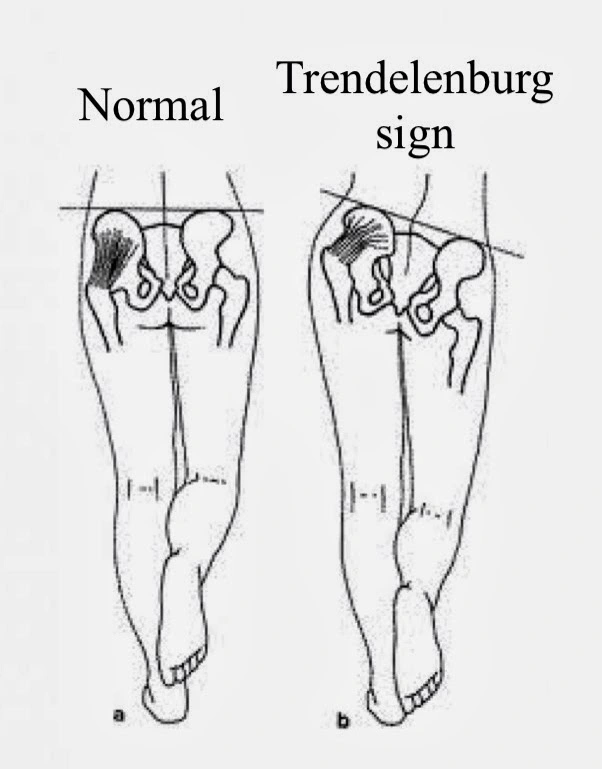
- May walk with a significant limp if partial weight-bearing
Numbness
- Numbness along the lateral heel, foot, and toes may indicate Sural nerve injury
- Up to 25% of fractures are associated with sural nerve injury
Crepitus
- A crunching or grinding sensation may be felt when pressing along the fracture due to bone fragments rubbing together
Early recognition based on these signs/symptoms along with radiographic confirmation is important for prompt management. Complications like arthritis, stiffness, chronic pain, and nerve injury can result if not well treated.
Diagnosis
History:
- Acute trauma – fall from height, motor vehicle accident
- Severe hindfoot pain and swelling, unable to bear weight
Physical Exam:
- Tense swelling, and bruising around the hindfoot & lateral ankle
- Tenderness directly over the calcaneus
- Abnormal widening of heel contour
- Pain with hindfoot motion
- The heel fat pad may be flattened or bulbous
Imaging:
- X-ray – Initial standard views (lateral, axial calcaneal, Broden’s)
- CT Scan – Confirms fracture pattern, displacement, joint involvement
- Allows classification – Essex-Lopresti, Sanders classifications
Additional imaging/testing:
- MRI if osteomyelitis or bone marrow edema suspected
- Compartment pressure testing if compartment syndrome concerns
In the radiographic images, some examples of the reference angle and sign are:
- A hematoma found on CT scans of the sole that is thought to be pathognomic for calcaneal fractures is known as Mondor’s Sign.
- The angle between two lines drawn on plain film—one between the highest point on the tuberosity and the highest point of the posterior facet, and the other between the highest point on the anterior process and the highest point on the posterior facet—is known as Bohler’s Angle, and its normal range is 20 to 40 degrees. If the fracture is a calcaneus, the angle may be depressed on plain radiographs.
- The angle between two lines drawn on plain film, one along the calcaneus’s anterior downward slope and the other along its superior upward slope, is known as the Critical Angle of Gissane. A typical angle is between 130 and 145 degrees, and it may indicate a higher risk of calcaneus fracture.
Treatment of Calcaneal Fracture
Nonoperative Treatment
Indications:
- Nondisplaced extra-articular fractures
- Minimally displaced (less than 2mm) tongue-type fractures
- Low-demand elderly patients with osteoporotic fractures
Protocol:
- Short leg non-weight-bearing cast or splint for 6-12 weeks
- The cast held in slight Equinus to maintain fracture reduction
- Strict non-weight-bearing restrictions during the entire casting period
- Serial X-rays are done every 2 weeks to monitor the maintenance of the fracture position
- CT scan pre-cast removal to confirm early consolidation before weight-bearing
- Gradual return to protected weight bearing in a walking boot over 4-6 weeks
Considerations:
- Must be very compliant and reliable with non-weight-bearing precautions
- Higher re-displacement rates compared to surgery
- Residual stiffness and loss of hindfoot motion common
Surgical Treatment
Goals of surgery:
- Anatomically reduce the joint surface to prevent arthritis
- Stably fix fragments with rigid fixation to enable early motion and rehabilitation
- Bone graft defects to stimulate union
Surgical approach:
- Extensive lateral approach is most commonly used
- Extended osteotomies of fibula and calcaneal tuberosity routinely performed for maximal exposure
- The sinus tarsi approach can be used for tongue-type fractures
- Percutaneous fixation growing as a less invasive option
Fixation methods:
- Plates and screw constructs provide rigid stabilization
- No superior implant established; surgeon preference and skills vital
- External fixation is rarely used as the final treatment.
- K-wires and Steinmann pins for percutaneous fixation methods
Additional considerations:
- Bone grafting supplements structural integrity in comminuted fractures
- Staged procedures may be beneficial
- Second look surgery to remove prominent hardware once fracture shows signs of consolidation
The decision for operative vs non-operative treatment is multi-factorial – fracture pattern being the most critical guide. A coordinated team approach with experienced foot and ankle surgeons generally leads to the best outcomes.
Physical Therapy Management
Physical therapy management of calcaneal fractures can be similar between nonoperative and operative methods. These methods include joint mobilization, range of motion exercises, pain management, strengthening, proprioception training, gait training, plyometrics, and gradual loading to return to more demanding activities.
Pre-Surgery
Open reduction internal fixation of intraarticular calcaneal fractures requires initial stability.
Preoperative revalidation consists of the following:
- Giving instructions on how to use a wheelchair, bed transfers, or crutch walking;
- Immediate elevation of the injured foot to decrease swelling;
- Compression utilizing a foot pump, intermittent compression devices, or compression wraps as tolerated.
Post-Surgery
Traditional immobilization protocols of both nonoperative and postoperative management of calcaneal fractures are included in the progression below, as are phases II and III of traditional and early motion rehabilitation protocols following nonoperative or postoperative care. The traditional immobilization protocols of nonoperative and postoperative management are similar and are thus combined in the progression below.
Pain Management
You will have some pain following surgery; this is a normal part of the healing process, and your physician and nurses will make every effort to minimize your pain to expedite your recovery. Your doctor may prescribe a combination of these medications that will improve pain relief while minimizing the need for opioids.
Opioid addiction and overdose have become major public health concerns in the US. It is critical to take opioids only as prescribed by your doctor and to discontinue them as soon as your pain begins to improve.
Consult your doctor if your pain has not improved within a few days of surgery. Be aware that, while opioids can help reduce pain after surgery, they are narcotics and can become addictive.
Early Phase (0-6 weeks)
Goals:
- Maintain ankle and foot mobility
- Control swelling and pain
- Prevent complications like stiffness, skin issues
Interventions:
- Strict non-weight-bearing precautions
- Elevation of the leg to aid edema drainage
- Active and passive ankle range of motion exercises
- Gentle foot and toe range of motion exercises
- Modalities like ice, and contrast baths for pain and swelling
- Bracing initially to protect fracture fixation
Late Phase (6 weeks onwards)
Goals:
- Regain strength and mobility
- Progress weight-bearing smoothly
- Work on balance and proprioception
Interventions:
- Wean off of walking boot into regular shoe wear
- Gradually progress weight-bearing over 4-6 weeks under guidance
- Increase focus on ankle plantarflexion and foot intrinsic exercises
- Manual joint mobilizations to regain hindfoot mobility
- Balance and proprioceptive training
- Impact and plyometric training around 4-5 months
Complications associated with calcaneus fractures:
Malunion
- Improper healing of fracture fragments in an abnormal position
- Causes chronic pain, stiffness, abnormal gait
- Requires corrective osteotomy/fusion
Nonunion
- Lack of bony consolidation >6 months post-injury
- More common with open fractures or highly comminuted fractures
- Repeat surgery needed – bone grafting with internal fixation
Post-traumatic Arthritis
- Secondary osteoarthritis of subtalar joint surfaces
- Caused by intra-articular cartilage damage, incongruity
- Pain, stiffness, and loss of hindfoot motion
- Usually requires arthrodesis at some point
Loss of Reduction
- Replacement after closed reduction or open surgery
- Related to inadequate fixation, early weight-bearing
- Requires return to ORIF ± bone grafting
Infection
- Superficial soft tissue infection or osteomyelitis
- Wound necrosis with hardware exposure
- Difficult to treat with implanted hardware
- Serial debridement, antibiotics, device removal
Compartment Syndrome
- Elevated foot pressures cause ischemic muscle necrosis
- Extremely painful, requires emergent release
- At risk of loss of limb viability
Reflex Sympathetic Dystrophy
- Complex pain syndrome linked to sympathetic response
- Severe hindfoot pain, hypersensitivity, trophic changes
- Very difficult to treat, rehabilitation challenging
Sural Nerve Injury
- Up to 25% of fractures get Sural nerve injury
- Causes numbness along the lateral foot
With the many complications, outcomes are very surgeon and fracture-pattern-dependent. However, with modern treatment algorithms, more reliable improvements are being attained.
Outcomes & Prognosis
Depends significantly on the initial fracture pattern and adequacy of the reduction
Positive Prognostic Factors:
- Non-displaced fractures
- Extra-articular fracturesAnatomic reductions restoring articular congruity
- Appropriate bone grafting of defects
Negative Prognostic Factors:
- Comminuted, intra-articular injuries
- Advanced patient age, osteoporosisSmoking, diabetes, and other comorbidities
- Inadequate surgical reduction
General guidelines on return to normal function:
- Nonoperative: 3-6 months protected weight bearingORIF: 4-6 months protected weight bearing
- Secondary arthrodesis: 9-12 months for complete recovery
With optimum treatment, most patients regain good functionality. However, long-term arthritis is not uncommon and remains difficult to avoid in some fracture patterns.
Prevention
Key strategies:
- Preventing falls among the elderly via safety measures at home
- Avoiding risky behavior that could lead to high-energy traumaWearing protective gear during sports or manual labor jobsMaintaining bone density with nutrition, weight-bearing activity
- Managing medical issues like osteoporosis, diabetes
With focused rehab and preventative steps, patient outcomes can be greatly optimized following these difficult injuries.
Summary
A calcaneus fracture is a break in the heel bone, which is the largest bone in the foot. It accounts for 60-75% of major foot fractures with an annual incidence of 10.3 per 100,000. Falls and vehicle accidents are common causes. These fractures can be intra or extra-articular, displaced, or nondisplaced in varying patterns like tongue-type and comminuted. Signs include pain, swelling, bruising, and deformity of the heel. X-ray and CT confirm the diagnosis and pattern.
Treatment options for calcaneus fractures range from casting and non-weight-bearing to various surgical fixation and bone grafting techniques. Rehabilitation progresses weight-bearing and strength over months. Complications like arthritis, chronic pain, and nerve issues can occur. However, outcomes continue to improve with anatomical reconstruction approaches when needed. Prevention revolves around fall precautions and safety measures.
FAQs
How is a calcaneus fracture diagnosed?
Calcaneus fractures are diagnosed based on clinical signs like heel pain/swelling and X-rays showing the fracture line. CT scans further characterize the fracture pattern and joint surface involvement.
What are the treatment options for a displaced intra-articular calcaneus fracture?
The standard treatment is open reduction and internal fixation (ORIF) surgery using plates and screws to restore the joint anatomy, followed by bone grafting defects and gradual rehabilitation with protected weight-bearing over months.
What are the treatment options for a displaced intra-articular calcaneus fracture?
Following ORIF surgery, patients will require approximately 12 weeks of non-weight-bearing and 12 additional weeks of progressive, protected weight-bearing. Complete recovery can take over 6 months.
What can prevent future calcaneus fractures?
Preventing falls, wearing appropriate footwear during work/sports, maintaining bone density, and managing conditions like osteoporosis are key prevention strategies to protect the heel bone as we age.
Does a calcaneus fracture lead to arthritis?
It depends on factors like fracture displacement and accuracy of reduction. However post-traumatic arthritis is fairly common following these injuries, ultimately requiring arthrodesis (fusion) later in life in some cases.
REFERENCES
- Calcaneal Fractures. (n.d.). Physiopedia. https://www.physio-pedia.com/Calcaneal_Fractures
- Calcaneus (Heel Bone) Fractures – OrthoInfo – AAOS. (n.d.). https://orthoinfo.aaos.org/en/diseases–conditions/calcaneus-heel-bone-fractures/
- Cluett, J. (2022, April 25). A Calcaneus Fracture Is a Broken Heel Bone. Verywell Health. https://www.verywellhealth.com/calcaneus-fracture-2549435