Patello-femoral Pain Syndrome: Treatment & Exercise
Introduction of the Patello-femoral pain syndrome
- This syndrome produces pain at the front of the knee, around the kneecap means patella.
- This syndrome is also known as the runner’s knee or jumper’s knee.
- This syndrome is more common into the people who have to participate into the sports like as the running & jumping.
- This pain is also produced when the patient walks up, run, sit for a long period, squat & downstairs.
- It is most common in females & young adults.
- The patient also feels difficulty in everyday activities.
- Many things contribute to the development of this syndrome.
- For as the alignment of the kneecap & overuse of vigorous athletics & training is also significant factors.
- This Symptom is relieved by the conservative treatment & therapeutic exercise in this syndrome Risk factors are trauma, weak quadriceps muscle & increased training.
- Diagnosis of this is based on the symptoms & examination.
- Differential diagnosis of this syndrome is chondromalacia patellae & patellar tendinopathy.
- The pathophysiology of this syndrome is thought to be different
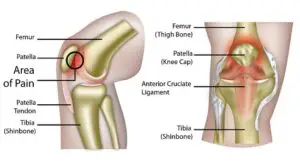
Anatomy of the Patello-femoral pain syndrome :
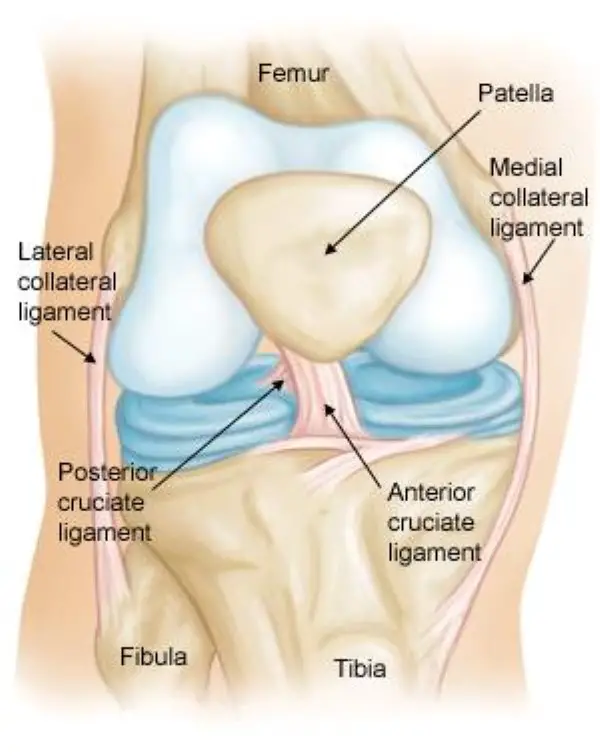
- The knee joint is the largest joint in the body.
- it is one of the most complex joints of the body.
- It is made up of three bones.
- The lower end of the femur = thighbone.
- The upper end of the tibia = shinbone.
- The patella =kneecap.
- The knee joint is become form 2 joint.
- Tibiofemoral joint.
- Patellofemoral joint .
- Ligaments & tendons of lower legs are connect onto the femur.
- Many Muscles are connected to the bones by the tendons.
- Quadriceps tendon = it is connect to the muscles in the front of the thigh to the patella.
- The patellar reticulation = it is attached of to the tibia for to help to the stabilize of the patella.
- Several structures of the knee joint is become to movement easier.
- Slippery substance of the knee joint is called the articular cartilage .
- Which is covers to the ends of to the femur, trochlear groove, & patella [ underside ].
- It is helps into the bones for glide smoothly against to each other during to movement .
- Synovium it is also a thin lining of to the tissue which is covers of to the surface of to the joint.
- It is produces a small amount of the fluid which is lubricates to the cartilage.
- It is perform as the cushions of the kneecap & acts to as a shock absorbed.
Epidemiology /Etiology of the Patello-femoral pain syndrome :
- This syndrome is due to mostly of a patellar trauma but it is also due to many other factor Patellofemoral joint overuse & overload abnormalities of the anatomical or bio-mechanical , muscular weakness, dysfunction or imbalance .
- It’s more likely that PFPS is worsened and resistivity to treatment because of several of these factors.
- One of the main causes of this syndrome is to patellar orientation & alignment.
- When to the patella in to the different orientation, it is give to the glide more to one side of to the femur apply to the over pressure onto the part ofto the femur.
- It is produce to the pain, irritation or discomfort .
- Patellar orientation is varies from to the one patient to the another .
- Also different the left to right knee in to the all the patients & it is a result of the anatomical malalignments .
- Patellar deviation is a cause of muscular imbalances & biomechanical abnormalities which are causes of this syndrome.
- It is also due to the knee hyperextension.
- Lateral tibial torsion.
- Genu valgum or varus .
- Increased Q-angle.
- Tightness into the iliotibial band, hamstrings or gastrocnemius.
Muscular etiologies of the Patello-femoral pain syndrome :
| NO. | Etiology | Pathophysiology |
| 1 | Weakness in to the quadriceps | It is do the adversely affect on the the PF mechanism. Strengthening is to advice . |
| 2 | Weakness in to the medial quadriceps | It is allows to the patella for to the track too far the laterally. need to the Strengthening of the VMO |
| 3 | Tight of the iliotibial band | It is places the excessive lateral force on to the patella & also externally rotate to the tibia, So that the upsetting the balance of to the PF mechanism. it is lead to the excessive lateral tracking of to the patella. I |
| 4 | Tight of the hamstrings muscles | It is places to the more posterior force on to the knee, so that the causing of the pressure between of to the patella & the femur. |
| 5 | Weakness of the tightness in to the hip muscle | Dysfunction of to the hip external rotators which is results into the compensatory for the foot pronation. |
| 6 | Tight of the calf muscles | It is lead to the compensatory of the foot pronation & it can increase to the posterior force on to the knee. |

Causes of the Patello-femoral pain syndrome:
- Overuse of the knee joint.
- The during to the Running, jumping, or sports it is puts repetitive stress on the knee joint.
- Weaknesses & Muscle imbalances.
- Muscles are not properly aligned onto the kneecap
- The trauma to the kneecap is like dislocation & fracture.
- After the Surgery of the knee cap, mostly in the particularly repair of the anterior cruciate ligament.
- Use to the improper sports for the training techniques & equipment
- Changes into footwear the playing surface
- Patellar Malalignment
- Abnormal tracking of the kneecap into the trochlear groove.
- Patient wear to the poorly fitted footwear
- Patient is also present with the excessive genu valgum
- Internal knee derangement
- Osteoarthritis of the knee
- Bony tumors into the around the knee
- some point which increases the pressure on the patella.
- Increased levels of physical activity
- Malalignment of the patella which is moves through to the femoral groove
- imbalance of the Quadriceps muscle
- Tight to the anatomical structures like the reticulum or iliotibial band
Symptoms of the Patello-femoral pain syndrome :
- It is a dull & aching pain into the front of the knee.
- Pain begins with the gradual, mostly activity-related pain
- This pain is like as diffuse vague pain around the kneecap [peripatellar] & localized pain is produced behind the kneecap[ retropatellar].
- Pain is aggravated when the patients
- During the Walking
- Down to the stairs
- Kneeling
- Squatting
- Sit with a bent knee for long periods of time
- Pain is also produced during the exercise.
- Pain is produced in the front of the knee after sitting for a long period of the time with to the kneesbent.
- This pain is reduced during the knee flexion.
- Like as the into the movie theater &during to tralling of the airplane.
- Popping or crackling sounds are produce in to the knee during to the climbing stairs & during to the standing up form to the prolonged sitting.
- Mild swelling is present
sign for to the pain of this syndrome:
- Mostly the pain is produced around the patella like a circle
- This is checked by to the place the hands over to the anterior patella
- This sign is called the circle sign
- Pain is also produced during prolonged sitting
- This sign is called the movie sign & theater sign
Diagnosis of the Patello-femoral pain syndrome:
X-rays:
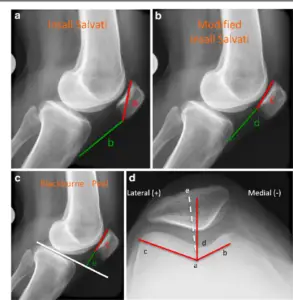
- x-ray shows the outer damage of the bones which is that make up onto the knee.
Magnetic resonance imaging (MRI) scans :
- It provides the clear images of the body’s soft tissues
- The Doctor advises doing this MRI when the symptoms do not improve form with physiotherapy & home exercise.
Differential diagnosis of the Patello-femoral pain syndrome :
- Referred pain from the hip joint.
- Sinding-Larson-Johansson syndrome
- Chondral lesions
- PCL injury/ruptur
- Chondromalacia Patellae
- Chondral lesions
- Osteoarthritis in the knee
- Hoffa’s pad syndrome
- ACL (anterior cruciate ligament) tear
- Medial overload syndrome
- medial meniscus tears
- Patellar tendinitis
- Referred pain from lumbar spine
- medial meniscus tears
- IIiotibial band friction syndrome
- Popliteal Cyst (Baker’s Cyst
Treatment of the Patello-femoral pain syndrome
Medical treatment:
- Give the patient anti-inflammatory medication like ibuprofen or naproxen.
- Give the Glycosaminoglycan polysulfate (GAGPS) it inhibits the proteolytic enzymes& increases the synthesis or degree of the polymerization of the hyaluronic acid into the synovial fluid.
Nonsurgical Treatment:
- Apply to the RICE method.
- Rest = Avoid putting the weight onto the painful knee.
- Ice = Use the cold packs for 20 minutes for in one time & perform for several times in a day.
- ice pack is not apply direct on to the skin.
- Compression = To prevent form additional swelling lightly wrap the knee with an elastic bandage
- Leaving to hole into the area of the kneecap.
- Make sure that the bandage is not to fits tight & not produce the additional pain.
- Elevation =if the possible, rest with the knee raised up higher than to the heart.
- Specific exercises for to the improve of the range of motion, strength, & endurance.
- Also do the Core exercises.
Orthotics:
- In the orthotics give the patient Shoe inserts which is help for the align & stabilize the foot & ankle.
- It also takes the stress off of the lower leg.
- Other one thing is also used which is custom-made for the foot which is known as the off the shelf.
Surgical Treatment:
- This treatment is very rarely needed in this syndrome.
- It is done only for the severe cases when do not respond to the nonsurgical treatment.
Arthroscopy:
- During the arthroscopy
- Surgeon is a inserts to a small camera , which is known as the arthroscope, into the knee joint.
- Camera is a displays pictures onto a television screen.
- Then the surgeon uses the images for to the guide miniature for the surgical instruments.
Debridement:
- In some cases, removing the damage to the articular cartilage from the surface of the patella provides pain relief.
Lateral release:
- If the lateral retinaculum tendon is too tight which is enough to pull the patella out of the trochlear groove,
- So that the lateral release procedure is loose to the tissue & correct to the patellar malalignment.
- After that, the short surgical video demonstrates the arthroscopic lateral release which is inside the knee.
- It is performed by a single procedure but sometimes it is performed as part of the larger surgery to treat a painful & unstable kneecap.
Tibial tubercle transfer :

- In some cases, it is necessary to realign the kneecap by moving the patellar tendon, which is along with a portion of the tibial tubercle, which means the bony prominence on the tibia.
- In this producer traditional open surgical incision is required
- Then to the doctor is partially or totally detaches of to the tibial tubercle so that the bone & the tendon is moved toward the inner side of the knee.
- Then piece of the bone is the reattached on to the tibia using the screws.
- In the most of cases, this transfer is allows for to the better tracking of the kneecap in to the trochlear groove.
Function Measures of the Patello-femoral pain syndrome :
- 10-point of the numeric pain rating scale
- Lower Extremity Functional Scale (LEFS)
The numeric pain rating scale:
- This scale range is from ‘0’ to 10.
- 0 means no pain.
- 5 means moderate pain.
- 10 means worse pain.
Lower Extremity Functional Scale (LEFS)
- The scale measures the patient’s ongoing progress, initial function & outcome of a wide range of lower-extremity conditions.
- In the scale, the therapist asks the question of the Patient about the difficulty in the activities.
- Difficulty in rating the activity.
- Unable to in the Perform Activity.
- Bit of the Difficulty.
- Moderate to the Difficulty.
- Little Bit of the Difficulty.
- No Difficulty with the activity.
Physiotherapy Examination of the Patello-femoral pain syndrome:
- For the knee pain therapist apply to the gently press & pull on to in front of the knees & kneecaps.
- Therapist is also ask to patient for perform to the many activities like as the squat, jump, or lunge .
- Therapist check to the patellar tracking.
- During the examination, your doctor will check your knee for problems in patellar tracking.
- Therapist is also check the Alignment of the lower leg & position of the kneecap.
- Therapist is check the Knee stability & ROM of the knees or hips.
- Therapist check the tenderness onto the kneecap.
- Therapist also check the strength of the muscles of the knee or hip.
- Therapist is check the Q-angle, J-sign & lateral hyper mobility,
- Tightness of the heel cord & flexibility of the feet.
- Patient is also examine the gait.
Special test of the Patello-femoral pain syndrome:
Patellar apprehension test:
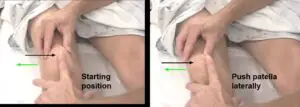
- Into the lateral instability which is assessed by the patellar apprehension test.
- This test is positive when the pain or discomfort is associated with the lateral translation of the patella.
Active Instability Test:
- It is a check of knee pain during stair climbing.
Clarke’s test:
- Pain with prolonged sitting.
- Pain is also felt during the squatting.
Stretching of the Patello-femoral pain syndrome:
Quadriceps stretch:

- The starting position is standing.
- Stand with the left hand resting gently on something sturdy, like a piece of furniture.
- Then Pull the right foot toward the buttocks & grasp the top of the right foot with the right hand.
- Point to the right knee toward the floor for the feel a stretch into the front of the leg.
- Hold the stretching position for the 20 to 30 seconds.
- Then Release to the stretch & repeat on to the other leg.
- Do the exercise for the 3 session per day.
Lunging Hip Flexor Stretch:

- The starting position is kneeling.
- Kneeling on to the left knee
- keep to the right shin on the ground.
- If the find to the ground is tough, get onto the back leg & try to stretch onto the yoga mat.
- Move the right leg back to the behind of the body.
- Keep to the right foot facing towards the ceiling.
- Put both hands on the right knee then push the body forward.
- Keep the torso & head in alignment.
- Patient is feel to the stretch in the hips, left leg.
- Hold the position for 20 seconds.
- Repeat the stretch the 3 times
- Do the 3 sessions per day.
Hamstring Stretch in supine:

- The starting position is the supine.
- Lie down on the back.
- Extend the right leg form to the front of the body.
- Bend to the left leg.
- Wrap around to the hands around of to the back & left thigh
- Then pull off to the leg slowly toward the patient’s can
- Hold for 30 seconds.
- Repeat the stretch for the 3 times.
- Do the 3 sessions per day.
Wall Hamstring Stretch:
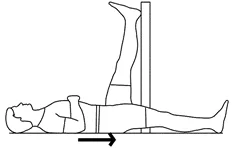
- The starting position is the supine.
- Lie onto the floor with the back facing towards the wall.
- Scoot the body and touch the glutes on the wall.
- Place one leg on the wall & try to extend the leg.
- Hold for 30 seconds.
- Repeat the stretch for the 3 times.
- Do this stretching 3 sessions per day,
Iliotibial Band Stretch:
Prevention
Knee pain can occasionally just appear. However, a few actions could lessen the suffering.
Build strength:
Having strong hip and leg muscles aids in maintaining knee balance during exercise. Avoid deep squats when lifting weights.
Move safely
Consult a physical therapist about proper jumping, running, and turning activities. The muscles surrounding the hips need to be strengthened in particular. This will prevent your knee from buckling inward during squats, leap landings, and step-downs.
Lose excess fat:
Reducing weight can help ease the strain on your knees if you are overweight.
Get warmed up: Warm up with a little exercise for five minutes or so before running or engaging in any other type of exercise.
Stretch Regularly: Use mild stretching techniques to increase flexibility.
Gradually Increase weight and Repetition of exercises. Don’t start working out more often all at once.
Be mindful of your footwear. Put on shoes that are appropriate for the activity and that fit nicely.
Prognosis
Most patients with patellofemoral pain syndrome get well using simple home treatments like the RICE technique. Physical therapy helps a lot of patients regain full function of their knee.
Epidemiology
Anterior knee pain in outpatients is most frequently caused by patellofemoral pain syndrome. Particular populations—runners, bikers, basketball players, young athletes, and females—are particularly vulnerable to primary PFPS.
In teenagers, having a higher BMI did not substantially raise the chance of developing PFPS. Adults with PFPS had a greater BMI than adults without it, though. Because the pain associated with PFPS causes people to become less active, it is hypothesized that having a higher BMI is linked to less physical activity in these individuals. Nevertheless, no long-term research can demonstrate that BMI can predict the onset or course of the illness.
FAQ
How do you fix patellofemoral pain syndrome?
To fix patellofemoral pain syndrome:
Cold packs
Rest with Elevating the leg
Compression knee wrap
Physical Therapy
Medicines eg. ibuprofen
Stretching exercises
Strengthening exercises
Arch support in shoes
Will patellofemoral syndrome go away?
Up to 90% of patients totally heal from patellofemoral pain and are able to return to their pre-painful activities. Most active individuals react well to nonsurgical interventions.
How should I sit with patellofemoral pain syndrome?
With your wounded leg extended in front of you and your upper thigh muscles relaxed, take a seat. Using your thumb and index finger, lightly press your kneecap down toward your foot.
Is walking good for patellofemoral syndrome?
By performing stretching and strengthening activities, you can reduce PFPS. He suggests doing five to seven minutes of gentle exercise, such as walking or stationary cycling, to warm up your muscles first.
Can you fully recover from patellofemoral syndrome?
The majority of patellofemoral syndrome cases respond well to conservative treatment, which includes bracing, a regular physical therapy program, stopping activity that triggers discomfort and inflammation for four to eight weeks, and using oral or topical NSAIDs.
How long is patellofemoral recovery?
Patellofemoral pain syndrome recovery can take a long time. When using non-surgical treatment, recovery typically takes six weeks or longer; however, if surgery is necessary, recovery times may increase.
Can I exercise with patellofemoral syndrome?
Regaining movement and strength is crucial following any patellofemoral knee pain. This will assist with tissue repair and enable you to resume your activities. It could take some time for you to get back to your regular workout routine, and at first, results might not be noticeable right away.
What happens if patellofemoral is not treated?
Patello-femoral dysfunction can exacerbate anterior knee discomfort if left untreated. It may also cause issues when playing sports. Alternative knee problems might result from weak hip and core muscles, poor leaping form, or poor running form.
What is the best exercise for patellofemoral pain?
You can either extend or bend your arm to rest your head on it. To balance your upper body, place the hand of your other arm on the floor in front of your belly. Raise your front leg up and toward the ceiling, hold it there for a short while, and then bring it back down. Do this drill ten to twenty times.






9 Comments