Central Pain Syndrome
What is Central Pain Syndrome?
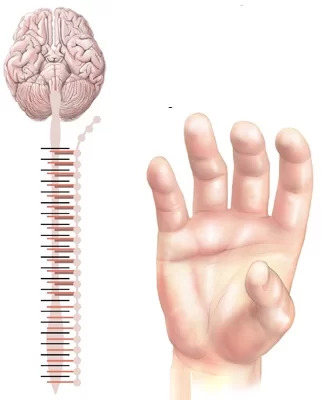
Central pain syndrome is a neurological disease caused by injury to or dysfunction of the central nervous system (CNS). The CNS contains the brainstem, brain, and spinal cord. This syndrome can be generated by:
- Stroke
- Multiple Sclerosis
- Tumors
- Epilepsy
- Brain Or Spinal Cord Trauma
- Parkinson’s Disease
The pain associated with central pain syndrome varies widely among persons partially because of the variety of potential reasons. It may involve a big part of the body or maybe more restricted to precise locations, like hands or feet. The extent of pain is generally linked to the cause of the central nervous system (CNS) injury or damage. Pain is generally constant, may be moderate to extreme in intensity, and is frequently made worse by:
- Touch
- Movement
- Emotions
- Temperature changes, generally cold
Symptoms of Central Pain Syndrome
The major symptom of Central Pain Syndrome (CPS) is pain. The pain differs significantly among people. It can be any of the observings:
- constant
- intermittent
- limited to a precise body region
- widespread throughout the body
A person generally defines pain as any of the observings:
- burning
- aching
- prickling or tingling, which is occasionally known as pins and needles
- stabbing
- itching that turns painful
- freezing
- shocking
- tearing
The pain is generally moderate to extreme. The pain may even be defined as agonizing by some people. In severe patients, a person with Central Pain Syndrome (CPS) may have pain even when touched lightly by blankets, clothing, or strong wind.
A combination of factors may cause the pain to worsen. These factors contain the following:
- touch
- stress
- anger
- different strong emotions
- movement, like exercise
- involuntary motions, reflexive, such as sneezing or yawning
- loud noises
- bright lights
- temperature modifications, particularly cold temperatures
- sun exposure
- rain
- wind
- barometric pressure changes
- altitude changes
In most patients, Central Pain Syndrome (CPS) stays a lifelong disease.
What causes central pain syndrome?
Central Pain Syndrome (CPS) guides pain that arrives from the brain and not from the peripheral nerves, which are beyond the brain and spinal cord. For this cause, it varies from most further pain diseases.
Pain is generally a protective reaction to a harmful stimulus, like touching a hot stove. No harmful stimulus generates the pain that happens in Central Pain Syndrome (CPS). Rather, an injury to the brain makes the perception of pain. This injury generally happens in the thalamus, a structure within the brain that processes sensory signals to further regions of the brain.
The most familiar diseases that can conduct to CPS contain:
- brain hemorrhage
- a stroke
- multiple sclerosis
- brain tumors
- an aneurysm
- a spinal cord injury
- a traumatic brain injury
- epilepsy
- Parkinson’s disease
Differential Diagnosis
Central pain presents in many chronic pain diseases, involving interstitial cystitis, fibromyalgia, temporomandibular condition, and irritable bowel syndrome. In extra, the differential diagnosis for central pain syndrome contains rheumatologic disorders like myopathy or myositis, polymyalgia rheumatica (PMR), psoriatic arthritis, rheumatoid arthritis, or lupus.
Also, centralized pain frequently accompanies chronic back and neck pain. It also connects with carpal tunnel syndrome, trauma, lateral epicondylitis, complex regional pain syndrome, osteoarthritis, and joint hypermobility syndrome. Centralized pain following a stroke or sequella of a neurological disease like multiple sclerosis is also a region of the differential. A thalamic stroke is also associated with a precise form of centralized pain syndrome. Lastly, mood conditions like significant depressive disorder or generalized anxiety condition are related to centralized pain.
How is central pain syndrome diagnosed?
Central Pain Syndrome (CPS) can be hard to analyze. The pain may be widespread and may appear unrelated to any harm or trauma. No single examination is available to help your doctor to analyze Central Pain Syndrome (CPS).
Your doctor will check your symptoms, conduct a physical examination, and ask about your medical record. It’s very essential to notify your doctor regarding any diseases or injuries you have now or may have had in the history, and any drugs you’re taking. Central Pain Syndrome (CPS) doesn’t form by itself. It only happens following an injury to the CNS.
Your doctor will bring a medical record and conduct a physical examination. An imaging examination, like an MRI, might be used to select the exact area of the damage. Central Pain Syndrome (CPS) can be hard to analyze. One familiar feature is that CPS must observe an event that injures or harms the central nervous system.
How is central pain syndrome treated?
Treatments for central pain syndrome possess medical and surgical choices.
Medications
Narcotics like codeine, morphine, hydrocodone, and oxycodone frequently are not useful for central pain syndrome. More frequently, drugs that modulate the neurotransmitters in the brain are used to assist control of central pain. These drugs were originally developed for further purposes like managing depression and epilepsy:
Antidepressants: amitriptyline, duloxetine, and nortriptyline
Anticonvulsants: carbamazepine, gabapentin, pregabalin,phenytoin, topiramate and levetiracetam
Surgery
When drugs fail to provide sufficient relief, surgical methods may benefit. The primary surgical methods utilized for central pain are:
Motor cortex stimulation: Using computer-guided surgical methods, stimulating electrodes are put on the surface of the brain over the area controlling the motion of the painful body region. An implanted pulse generator (battery) transmits constant electric pulses to the site to ease the pain.
Deep brain stimulation: One or two small wires are put deep in the regions of the brain that relay pain signs. Microelectrode recording (brain mapping) methods are utilized to specifically localize the location to put the electrode. An implanted pulse generator (battery) transmits constant electrical pulses to the region to ease the pain.
Prognosis
Prognosis is better in persons when the underlying condition state initially generated the pain can be corrected, cured, or managed, as in a shoulder replacement in osteoarthritis. Persons with osteoarthritis and centralized pain notice pain decrease with pharmacological treatment aimed at osteoarthritis and an increase in adverse pain outputs following joint replacement surgery.
When osteoarthritis is comorbid with central pain syndrome, the severity of the person’s pain does not connect with the radiographic severity of osteoarthritis. Also, these persons with radiological proof of osteoarthritis in a single joint were at raised risk of having numerous painful joints. Also, these comorbid people have more synovitis and effusion in knee osteoarthritis.
Central sensitization also plays a part in inflammatory arthritis. It happens in a considerable subset of the person population. Also, persons with rheumatoid arthritis and comorbid fibromyalgia have worse documented pain and poorer mental health and bring more drugs for pain, involving prednisone, while simultaneously having lower levels of inflammatory markers. Persons with inflammatory arthritis and central pain syndrome also have inferior results. Persons with centralized pain and comorbid rheumatoid arthritis sorrow from hyperalgesia at nonarticular areas in extra to articular covers.
Complications
The effect of central pain disease involves multiple conditions.
In rheumatoid arthritis, central pain is associated with neuropathic symptoms, raised pain scores without changes to inflammatory markers, raised adverse results, and fewer remission rates.
Central sensitization is associated with the raised use of opioids, as well as raised pain severity in persons with osteoarthritis, and is related to poorer person results.
A person with bilateral knee pain is at raised risk for joint pain in places further than the knees at a one-year follow-up.
For spondyloarthritis, central sensitization likens to worse results and condition scores, as well as poorer outcomes in therapy.
Centralized pain in lupus brings associations with mood changes, more substantial sleep disturbances, and worse results.
In chronic back pain, central pain syndrome generates more effective pain and mood modifications, as well as rising adverse effects. Joint hypermobility syndrome links with raised pain severity and poorer personal results.
In a person with carpal tunnel syndrome, central pain syndrome is associated with poorer surgical results, while in lateral epicondylitis, it is associated with more extreme pain, raised duration of pain, and a greater risk of failed therapy reactions.
For chronic whiplash injuries, centralized pain likens with raised pain, cognitive disturbances, and poorer results.
Preoperative increases in fibromyalgia pain scores are likened to the management of more postoperative morphine counterparts and less reaction to NSAIDs.
FAQ
Does Central pain syndrome ever go away?
In most patients, central pain syndrome stays a lifelong disease. Central pain syndrome can be restricted to a precise size of the body like the hands or feet or may be widespread over a big part of the body. Some locations of the body may be more greatly involved than further sites
Is chronic pain syndrome a mental disorder?
The sources of Central Pain Syndrome (CPS) are both physical and mental. Some professionals think that person with the disease has an issue with the system of nerves and glands that the body uses to handle pressure. That generates a sense of pain differently.
Who diagnoses chronic pain syndrome?
A pain management professional is a physician with special training in analyzing and managing chronic pain. Their primary purpose is to assist you to enhance your quality of life, and they frequently work as a region of a team with physical therapists, nurses, and mental health professionals.
How long does chronic pain syndrome last?
Chronic or persistent pain is pain that brings on for longer than 12 weeks despite drug or therapy. Most people get back to normal after pain following damage or operation. But periodically the pain brings on for longer or arrives on without any record of an injury or operation.
How much pain is too much pain?
Extreme Pain.
When it intensifies to level 8, pain makes even maintaining a conversation excessively hard and your physical activity is hardly impaired. Pain is told to be at level 9 when it is severe, controls your speaking, and may even create you moan or cry out. Level 10 pain is intolerable.






One Comment