Patellar Instability
Introduction
Patellar instability, also known as patellar dislocation, is a condition characterized by the displacement of the patella (kneecap) from its normal position within the femoral groove. It typically occurs when the patella is forced out of alignment during movement or injury, leading to pain, instability, and difficulty in walking or bearing weight on the affected leg.
A dislocated knee can be caused by an unsteady kneecap. Leg braces and physical therapy both have benefits. Chronic (ongoing) patellar instability affects some people. ACL tears, dislocations, and knee arthritis are all made more likely by this condition.
What is Patellar Instability?
Tendons connect the patella (kneecap) to the femur (thigh bone) and tibia (shin bone). The patella moves up and down in the trochlear groove at the end of the femur when the knee bends and straightens.
When the kneecap shifts out of this groove, patellar instability results.
Two variations of patellar instability exist. Traumatic patellar dislocation is the term for the first condition. The most frequent cause of this is a knee injury. The patella is entirely pushed out of the groove during a patellar dislocation. Chronic patellar instability is the name for the other type of instability. The kneecap only typically slides partially out of the groove in this type. An example of a subluxation is this.
What is the connection between a dislocated kneecap and patellar instability?
Kneecap dislocation can result from patellar instability. You might have Complete dislocation: The kneecap is lost when the ligaments holding it in place slide to the outside of the knee. Ligaments could be torn or stretched. The kneecap is completely misaligned.
A partial dislocation (subluxation) occurs when the kneecap comes loose from its groove.
How common is Patellar instability?
Your knees are constantly in use throughout the day. They become more vulnerable to issues like patellar instability as a result. According to experts, 50 to 77 Americans out of 1 lakh have some form of patellar instability.
Epidemiology
For 3% of all knee injuries, patella dislocation occurs. Young people are most frequently affected by pathology and injuries. Patients with patellar instability tend to be female and between the ages of 10 and 16 in general. Patellar instability occurs in 5.8 out of every 100,000 people in the general population and 29 out of every 100,000 people aged 10 to 17 years old.
Many first-time dislocations without loose bodies or articular injury respond well to conservative therapy.. But after receiving conservative treatment, the recurrence rate can range from 15 to 44%. Recurrent dislocation episodes are 50% more likely to occur in patients who have had two or more prior dislocations.
The greatest risk of long-term patellar instability is linked to a history of patellar dislocation. The recurrence rates are even higher in patients who have a known medial patellofemoral ligament (MPFL) injury that has been verified on MRI. First-time dislocators may continue to experience pain, functional restrictions, and instability due to these recurrence rates.
Patellar instability can be summed up as follows, and each component will be covered in more detail below:
Young patients (10 to 17 years old)
Acute traumatic episode
Chronic Catholicity – Ehlers-Danlos syndrome
Bony misalignment- including pronated feet, external tibial torsion, and genu valgum. The three bony misalignments collectively known as “Miserable Malalignment Syndrome” result in a greater Q angle.
Anatomical pathology – trochlear dysplasia
Long-term arthritis, functional decline, and eventual progression to pain.
Classification
Patellofemoral instability is classified descriptively. These classifications are listed below:
Acute (first dislocation)
Subluxation or dislocation
Traumatic
Patellar instability
Recurrent
Involuntary dislocation of the patella due to habitual dislocation
Passive patellar dislocation with the aid of apprehension test
Patellar dislocation that is syndromic, or connected to a syndrome, connective tissue condition, or neuromuscular disorder
Mechanism
A direct blow, a knee-to-knee collision, or a helmet to the side of the knee injury can all result in traumatic mechanisms. non-contact twisting injury with the foot externally rotated and the knee extended.
What causes Patellar instability?
The skeletal system includes the kneecap. The front of the thighbone’s (femur) connective tissue, muscles, tendons, and ligaments—cross the kneecap and attach to the shinbone (tibia). When your leg is straight, these muscles pull the kneecap through the trochlear groove, and when your leg is bent, they pull the kneecap downward. The kneecap moves outside of this groove when it is shaky.
Causes of patellar instability include
A trochlear groove that is shallow or uneven.
joints with loose ligaments or that are very flexible.
During a fall, sports injury, or other accident, the kneecap receives a sharp blow.
What are the risk factors for Patellar instability?
Patellar instability can occur in anybody. Women are more prone to patellar instability because they typically have looser ligaments.
Playing high-impact sports like football or engaging in fast-paced activities like basketball, cheerleading, or soccer may put you at an increased risk.
Patellar instability can be exacerbated by loose connective tissue that is brought on by specific medical conditions. These consist of:
Cerebral palsy.
Down syndrome.
Ehlers-Danlos syndrome.
Signs and symptoms of Patellar instability
Your child may feel discomfort, stiffness, difficulty using the injured limb when walking, and/or buckling, catching, or locking in the knee. Last but not least, the affected knee may also have a noticeable deformity.
The majority of patients report feeling as though their kneecap has moved or shifted. Normally, the kneecap will reposition itself, but on occasion, surgery in the emergency room may be required.
The pain from chronic patellar subluxations might not be as bad as it would be from a traumatic injury.
Patients may experience pain below the kneecap, especially when engaging in deep knee-bending activities.
How is Patellar instability diagnosed?
Even if your kneecap returns to its normal position on its own, you should still see your doctor for a diagnosis and possible treatments. To evaluate your symptoms, including your range of motion, your doctor will conduct a physical examination.
Other options include:
X-rays to look for broken bones and determine whether the kneecap is misaligned.
MRI to look for fractures, meniscal tears, and injuries to the anterior cruciate ligament (ACL).
Treatment
The treatment approach for patellar instability depends on various factors, such as the severity of the dislocation, the presence of structural abnormalities, and the individual’s activity level.
What are the medical treatments for Patellar instability?
Consult a doctor if the kneecap doesn’t return to the trochlear groove on its own. A medical professional will carefully reposition the kneecap. The reduction can be an uncomfortable process.
Although you might be given pain medication, you shouldn’t require anesthesia.
Your doctor might advise the following for partial knee dislocations and patellar instability:
Knee brace to keep the kneecap in place and immobilize the knee. You might need to use crutches and wear a brace for several weeks.
NSAIDs, rest, elevation, and ice packs are all effective ways to reduce pain and swelling.
Physical therapy to increase the range of motion and strengthen the muscles that keep the kneecap in place.
What are surgical treatments for Patellar instability?
Your doctor might advise surgery if you have complete kneecap dislocation or persistent patellar instability. The majority of knee operations are arthroscopic. A tiny camera (arthroscope) and small incisions are used during the procedure.
You may have loose cartilage or bone fragments in your knee as a result of patellar instability brought on by an injury. They will be surgically removed by your doctor.
Surgical options include:
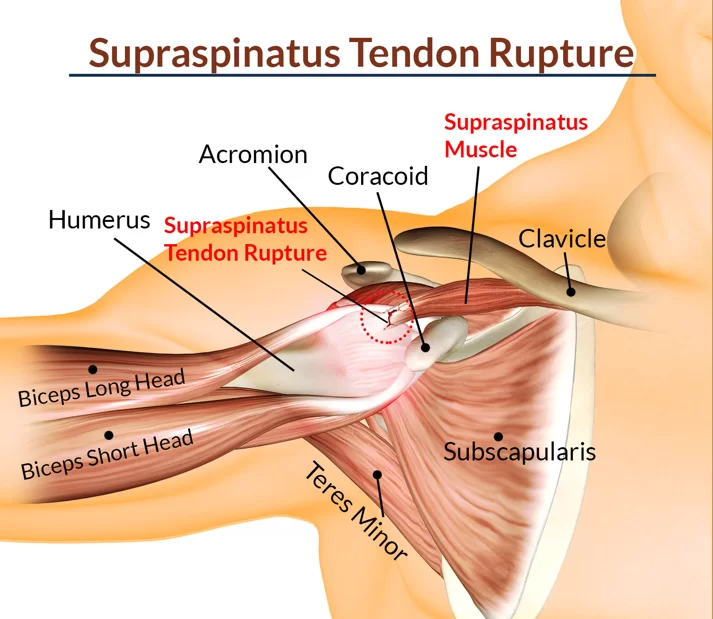
To strengthen and repair the ligaments that hold the kneecap in place, the medial patellofemoral ligament (MPFL) must be repaired.
Using a hamstring tendon from your own body or a donor, an MPFL reconstruction can repair a damaged ligament.
To realign the kneecap, connective tissues, and shinbone, a knee osteotomy (tibial tubercle transfer) is performed. Compared to arthroscopic surgery, this open surgical procedure necessitates a larger incision and a longer recovery period. severe arthritis or recurrent dislocations can be treated with a knee replacement.
Physiotherapy Treatment of Patellar Instability
Patellar instability can be effectively treated with physical therapy, which is less invasive. The goal of Treatment for Patellar instability are:
- Decreased pain
- Increased strength
- Improved knee function
- Restoration of proper movement
Best Patellar Subluxation Physical Therapy Exercises
Numerous exercises can aid in regaining your knee’s general stability.
- Quadriceps Strengthening: Strong quadriceps muscles can help stabilize the patella. Try exercises like squats, lunges, leg presses, and step-ups. Start with bodyweight or light resistance and gradually increase the intensity as tolerated.
- Hamstring Strengthening: Strong hamstrings can help balance the forces around the knee joint. Exercises like hamstring curls, deadlifts, and bridges can be beneficial. Again, start with light resistance and progress gradually.
- Vastus Medialis Oblique (VMO) Strengthening: The VMO is a part of the quadriceps muscle group and plays an important role in patellar stabilization. Exercises like terminal knee extensions and straight leg raises with a focus on activating the VMO can be helpful.
- Hip Strengthening: Strong hips can help improve overall lower limb alignment and stability. Include exercises like hip abductions, hip extensions, and lateral leg raises in your routine.
- Core Strengthening: A strong core can provide a stable base for your movements and help improve overall body mechanics. Include exercises like planks, bridges, and bird-dogs to strengthen your core muscles.
- Balance and Proprioception Training: Exercises that challenge your balance and proprioception (awareness of your body position) can improve joint stability. Examples include single-leg standing, balance board exercises, and stability ball exercises.
Remember to start with low-intensity exercises and gradually progress as your strength and stability improve. It’s important to listen to your body and avoid any exercises that cause pain or discomfort. If you experience any unusual symptoms or increased pain, stop the exercises and consult with a healthcare professional.
Exercise for Patellar Instability:
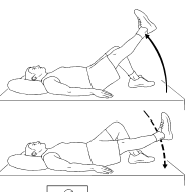
Straight Leg Raises:
Lie on your back (Supine Position) with one leg straight and the other bent. Lift the straight leg off the ground to a comfortable height, hold for a few seconds, and then lower it back down. Repeat for several repetitions on each leg. This exercise targets the quadriceps muscles.
Terminal Knee Extensions (TKE): Attach a resistance band around a sturdy object and loop it around your affected knee. Stand with the resistance band pulling the knee slightly forward. Straighten your knee against the resistance of the band, hold for a moment, and then release. Perform several repetitions on each leg.

Step-Ups: Use a step or sturdy platform that is about knee height. Step onto the platform with your affected leg, pushing through the heel, and bring your other leg up. Step back down and repeat for several repetitions. This exercise helps strengthen the quadriceps and gluteal muscles.
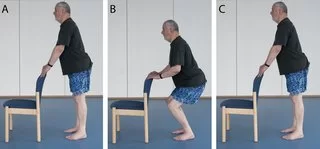
Mini Squats: Stand with your feet shoulder-width apart and slowly squat down by bending your knees, as if sitting back into a chair. Keep your weight on your heels and your knees aligned with your toes. Rise back up and repeat for several repetitions. Start with a partial squat and gradually work your way toward a deeper squat as your strength improves.

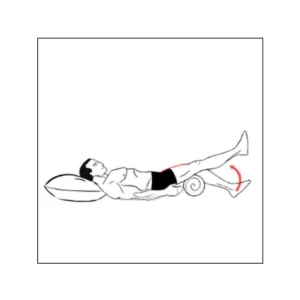
Clamshells: Lie on your side (side-lying position) with your knees bent while keeping your feet together. Now lift your top knee while keeping your feet in contact with each other. Lower it back down and repeat for several repetitions on each side. This exercise targets the hip abductors, which contribute to knee stability.

Single-Leg Balance: Stand on one leg and maintain your balance for as long as you can, aiming for 30 seconds to a minute. Once you feel comfortable, you can add difficulty by closing your eyes or performing small knee bends while balancing.

Wall Squats: start with a standing position with your back against a wall and your feet shoulder-width apart. Slowly slide down the wall by bending your knees until you reach a comfortable squat position. Hold this position for a few seconds and then push through your heels to rise back up. Repeat for several repetitions, focusing on maintaining proper alignment and keeping your knees tracking over your toes.

Hamstring Curls: Use a resistance band or a cable machine to perform hamstring curls. Attach one end of the band to a sturdy object or use the cable machine’s ankle attachment. While standing, bend your knee, bringing your heel towards your glutes against the resistance of the band or machine. Slowly release and repeat for several repetitions on each leg.
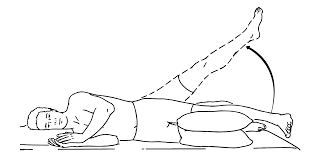
Hip Abduction: Stand with a resistance band looped around your ankles. Keeping your core engaged, lift one leg out to the side against the resistance of the band. Hold for a moment and then bring your leg back to the starting position. Perform several repetitions on each leg.

Calf Raises: Stand with your feet hip-width apart and rise up onto your toes, lifting your heels off the ground. Hold for a moment and then lower your heels back down. Repeat for several repetitions. You can perform calf raises on both feet or focus on one leg at a time for additional challenge and balance work.
How can I prevent patellar instability?
Connective tissue can be harmed by an unstable kneecap. Your risk of experiencing additional kneecap dislocations is increased by this damage.
Exercises used in physical therapy can strengthen the connective tissue and muscles that keep the kneecap in the femoral groove. Knee-strengthening exercises can also be done outside or on an exercise bike. Additionally, your doctor might advise using a knee brace while performing particular motions.
Prognosis
When non-surgical treatments for patellar instability are finished, almost half of the patients experience another knee dislocation. This indicates that the patella is still unstable.
Your risk of developing arthritis and ligament damage rises as a result of persistent patellar instability.
Surgery might be advised by your doctor.
FAQs
What is the direction of patella instability that occurs most frequently?
Because the quadriceps muscle pulls slightly laterally to the mechanical axis of the limb, patellar dislocations frequently occur in this direction.
What elements support the patella?
The lateral femoral condyle’s anterior projection and the vastus medialis’s horizontal fibres work together to stabilize the patella. The medial patellar retinaculum’s tension contributes to its stability.
How can you improve patella instability?
Slide down until your knees are bent 20 to 30 degrees while leaning against the wall. Squeeze your knees together for about 6 seconds at a time while holding a ball the size of a football between them. After a brief period of rest, squeeze once more. At least three times per day, repeat 8 to 12 times.
How serious is patellar instability?
Dislocation can harm the kneecap and the end of the thighbone whether it happens infrequently or frequently. In some cases, the injury can worsen and eventually cause arthritis in later life.



2 Comments