Pseudobulbar Palsy : Cause, Symptoms, Physiotherapy Treatment
What is Pseudobulbar Palsy?
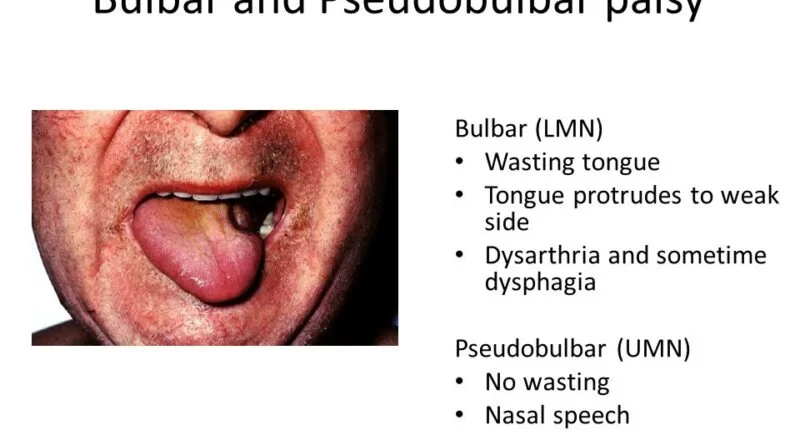
Pseudobulbar palsy is a form of upper motor neuron disease in which bulbar innervated muscles are affected. This palsy is caused by bilateral supranuclear lesions involving the corticobulbar pathways. Most common types of bulbar palsy are progressive bulbar palsy (PBP) and pseudobulbar palsy.
Most common symptoms are dysphagia, nasal regurgitation, choking, and drooling. However the tongue may be strikingly become immobile (slow tongue movements), atrophy and fasciculations do not develop. There is mostly an exaggerated jaw jerk, a hyperactive gag reflex and frontal release signs such as snout and suck reflexes.
Pseudobulbar palsy mostly occurs in multiple cerebral infarctions related condition such as encephalitis, MS, trauma, cerebral anoxia, primary lateral sclerosis, or other disease in which bilateral corticobulbar tract lesions affected.(3-5)
Patients may keep food in the mouth for prolonged periods.
It is also called Pseudobulbar affect, Pseudobulbar paralysis, Spastic bulbar palsy, and supranuclear bulbar paralysis.
Related Anatomy :
Damage of descending white matter pathways can lead to abnormal pseudobulbar affect and can be seen in Multiple Sclerosis patients and other cortical-related conditions.
Pseudobulbar affect shows sudden crying or laughter that is not associated with underlying emotions of sadness or happiness. Pseudobulbar affect has also been termed symptomatic laughing or crying.
Pseudobulbar palsy is upper motor neuron weakness of the muscles innervated by the 9th, 10th, and 12th cranial nerves, while in bulbar palsy is a lower motor neuronal weakness of these muscles.
Glossopharyngeal nerve (9th cranial nerve)
Sensory: Innervates the oropharynx, carotid body and sinus, posterior 1/3 of the tongue, middle ear cavity, and Eustachian tube.
Special sensory: somatic sensory and bitter/sour taste sensation to the posterior 1/3 of the tongue.
Parasympathetic: Provides parasympathetic innervation to the parotid gland.
Motor: Innervates the stylopharyngeus muscle of the pharynx
Injury leads to loss of taste in posterior third tongue and difficulty in swallowing
The vagus nerve (10th cranial nerve)
The vagus nerve carries afferent fibres from the root of the tongue and epiglottis.
Motor function- innervates the majority of the muscles associated with the pharynx and larynx.
Efferent fibres for the gag reflex
There are somatic and visceral components to the sensory function of the vagus nerve.
Somatic refers to sensation from the skin and muscles. This is provided by the auricular nerve, which innervates the skin of the posterior part of the external auditory canal and external ear.
Viscera sensation is that from the organs of the body.
Hypoglossal nerve (12th cranial nerve)
The Hypoglossal nerve is the twelfth cranial nerve, and innervates all the extrinsic and intrinsic muscles of the tongue, except for the palatoglossus which is innervated by the vagus nerve.
It is a nerve with mainly a motor function.
Isolated damage to the nerve is uncommon but it may be caused by tumours, wounds, sarcoid, multiple sclerosis (MS), presence of an ectatic vessel in the hypoglossal canal the most common disease affecting it is motor neuron disease (MND)
if the damage is to the nerve pathway (an upper motor neuron lesion) the tongue will curve away from the side of damage, due to action of the affected genioglossus muscle, and will occur without fasciculations or wasting.
These may lead to difficulty in chewing, talking, and swallowing and may also cause drooling.
Vertebrobasilar stroke may affect both hypoglossal nerves, facial nerve, and trigeminal nerves resulting in tight oral musculature, dysarthria, and difficulty eating and chewing.
Causes of Pseudobulbar palsy
Following are the list of upper motor neuron disease-related condition in which Pseudobulbar palsy can be associated.
- Stroke that affected the bilateral internal capsule are the most common and may cause acute mutism with paralysis of the bulbar and facial muscles
- If it is also associated with severe limb weakness then this is called “locked-in” syndrome
- Multiple sclerosis (MS)
- Parkinson’s disease
- Motor neurone disease (MND)
- Amyotrophic lateral sclerosis (ALS)
- Alzheimer’s disease
- Progressive bulbar palsy
- High brainstem tumors
- Traumatic Head injury
Symptoms of Pseudobulbar palsy:
- Increased reflexes – gag reflex and jaw jerk
- Spastic tongue – small, tight tongue that cannot be protruded
- “Donald Duck” speech
- uncontrolled emotions such as frequent, involuntary, and uncontrollable crying or laughing that are exaggerated
- bilateral upper motor limb signs
- sleep disturbances or a loss of appetite
Differential diagnoses:
- Myasthenia gravis
- Lyme disease
- botulism
- Brown–Vialetto–Van Laere syndrome
- Worster-Drought syndrome or congenital suprabulbar paresis
- X-linked bulbospinal muscular atrophy (Kennedy’s disease)
Diagnosis:
Diagnosis of Palsy mostly By Doctors such as Neurologist, Neuro physicians, neuropsychologists, and psychiatrists.
This condition is mostly diagnosed wrongly such as depression, bipolar disorder, generalized anxiety disorder, schizophrenia, a personality disorder and epilepsy. To help your doctor determine if you have PBA, share specific details about your emotional outbursts.
Imaging studies are MRI, CT Scan, and X-Ray of the Brain or Head depending upon cause, and symptoms. The doctor also recommended Nerve conduction studies (NCV), Electromyography (EMG).
Treatment of Pseudobulbar Palsy
The goal of treatment for pseudobulbar palsy is to reduce associated symptoms that depend upon symptoms, cause, and Diagnosis.
Medical treatments are:
Symptomatic Medical Treatment.
Dysphasia is improved with oromotor exercises, pharyngeal tactile stimulation, tongue retraction exercises, effortful swallowing exercises, the Mendelsohn maneuver, and shaker exercises.
Percutaneous endoscopic gastrostomy tube (PEG) may be recommended by Doctor if you have severe dysphagia or recurrent aspiration pneumonia.
Antidepressants: Antidepressants, such as tricyclic antidepressants (TCAs) and selective serotonin reuptake inhibitors (SSRIs), can help reduce the frequency and severity of your uncontrolled emotional episodes.
Dextromethorphan hydrobromide and quinidine sulfate (Nuedexta) (approved by the Food and Drug Administration)
Physical therapy and occupational therapy also can help you to improve day-to-day activity.
Speech therapy also helps to improve your speech (dysarthria). Mainly vocal cord adduction exercises and respiration-phonation training can be beneficial.
Rehabilitation: Rehab. Team including a physician, physical therapist, occupational therapist, speech therapist, social worker, respiratory therapist, and nurse caseworker help you to improve your overall Rehabilitation.






One Comment