Developmental Coordination Disorder
What is developmental coordination disorder?
- Children normally develop the ability to sit up, stand, walk, and talk at foreseeable ages. When they are behindhand in achieving these milestones, it may require a developmental problem. Developmental coordination disorder is one such condition.
- Developmental coordination disorder (DCD) is a lack of coordination between your mental intentions and your capacity to get your body to carry out those intentions.
- When you try to tie your shoe, However, your brain does not properly send the order for shoe tying to your hands and feet.
- Your brain realizes how to tie shoes, yet your hands just can not follow your brain’s instructions.
- The equal thing happens when you try to run, jump, write, button a shirt, and many other tasks that most people take for granted.
- People with developmental coordination disorder generally have normal intelligence.
- However, developmental coordination disorder is sometimes called “clumsy child syndrome,” and it may cause others to think that people with this condition are incompetent or unintelligent because they cannot perform basic tasks.
- This condition can be considered a childhood disorder, yet the effects of developmental coordination disorder continue into adulthood.
What are the symptoms of developmental coordination disorder?
- Different areas of development can be affected by developmental coordination disorder and these may persist into adulthood.
- Developmental coordination disorder has no cure.
- Often various to deal successfully with difficult situations strategies are developed, and these can be increased through occupational therapy, psychomotor therapy, physiotherapy, speech therapy, and psychological training.
- Incorporation to physical impairments, developmental coordination disorder is associated with problems with memory, especially working memory.
- This typically consequences in difficulty remembering instructions, difficulty organizing one’s time and remembering deadlines, increased tendency to lose things, or problems carrying out tasks that require remembering several steps in sequence.
- Whilst most of the widespread population experiences these problems to some extent, they have a much more significant collision on the lives of dyspraxic people.
- However, many dyspraxics have excellent long-term memories, notwithstanding poor short-term memory.
- Many dyspraxics useful from working in a structured environment, as repeating the same routine minimizes difficulty with time management and allows them to confine procedures to long-term memory.
- People with developmental coordination disorder sometimes have adversity moderating the amount of sensory information that their body is continuously sending them, so as a result, these dyspraxics can be prone to sensory overload and panic attacks.
- Moderate to extreme difficulty doing physical tasks is experienced by some people with dyspraxia, and fatigue is common because so much energy is expended trying to accomplish physical movements correctly.
- Some dyspraxics have hypotonia, and low muscle tone, which like developmental coordination disorder can detrimentally affect balance.
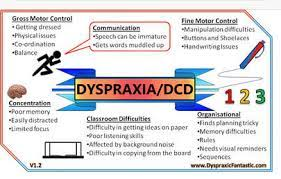
Gross motor control
- Entire body movement and motor coordination issues mean that major developmental targets including walking, running, climbing, and jumping can be affected.
- The difficulties differ from person to person and can include the following:
- Poor timing.
- Poor balance(sometimes even falling over in mid-step).
- Stumbling over one’s own feet is also common.
- Difficulty combining movements into a controlled succession.
- Difficulty remembering the next movement in succession.
- Problems with spatial awareness, or proprioception.
- Trouble picking up and holding onto simple objects like as pencils, owing to poor muscle tone or proprioception.
- Clumsiness to the point of knocking things over, causing minor injuries to oneself, and rebounding into people accidentally.
- Difficulty in refereeing left from right.
- Cross-laterality, ambidexterity, and a shift in the preferred hand are likewise common in people with developmental coordination disorders.
- Problems with chewing foods.
- Fine motor control.
- Fine motor problems can cause difficulty with a wide variety of other tasks like as using a knife and spoon, fastening buttons and shoelaces, cooking, brushing teeth, styling hair, shaving, applying cosmetics, opening jars, and bottles, and packets, locking and unlocking doors, and doing housework.
- Difficulties with fine motor coordination lead to problems with handwriting, which may be due to either ideational or ideo-motor difficulties.[non-primary source needed] Problems associated with this area may include:
- Learning basic movement patterns.
- Developing a desired writing speed.
- Successfully to the correct pencil grip.
- Handwriting is difficult to read and may fail to catch words in sentences or place words in the incorrect order.
- The appropriation of graphemes – e.g. the letters of the Latin alphabet, besides numbers.
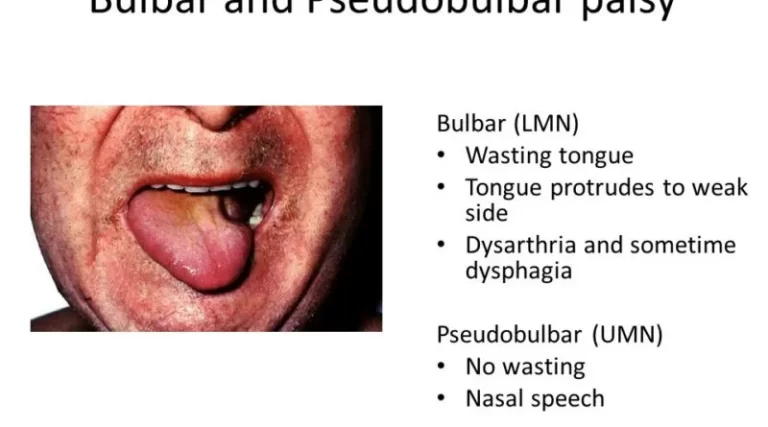
- Developmental verbal dyspraxia
- Developmental verbal dyspraxia (developmental coordination disorder) is a type of ideational dyspraxia, that causes speech and language impairments.
- This is the supported term in the UK; however, it is also sometimes referred to as articulatory dyspraxia, and in the United States (US) the usual term is childhood apraxia of speech (CAS).
Key problems include:
- Difficulties jurisdictions the speech organs.
- Difficulties developing speech sounds.
- Difficulty sequencing sounds
- Within a word, and
- forming words into sentences.
- Difficulty jurisdictions breathing, suppressing salivation, and phonation when talking or singing with lyrics.
- Slow language development.
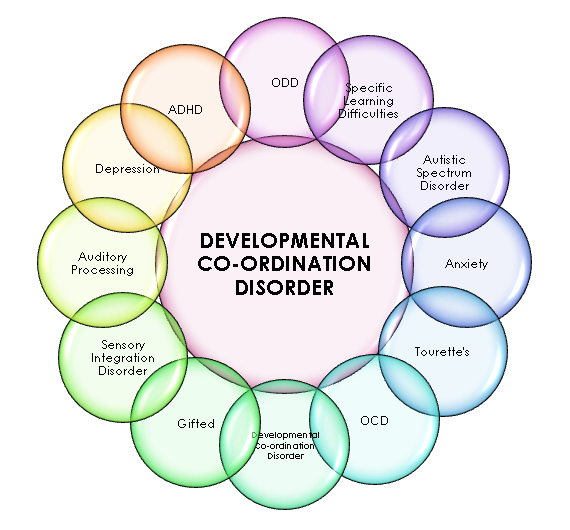
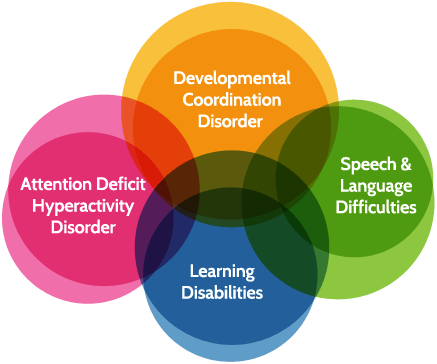
Associated disorders and secondary consequences:
- People who have developmental coordination disorder may likewise have one or more of these co-morbid conditions:
- Attention deficit hyperactivity disorder (inattention, hyperactivity, impulsive behavior).
- Fetal Alcohol Spectrum Disorder
- A condition on the autism spectrum.
- Dyscalculia (difficulty with numbers).
- Dysgraphia (an incapability to write neatly or draw).
- Dyslexia (difficulty with reading and spelling).
- Hypotonia (low muscle tone).
- Nonverbal learning disorder.
- Sensory processing disorder.
- Developmental Language Disorder (DLD).
- Visual perception deficits.
- However, a person with developmental coordination disorder is unlikely to have all of these conditions.
- The pattern of difficulty differs widely from person to person; an area of major weakness for one dyspraxic can be an area of strength or power for another.
- For example, while some dyspraxics have difficulty with reading and spelling as a result of dyslexia, or with numeracy as a result of dyscalculia, others may have brilliant reading and spelling or mathematical abilities.
- Co-morbidity between attention deficit hyperactivity disorder and developmental coordination disorder is particularly high; the convergence between the two disorders is believed to be about 50% (approximately half of people with developmental coordination disorder have attention deficit hyperactivity disorder, and approximately half of people with attention deficit hyperactivity disorder have developmental coordination disorder).
What causes developmental coordination disorder?
- The causes of developmental coordination disorder are not well understood, yet researchers are convinced that it is the result of delayed brain development.
- People with developmental coordination disorder generally have no other medical issues that can explain the disorder.
- In unidentified cases, can happen with other disorders, like as attention deficit hyperactivity disorder or disorders that cause intellectual disabilities.
- Nevertheless, these conditions are not linked
- Researchers do not know the cause of developmental coordination disorder, but there are some risk factors.
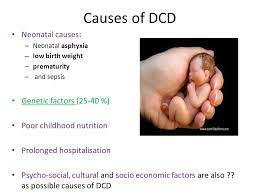
These include:
- Being a male
- Being little for gestational age
- Being born prematurely or with a less birth weight
- Genetics, or a history of developmental coordination disorder in the family
- If you have inquiries about these risk factors, reach out to your child’s doctor for additional information.
How developmental coordination disorder is diagnosed?
- There are a number of professionals who can either diagnose or identify developmental coordination disorders.
- Ideally, they will work as a group to evaluate a child.
- Certain types of medical doctors can diagnose developmental coordination disorders.
- They include:
- Pediatricians
- Developmental-behavioral pediatrician
- pediatric neuropsychologists
- child pediatrician
Developmental-Behavioral Pediatricians(What You Need to Know):
- If you are worried that your child is showing signs of a developmental delay or behavior difficulties, who can help you figure out what is going on?
- The first person to speak to is your child’s doctor or other health care provider.
- The doctor may mention you to a type of medical specialist who focuses on these issues.
- That professional is called a developmental-behavioral pediatrician.
- These doctors are trained as a pediatrician.
- Yet they go on for another three years of training in developmental and behavioral problems.
- They frequently work in metropolitan areas, so depending on where you reside, you may not have uncomplicated to access to one.
- Here is what you need to know about developmental-behavioral pediatricians.
What do developmental-behavioral pediatricians do?
- The main role of developmental-behavioral pediatricians is to evaluate kids who are not developing, learning, or behaving the way their peers are.
- Kids may be referred to them across the early intervention program in their state.
- They are also referred through their regular doctors.
- These specialists can tease apart what you are seeing and come up with a diagnosis.
- For example, if your child acts up at school and in other settings, you or the teacher may suspect your child has attention deficit hyperactivity disorder.
- But there are other issues that may look like attention deficit hyperactivity disorder, like as anxiety.
- And several kids will have more than one issue.
Here are certain the things certain developmental-behavioral pediatricians might evaluate for:
- Delayed development during the speech, language, or motor skills,
- Nonverbal learning disabilities or other social skills issues,
- Attention deficit hyperactivity disorder,
- Mental health issues like anxiety,
- Autism,
- Performance issues in school,
- Learning differences such as dyslexia.
- The evaluation process With a developmental-behavioral pediatrician
- There is a succession of things a developmental-behavioral pediatrician may do as part of the evaluation.
- These include:
- Taking an exhausted history of your child,
- Doing a medical exam,
- Observing and discussing with your child,
- Inquiring how your child acts in a variety of settings,
- Seeking a response from teachers at your child’s school or daycare,
- The doctor may also desire your child to be evaluated by other specialists.
- Those might incorporate an occupational therapist, a physical therapist, or a neuropsychologist.
- After looking at whole the information, the doctor possible to make a diagnosis.
- There possibly to be cases where she holds off making it right away, nevertheless.
- The diagnosis may not be clear, or there might not be a diagnosis that applies.
- The doctor may discern your child periodically to monitor his development and progress with you.
What happens after a diagnosis?
- The developmental-behavioral pediatrician might maintain without interruption to treat of your child or she might recommend other professionals who can help with ongoing treatment.
- Here are certainly other ways she might help:
- Prescribe and monitor medication if your child has an issue such as attention deficit hyperactivity disorder or anxiety.
- Help you better understand what is behind your child’s behavior and come up with discipline strategies.
- Recommend services at school, and therapies exterior of the school.
Pediatric Neuropsychologists (What You Need to Know?)
- If you believe your child may have learning and thinking differences, where do you go to find out? You can inquire to have him evaluated at school.
- you can carry him to a specialist for a private evaluation.
- One type of specialist who diagnoses, and sometimes treats, kids with learning and thinking differences is known as a pediatric neuropsychologist.
- Here is what you need to know about pediatric neuropsychologists.
What do pediatric neuropsychologists do?
- Pediatric neuropsychologists are licensed psychologists who job with kids.
- They have additional training and expertise, nevertheless.
- Their attention is on how learning and behavior are related to brain development.
- These specialists have a doctoral degrees in psychology and work in personal practices and hospitals.
- They likewise complete a two-year fellowship in neuropsychology.
- They are not medical doctors, so they can not prescribe or manage medications.
- Their important role is to diagnose conditions.
- Certain may also provide therapy and academic interventions.
- These specialists give kids many of the equal tests used in school evaluations to look for areas of strengths and weakness.
- Yet they may look at the results in different ways, or do additional testing.
Pediatric neuropsychologists can diagnose issues in these areas:
- Sensory and motor skills,
- Attention and focus,
- Language skills,
- working memory,
- Visual-spatial processing,
- executive functioning skills,
- Academic skills, like as reading or math,
- They utilize their knowledge of brain development when assessing the test results.
- From there, they can form a diagnosis and explain not just the areas of weakness, but what is causing it.
- In certain cases, that might be multiple challenges or conditions.
- For example, if your child is struggling with reading, there are several possible reasons.
- It may be an attention difficulty.
- It may be a reading cogency issue or an auditory processing disorder.
- There are other possibilities, excessively.
- And testing may disclose that your child has more than one issue that is causing his trouble with reading.
The evaluation process with a pediatric neuropsychologist
- The evaluation process can carry anywhere from five to twelve hours.
- You and your child will require to meet with the specialist several times.
- Here is what to expect at these meetings.
- Initial visit: The neuropsychologist will collect a detailed case history.
- You may be inquired to fill out questionnaires about your child’s development and behavior.
- From there, the specialist will decide on the appropriate tests to confer on your child.
- Testing: Your child will come back for anywhere from two to four sessions of testing.
- A session can rearmost from 90 minutes to three hours.
- The specialist will determine the session length that is right for your child.
- Review and diagnosis: Once the neuropsychologist has reviewed the test results, you will meet again.
- If your child is a teen, he will likely be part of this discussion.
- The specialist will describe what the tests show and how they explain what you are seeing in your child’s learning or behavior.
- If your child has one or more learning and thinking differences, the specialist will diagnose them.
- The neuropsychologist as well as might suggest types of help for your child or come up with a treatment plan.
- In her report, she may recommend that your child get particular support and services at school. Some neuropsychologists as well as provide more specialized therapy in their offices or at a hospital.
- You might also acquire a referral to other types of professionals.
- These might incorporate a psychologist, speech-language pathologist, occupational therapist, reading specialist, or doctors who can prescribe medication.
How do pediatric neuropsychologists work with schools?
- Once you have the test results, the IEP or 504 plan team at school will gather to discuss them.
- Often, they will have done their own evaluation as well.
- A clinical diagnosis is not equal to the identification of learning disabilities that a school makes.
- The school will own the specialist’s report.
- But it is the best idea to have the neuropsychologist be part of the conversation.
- That can occur over the phone or in person.
- She can support making sure that the school’s treatment plan addresses all of your child’s issues.
- Let’s tell your child’s diagnosis is dyslexia.
- The school might incorporate special reading instruction in his IEP.
- But your child may require other supports or services to help with particular problems.
- Maybe he has difficulty with phonological awareness.
- The specialist might recommend that he job with a speech-language therapist.
- Those types of details can be unable or minimized in a long report.
- Having the specialist there means that she can answer the team’s questions and construe key details in the report.
Child psychiatrists
- Previously your child is evaluated for developmental coordination disorder, these doctors should rule out any other medical causes for your child’s coordination difficulties.
- There are other professionals who may assess for and diagnose developmental coordination disorder. But they can not make a diagnosis.
- These include:
- Physical therapists and occupational therapists
What is occupational therapy?
- Occupational therapy is a treatment for difficulties with movement and coordination.
- It assists people to improve the motor skills involved in everyday tasks, like writing and getting dressed.
- These skills incorporate fine and gross motor skills and motor planning.
- Therapists to work on coordination, balance, and self-regulation skills.
- Kids can get occupational therapy for free at school.
- Yet adults have to find a therapist who works privately(Doctors can frequently recommend private occupational therapists).
- Insurance may or may not cover occupational therapy.
- The need for occupational therapy can come up at any age and for a wide range of reasons.
- But there are lifelong conditions that collision motor skills starting in early childhood.
- One of them is developmental coordination disorder.
- While adults with developmental coordination disorder may benefit from occupational therapy, it is most effective with kids. And the earlier occupational therapy starts, the better.
- Educational evaluators
- Psychologists
- Researchers
- The most common ages to evaluate for developmental coordination disorder are 5 and 6.
- Evaluators will expect motor and cognitive skills.
- They will ask questions about other factors that could be having an impact, as well as, in school and home life.
- They will also want to know whether your child has hit unquestionable milestones in development and when symptoms began.
- Evaluators use unquestionable tests to assess movement skills.
- These skills include:
- Strength
- Balance
- Coordination
- Range of motion
- Motor planning
- Fine motor control
- Evaluators might look at dexterity by having kids do things such as trace and string beads.
- They might assess visual-perception skills by looking at how satisfactorily kids can draw a progression of shapes and stay in the lines when drawing.
What is physiotherapy for DCD?
- Your child’s first physical therapy session will start with a complete evaluation.
- Your child’s physiotherapy may:
- Take a whole medical history.
- They will inquire questions about the mother’s pregnancy and the child’s birth and development (the age the child sat up, crawled, walked), the general health of the child, and the parent’s concerns.
- Scale the child’s height and weight.
- Notice the child’s movement patterns.
- Assess the child’s muscle strength, tone, flexibility, & balance.
- Test the child’s movement skills, like skipping or walking in a straight line.
- Screen for problems using their hands, vision, language skills, intellect, and other regions of development.
- Mention you and your child to other health care providers as part of a team approach to address your child’s needs.
- Physical therapists work with children with developmental coordination disorders to improve muscle strength, coordination, and balance.
- They as well as help them develop skills to improve their daily activities and quality of life.
- Your child’s program may in corporate treatments to:

- Improve strength.
- Your physical therapist will educate you and your child on exercises to increase muscle strength.
- They will diagnose games and fun tasks that improve strength, reduce obesity, and improve heart health.
2. Improve balance.
- Your physical therapist may teach your child exercises to help improve their balance, like standing on one foot.
3. Improve body awareness.
- Your physical therapist might have your child play in obstacle courses to help them determine how to plan movements while having fun.

4. Improve skills through task-oriented and task-specific learning.
- Your child may learn fun new skills such as bike riding.
- Your physical therapist may purpose making adjustments (like using a 3-wheeled bike or training wheels for bike riders) to keep your child safe as they learn new activities.
Can this injury or condition be prevented?
- The exact cause of developmental coordination disorder is unknown.
- Research has shown that the disorder is linked to premature birth and less birth weight.
- Sometimes changes in the brain can be noticed on brain scans ordered by a physician.
- One zone of the brain, the cerebellum, may be affected.
- Research is ongoing.
- If your child is diagnosed with developmental coordination disorder, a physical therapist can work with you and your child to assist to prevent added complications that might occur including:
- Poor posture
- Walking with the feet moved in or out,
- Delayed learning of movement skills,
- Less self-esteem caused by being unable to keep up with peers,
- Obesity or heart disease is caused by inactivity.
What kind of physical therapist do I need?
- All physical therapists are prepared through education and experience to treat a diversity of conditions or injuries.
- You may want to consider:
- A physical therapist who has proficiency in working with children with developmental disorders.
- Certain physical therapists have a pediatric practice and will work with you and your child in your home or in the school or community environment.
- A physical therapist who is a board-certified clinical specialist or who has accomplished a residency or fellowship in pediatric physical therapy.
- This physical therapist has advanced knowledge, experience, and skills that may practice to developmental conditions.


One Comment