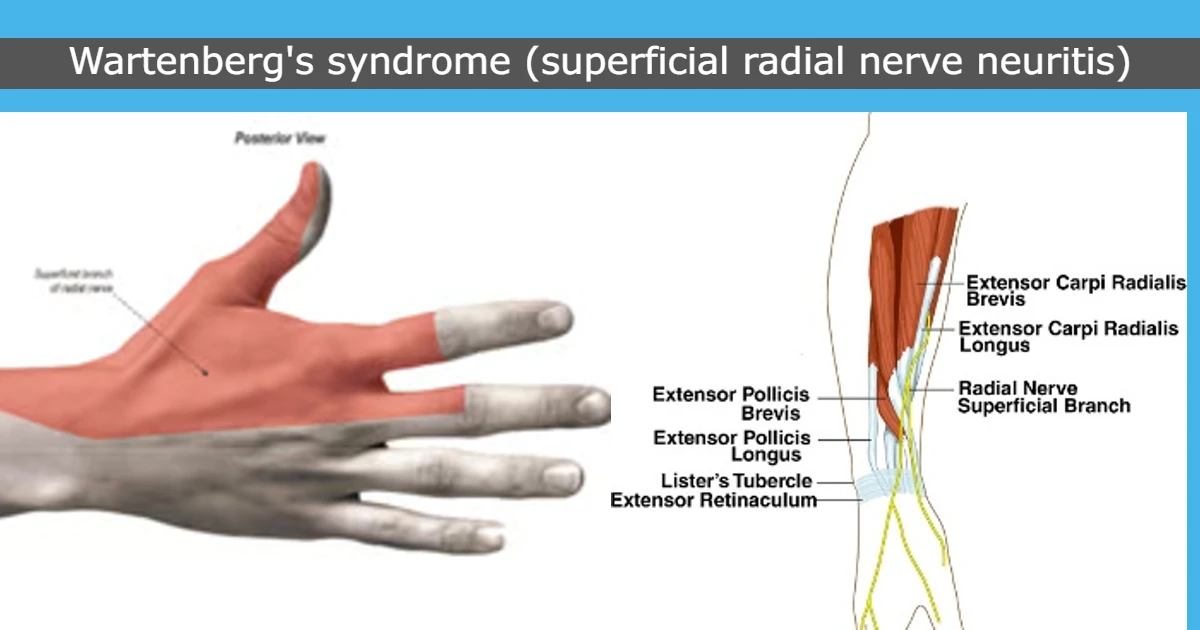
Cheiralgia Paresthetica (Warternberg syndrome):
What is a Cheiralgia Paresthetica?
Cheiralgia Paresthetica is the entrapment of the superficial branch of the radial nerve with only sensory functions altered no other movements are restricted. In this condition, the patient has pain over the distal radial forearm and paresthesia present over the dorsal radial hand.
Cheiralgia Paresthetica also called Warternberg syndrome is a compressive neuropathy. This is an entrapment neuropathy of the superficial sensory radial nerve (SRN). Due to compression by the movement of the brachioradialis and extensor carpi radialis longus (ECRL) during forearm rotation, for example, when turning a key. The condition comes and goes with suffering long periods, potentially years, sometimes without complaint interrupted by one or more attacks in succession. It is considered a benign condition. Conservative treatment is rest, wrist splints, and CSIs with surgical decompression used in rare cases.
In 1932, Wartenberg described isolated neuropathy of the Superficial Radial Nerve (SRN). The Incidence was rare like < 1 per 100,000 annually. The male: female ratio is 1:4, it is seen as more common in women in 20-70 years of age.
Cheiralgia Paresthetica is caused by compression of the superficial branch of the radial nerve at the point where the nerve arises from beneath the muscles. Entrapment of the superficial branch of the radial nerve happens where the nerve pierces the antebrachial fascia approximately 2/3 the go down the forearm at the lateral border between the brachioradialis and extensor carpi radialis longus muscles. Entrapment occurs with repetitive pronation movement of the forearm and the brachioradialis muscles close the space between these two muscle tendons in a scissor-like fashion while rotating the nerve. Pain aggravates with forced pronation and ulnar deviation of the wrist.
Anatomy of the superficial radial nerve:
The superficial sensory branch of the radial nerve arises from the division of the radial nerve in the proximal forearm, it travels deep to the brachioradialis in the undersurface of forearm muscle approximately 9 cm proximal to the radial styloid then emerges between the brachioradialis and extensor carpi radialis longus (ECRL) to become superficial. The superficial radial nerve (SRN) continues to run in the subcutaneous tissues. It gives branches to dorsal digital nerves and it is responsible for carrying afferent sensory input from the dorsum of the thumb, index, and middle fingers proximal to the proximal interphalangeal joints.
Branches:
The dorsal branch is situated 1-3cm radial to Lister’s tubercle. It supplies 1st and 2nd web space.
palmar branch passes within 2cm of 1st dorsal area directly over the extensor pollicis longus and supplies the dorsolateral thumb.
Radial Nerve Roots: C5, C6, C7, C8 and T1.
Pathophysiology:
The SRN is entrapped at any point along its whole course in the forearm, but the higher risk is at the posterior border of the brachioradialis. Trauma is also a common cause for superficial radial nerve compression, which occurs from direct pressure on the nerve (i.e. by a wristband or handcuffs) or due to stretch injury to the nerve (for example, closed reduction of a forearm fracture).
Wartenberg’s symptoms and injury of the nerve are related to the amount of force on the nerve and the duration of compression of the nerve.
Due to the compression injury to the microvasculature of the nerve, the myelin sheath of the nerve, or the nerve itself.
Mild compression, congestion, and edema give result in obstructing the venous flow, leading to Schwann cell necrosis and demyelination from resultant ischemia.
Due to Severe compression, arterial flow is obstructed which can lead to axonal injury and result in ischemia.
The duration of compression also affects the nerve in a different manner:
1) Intermittent compression can lead to transient decreases in blood flow.
2) Chronic compression results in a long time decrease in blood flow.
These chronic changes can lead to demyelination, inflammation, scar formation, fibrosis, and eventual axonal degeneration. It is necessary to remove before severe nerve damage has occurred, for a better chance of recovery. Remyelination of the nerve can take a few weeks for recovery. However, axonal regrowth is very slow.
Cause of Cheiralgia Paresthetica:
The radial nerve is compressed anywhere along its whole course. Due to the superficial region of the terminal branches, the nerve has a higher risk for local trauma. Tight wristwatches and tight handcuffs can compress the nerve over the lateral wrist region. It is also at risk for compression occurring by distal radius fracture fragments of soft tissue masses (like lipomas or ganglion cysts). Another cause of nerve injury is an iatrogenic injury during first dorsal compartment release, internal fixation of distal radius fractures, wrist arthroscopy surgery, and external fixation placement.
similar procedures such as acupuncture, cephalic venipuncture, cannulation, and radial arterial line removal. Steroid injections are given into the tendon sheath for de Quervain’s tenosynovitis and it can damage the nerve itself and cause subdermal atrophy resulting in injury to the nerve.
Repetitive supination and pronation movement and especially hyperpronation can entrap the nerve between the brachioradialis and extensor carpi radialis longus muscles. During forearm supination movement, these two tendons are parallel to each other, and the nerve doesn’t get compressed. But during pronation movement, the extensor carpi radialis longus crosses the brachioradialis muscle and compresses the nerve.
The presence of diabetes mellitus in the body is also responsible for the development of Wartenberg’s syndrome. This condition is also associated with De Quervain’s disease in 20-50%.
Symptoms of Cheiralgia Paresthetica:
- Burning type of pain at the proximal forearm and the dorsomedial hand.
- Tingling sensation
- Numbness
- Hypoaesthesia
- No, muscular weakness is present
- The symptoms are also aggravated by repetitive movement of wrist flexion and ulnar deviation
Signs:
It is a neurological sign that consists of involuntary abduction of the fifth (little) finger and it is caused by unopposed action of the extensor digiti minimi.
This commonly results from weakness of some of the ulnar nerve supply by the intrinsic hand muscles -in particular denervation of the nerve which is supplied to the palmar interosseus muscle to the little finger.
Tinel’s sign is positive when taped over the particular area of the superficial nerve.
A provocative test for repeated wrist flexion, ulnar deviation, and pronation movement.
Physical examination:
- Provocative tests.
- Tinel’s sign is the superficial sensory radial nerve (most common exam finding).
- Wrist flexion, ulnar deviation, and pronation movement repeatedly for one minute.
- Finkelstein test: The patient sits in a comfortable position and relaxed hand relaxed on the table. The patient’s affected hand is in the air, while the other hand rests beside the body. The therapist asks the patient to make a fist around a thumb and do an ulnar deviation movement(wrist movement in the upward direction). By this test, 96% of patients have aggravated symptoms.
- Masses, scars, and external compression are present.
- Skin changes.
Sensation:
Light touch: This may be abnormal.
2-point Discrimination: This may be abnormal in 80% of patients.
Vibration (256 Hz): This may be abnormal.
Muscle Strength: No motor weakness or signs of atrophy. Maybe grip strength is reduced.
Special test for the superficial branch of the radial nerve and lateral antebrachial cutaneous nerve.
- Hoffman Test: Identify the upper motor neuron disorder.
- Dellon Test: Active, forceful hyperpronation of the forearm and ulnar deviation and flexion of the wrist with the elbow extended by the side.
- Wartenburg’s Neuritis Compression Test.
- Superficial Branch of the Radial Nerve Compression Test.
Optional Examination with Nerve Block:
Local anesthesia block the superficial branch of the radial nerve:
- Given the local anesthesia subcutaneously near the area of entrapment.
- Ultrasound advised preferred to avoid nerve injury.
- Finkelstein Test may become negative.
- Measured pinch and grip strength may be improved.
Another evaluation:
Imaging Examinations:
Radiography:
If the entrapment of the radial nerve in the arm, a radiological investigation should be performed to check for any fracture, healing callus, or tumor. In radial tunnel syndrome and posterior interosseous nerve syndrome, radiological reports give the confirmation for any condition like; elbow or forearm fractures, dislocations or instabilities, tumors, and arthrosis.
Nerve Conduction Study:
It is used to check the electrical activity of the affected nerve and compare it to normal values.
It May be able to find the location and nature of nerve injury incorrectly way.
Ultrasonography:
It helps identify the different causes of wrist pain like cheiralgia paresthetica, de Quervain tenosynovitis, and thumb joint arthritis.
It also uses to identify areas of nerve entrapment or compression.
Plain Radiographs:
They help to identify any bony prominences or orthopedic conditions present.
Magnetic Resonance Imaging:
T1-weighted images can give any narrowing or enlargement of the bony part.
T2-weighted images fat suppressed density- weighted can identify the changes in the nerve itself including edema and enhancement. It is also useful to check lipomas, ganglions, and aneurysms.
Electromyography:
EMG helps to locate the injured area and monitor the nerve recovery time. EMG was not positive in 3-6 weeks after injury. After the 4 months of the injury, nerve recovery should be demonstrable.
If the medial branch of the posterior interosseous nerve is compressed, EMG and conduction studies results are an abnormal function of the extensor carpi ulnaris, the extensor digitorum communis, If only the lateral branch is compressed, then abnormal function of the abductor pollicis longus, the extensor pollicis longus and brevis, and the extensors indicis muscles. The site of compression is localized if the proximal part is compressed its function is normal and if the distal part is compressed so its function is abnormal.
Differential Diagnosis:
Patients with SRN compression have pain or dysesthesias on the dorsal radial forearm and pain radiating to the thumb and index finger, however, the distribution of symptoms may vary owing to differences in anatomy. When the sensory disturbances present concomitantly with weakness of the muscles which is supplied by PIN, the dr may consider alternative diagnoses, such as a more proximal lesion or a mass in the radial tunnel in large to affect both the PIN and SRN. Because compression of the SRN often occurs in the first dorsal compartment area, SRN entrapment symptoms may be confused with the symptoms of de Quervain’s tenosynovitis having pain with ulnar deviation of the wrist. The main symptom is if the SRN compression is present have the symptoms at rest.
De Quervain’s tenosynovitis:
In this condition, pain is not aggravated by wrist pronation movement, unlike Wartenberg Syndrome.
Lateral antebrachial cutaneous nerve (LACN) neuritis:
Intersection syndrome:
This may have dorsoradial forearm swelling.
The symptom is exacerbation and “wet leather” crepitus on the repeated movement of wrist flexion or extension.
Thumb carpometacarpal joint arthritis.
Complications of Cheiralgia Paresthetica:
- Failed decompression surgery.
- Persistent pain and numbness
- Wound dehiscence
- Infection
- Worsening of symptoms
- Injury to the surrounding of the suture.
Treatment of Cheiralgia Paresthetica:
Conservative Management:
- This condition is mainly treated conservatively. If external compression is a common underlying cause, the removal of the tight element such as a wristwatch or bracelet is an essential component of nonsurgical management.
- Rest,
- Splinting,
- Nonsteroidal anti-inflammatory drugs.
- activity modification.
More patients treated nonoperatively in this condition have good to excellent outcomes.
Surgical management:
surgical decompression.
Surgical Decompression:
Neurolysis and fascia band release between the brachioradialis and extensor carpi radialis longus:
Procedure:
To reach the superficial branch of the radial nerve, first, palpate the radial styloid process and follow the border of the brachioradialis proximal to 10 cm. Draw a line to connect the two muscles. Identify the entrapment area. Then center the incision over this. Pick up skin flaps to identify the brachioradialis and extensor carpi radialis longus tendons. The superficial branch of the radial nerve generally appears between the two tendons, brachioradialis situated above and extensor carpi radialis longus situated below. slowly dissect out the nerve and free it from adhesions. Remove any adhesions or fascial bands which is compressing the nerve.
Fully decompression, one can choose to wrap the nerve in many different adhesive barriers. The nerve compression area is carefully measured, and the barrier is trimmed to match. It is then situated around the nerve and placed loosely with 8-0 nylon sutures if needed. One can proceed with layered closure and apply the soft sterile dressing.
Postoperative care should be necessary for an early range of motion. Physical therapy should be started after 2 weeks of surgery. It should reinforce this early range of motion protocol and nerve gliding techniques to reduce the adhesion formation, desensitization, and scar massage given around the scar area. Patients receive therapy for 4 to 6 weeks and achieve maximum medical improvement in 60 to 90 days after surgery.
Physiotherapy Treatment of Cheiralgia Paresthetica:
- Peripheral nerve stimulation (PNS) – for reduced pain.
- Pulsed low-intensity infrared laser,
- Electrical stimulation.
- Splint
- mobility exercise
- Ice massage
Peripheral nerve stimulation:
Given the nerve stimulation or TENS modality over the pain area. It helps to decrease the pain by the pain gate theory.
Apply this stimulation for 10 mins once a day.
Pulsed low-intensity infrared laser:
Laser is placed over the pain area it also helps to reduce the pain and tissue healing. Before starting, this modality asks to the patient whole precautions for this modality. The therapist also takes a history of the patient and any previous surgery. infrared rays go into the body directly on the affected part. This modality is used after the surgery for tissue healing purposes.
Splint:
Advised the patient to wear a wrist splint for the restricted or avoid the jerky movement and hand will be supported.
- Stimulation is given for the affected muscles of the lateral border of the brachioradialis and extensor carpi radialis longus.
- First, find out the exact motor point of the muscle.
- Given the first galvanic current and then progressively faradic current. It will be decided according to the patient condition and examination results and mobility of the hand.
Mobility exercise:
- In this condition, the forearm pronation or wrist deviation movement is restricted or painful so that starts with less repetition for wrist ulnar and radial deviation, and forearm pronation movement.
- The therapist asks them to sit in a relaxed position in a supported chair, forearm will be supported, make a fist and rotate the forearm front and back. Repeat it 5 to 7 times then gradually increase.
- Then ask the patient to do the wrist deviation movement. Repeat it 5 to 7 times and gradually increase.
- Do this exercise with a pain-free range.
FAQ
What is Cheiralgia?
Cheiralgia paresthetica is a compression neuropathy of the superficial radial nerve. It manifests as sensory disturbances, such as paresthesias, to the dorsal and radial aspects of the wrist and hand. It is also known as Wartenberg’s syndrome.
What is a positive Wartenberg sign?
A positive sign of Wartenberg’s syndrome is the observation of the 5th digit abduction movement and the inability to adduct the 5th finger when extended.
What is Wartenberg’s migratory sensory neuropathy?
Wartenberg’s migratory sensory neuropathy is characterized by frequent episodes of burning pain and loss of sensation in the distribution of one cutaneous nerve at a time. It commonly affects the skin of the extremities, chest, and face.
What causes Wartenberg?
This syndrome is caused by compression of the superficial branch of the radial nerve at this point, where the nerve arises from under the muscles. In this condition, the superficial radial nerve is compressed in between the brachioradialis and the extensor carpi radialis tendons, especially during forearm pronation movement.
Do this exercise with a pain-free range.