Costochondritis and Physiotherapy Management
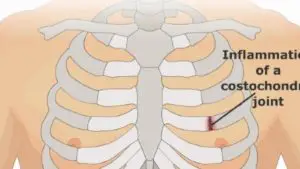
Costochondritis is a self-limiting condition defined as painful chronic inflammation of the costochondral junctions of ribs or chondrosternal joints of the anterior chest wall.
- It is a clinical diagnosis and does not require specific diagnostic testing in the absence of concomitant cardiopulmonary symptoms or risk factors.
- Costochondritis is often confused with Tietze syndrome.
- Palpation of the affected chondrosternal joints of the chest wall elicits tenderness and pain is reproduced by palpation of the affected cartilage segments which may radiate out into the chest wall.
- Costochondritis usually has no apparent cause. Treatment is mainly Symptomatic- relieving your pain while you wait for the condition to improve on its own gradually or it may take several weeks or longer.
Clinically Relevant Anatomy
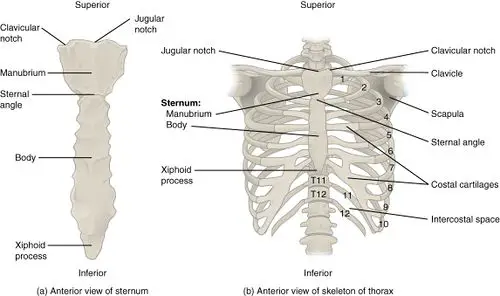
- The thoracic wall consists of the Sternum anteriorly.
- 12 thoracic vertebrae posteriorly,
- Ribs consist of bone and cartilage, with cartilage serving as an elastic bridge between the bony portion of the rib and the sternum.
- According to their attachment to the sternum, the ribs are classified into 3 groups: true, false, and floating ribs.
Cause of Costochondritis:
It is caused by inflammation of the costal cartilages and their sternal articulations, also known as the costochondral junctions, Costochondritis usually has no clear cause. Occasionally, It may happen by the following caused are:
- Injury: A fall on the chest creates strain on costochondral junctions and may lead to Pain.
- Physical strain: Heavy lifting, Over-exercise, and severe coughing may cause pain.
- Arthritis: It is also linked with Rheumatoid Diseases such as rheumatoid arthritis, osteoarthritis, or ankylosing spondylitis.
- Joint infection: Viruses, bacteria, and fungi — such as tuberculosis, syphilis, and aspergillosis — can infect the rib joint.
- Tumors: Noncancerous and cancerous tumors can cause costochondritis. Cancer might travel to the joint from another part of the body, such as the breast, thyroid, or lung.
- Chest Surgery: Post-operative surgery that affects the chest wall, such as cardiac bypass
In Medical Journal- costochondritis that has no known causes is called idiopathic costochondritis.
Sing and Symptoms of Costochondritis
Chest pain with discomfort may be stabbing, burning, or aching in nature. The ribs most affected are the second to fifth ones. The pain may radiate to the back of the abdomen.
It may also get worse if you move, stretch, or breathe deeply. These symptoms can indicate other conditions, including a heart attack. Seek immediate medical care if you experience persistent chest pain.
- Occurs mainly on the left side of your costochondral junctions
- Is sharp, aching, or pressure-like
- Affects more than one rib
- Symptoms may increase when you take a deep breath or cough
There is a variation of costochondritis called Tietze syndrome. This condition causes pain associated with costochondritis, as well as swelling of the rib cartilage.
Clinical Presentation:
- As with any chest pain, a history of present illness, past medical history, social history, family history, and a review of systems are very important. Many deadly causes of chest pain should be ruled out prior to establishing a diagnosis of costochondritis.
Possible signs or Symptoms are as per following :
- The patient will give a history of chest pain worsening with movement and certain positions. The pain will also be worse when the patient takes a deep breath.
- Pain quality is variable, but it may be described as a sharp or dull aching pain.
- Patients show a gradual or rapid onset of pain and swelling of the upper costal cartilage of the costochondral junction.
- Pain is usually reproducible by mild-to-moderate palpation. Often, there is point tenderness at the costochondral junction (a pitfall of the typical physical exam findings is that pain due to acute coronary syndrome can also be described as reproducible).
- Symptoms may occur gradually and can disappear spontaneously after a few days, but equally, it may take years to disappear. Even after the symptoms have resolved, they may return at the same location or at another rib level.
- There may be stiffness of the upper thoracic spine, costovertebral joints, and the lateral ribs.
- True ribs are the ribs that directly articulate with the sternum with their costal cartilages – ribs 1-7. They articulate with the sternum by the sternocostal joints. The first rib is an exception to that rule; it is a synarthrosis and the first rib could uniquely articulate with the clavicle by the costoclavicular joint
- The false ribs (8,9,10) are the ribs that indirectly articulate with the sternum, as their costal cartilages connect with the seventh costal cartilage by the costochondral joint.
- The floating ribs (11,12) do not articulate with the sternum at all (distal two ribs).
- The ribs move with respiration and with truncal motion or movement of the upper extremities.
Evaluation
- Costochondritis is usually self-limited and benign – should be distinguished from other, more serious causes of chest pain.
- Coronary artery disease is present in 3 to 6 percent of adult patients with chest pain and chest wall tenderness to palpation.
- History and physical examination of the chest that document reproducible pain by palpation over the costal cartilage are usually all that is needed to make the diagnosis in children, adolescents, and young adults.
- Patients older than 35 years, those with a history or risk of coronary artery disease, and any patient with cardiopulmonary symptoms should have an electrocardiograph and possibly a chest radiograph.
- Consider further testing to rule out cardiac causes if clinically indicated by age or cardiac risk status.
Diagnosis
Patients with Costochondritis will present with:
- Chest pain is reproducible by palpation of the affected area, with ribs 2 to 5 mostly affected.
- Increasing factors are slouching or exercise.
- Often occurs after a recent illness with coughing or after intense exercise and it is mostly of unilateral origin.
- Maybe an associated restriction of the corresponding costovertebral and costotransverse on examination.
- Loss of normal spinal movement associated with chest pain.
- Palpation should be performed with 1 digit, on the anterior, posterior, and lateral sides of the chest, the clavicle, the cervical, and the thoracic spine.
- When on the affected area it reveals a reproducible pain that might suggest Costochondritis, but it cannot entirely be concluded.
- Motion palpation is a manual process of moving a joint into its maximal end range of motion, after which it is challenged with a light springing movement.
- This endpoint of joint movement forms the basis for determining normal or abnormal joint movement. When motion palpation is reduced, the joint is considered fixated or hypokinetic.
- X-rays and blood tests, to rule out other conditions
- To differentiate Diagnosis an electrocardiogram (ECG or EKG) or chest X-ray to make sure that the patient doesn’t have coronary artery disease or another heart condition.
Medical Treatment
- Treatment consists of conservative management and is usually also symptomatic.
Management includes:
- Reassurance
- Topical or oral analgesics.
- Local injections with steroids into the joint, tendon sheath, or around the nerve, inhibit inflammation and reduce swelling and pain to improve movement.
- If patients have severe or refractory costochondritis, refer to outpatient follow-up. Physiotherapy is a treatment option for refractory costochondritis
- Alternative treatments may also include: ice, acupuncture, manual therapy, Physiotherapy Treatment- -exercise, and other medications such as sulfasalazine which may have an additional long-term benefit in the management of costochondritis
Physiotherapy Treatment in Costochondritis:
- Education – re-assure the patient by explaining the condition
- Minimizing activities that provoke the symptoms (e.g. reducing the frequency or intensity of exercise or work activities)
- A course of trigger point therapy to reduce pain – eg. cross-fiber friction massage
- Use heat/ cold pads and massage to help against the overloading of muscles and to lessen the pain. Heat and cold pads are both equally effective. So the patient can choose which one he likes the most. Instead of using cold pads, the patient can also use Vapo-coolant spray on the involved areas. This spray can relieve the pain in the chest.
- Postural exercises – Re-train proper posture in functional positions (Neuro-muscular control). Functional training is all about using the right muscles at the right time, to sustain the correct posture, in daily activities. Simple activities like eg. correct standing posture, sitting to stand, and walking upstairs all need to be addressed to ensure correct technique and muscle recruitment.
- Thoracic manual therapies directed at the lateral and posterior rib structures to improve rib and thoracic spine mobility
- Exercises in the range of motion should be induced as soon as possible. The patient may not have pain when he is doing the exercises eg. rotation exercises for the thoracic spine. Do not invoke pain.
- Progressive stretches. They can begin with simple mobility exercises as tolerated Stretching of the M. pectoralis major can be helpful (stretch the M. pectoralis major, stand in a corner for 10 seconds with both of your hands against the wall (like when you do a push-up)repeat it a few times a day for 1 or 2 minutes).
- Mobilization of the spine and ribs to improve thorax mobility and reduce symptoms. In the painful area, they can use transcutaneous electrical stimulation and electroacupuncture. The acupuncture needle is placed within the involved spinal segment. Then low-frequency electrical currents are applied to the inserted needle.
- Dry needling: Musculoskeletal chest wall pain has traditionally been a difficult area to evaluate and treat. Dry needling in the hands of properly trained providers may aid in the diagnosis and treatment of focal chest wall syndromes






One Comment