Iliopsoas Bursitis
What is an Iliopsoas Bursitis?
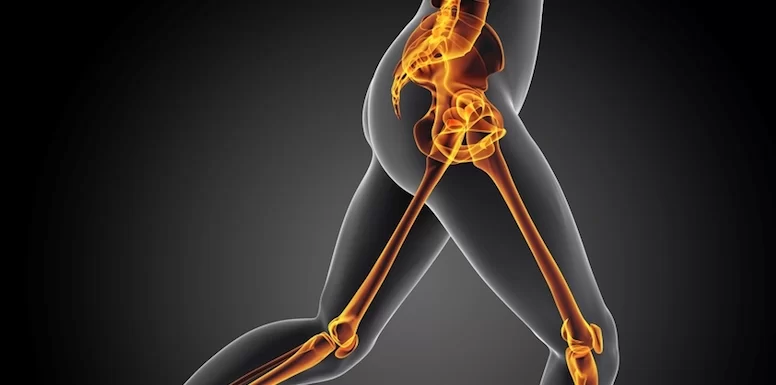
Iliopsoas bursitis is an inflammation of the bursa located beneath the iliopsoas muscle. This muscle is located in front of the hip. A bursa is a fluid-filled sac between bones, muscles, tendons, and skin. It provides a cushion between tissue to decrease friction and irritation.
Definition/Description
A Bursitis is an inflamed bursa.
The inflammation can be a result of friction from the overlying tendons.
A bursa is mostly flattened and is filled with a thin layer of synovial fluid.
It appears for example at a junction of a tendon on the bone.
The iliopsoas bursa separates the muscle or tendon from bone and facilitates movement by reducing friction between the anterior hip capsule and the iliopsoas.
The iliopsoas bursitis is one of the affections related to anterior hip pain.
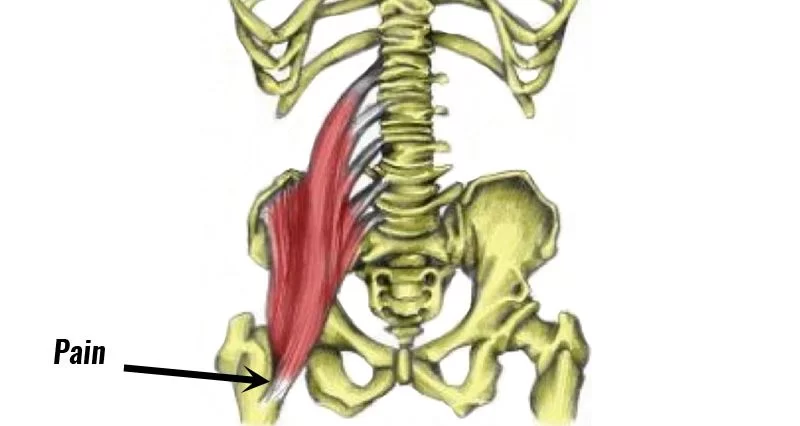
Clinically Relevant Anatomy
The iliopsoas bursa is the largest bursa of the human body and is bilaterally present in 98% of adults.
This bursa is bounded by the musculotendinous junction of the M. iliopsoas (anteriorly) and by the fibrous capsule of the hip (posteriorly).
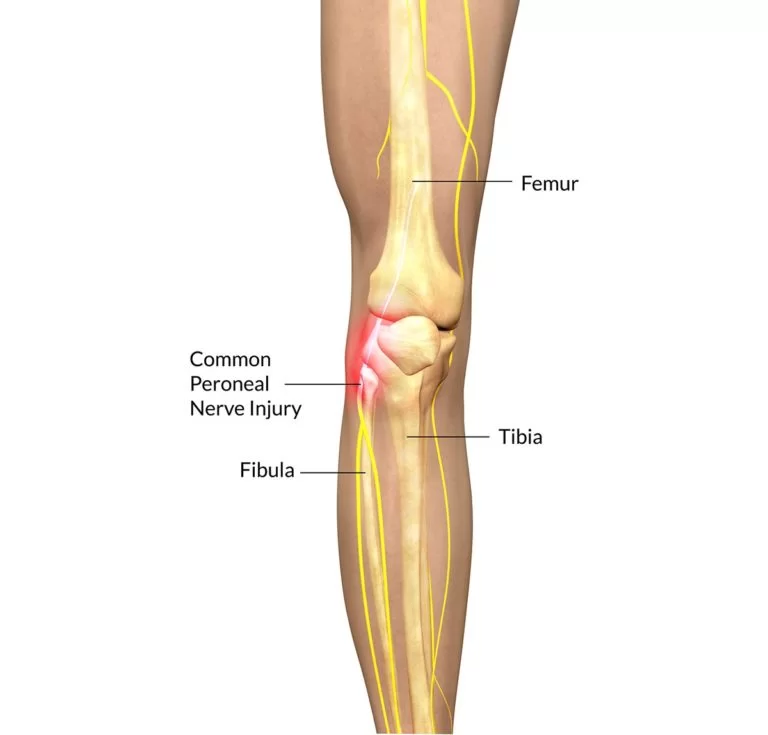
It extends from the inguinal ligament superiorly to the lesser trochanter inferiorly and is flanked by the femoral vessels (medially) and the femoral nerve (laterally).
The bursa is always collapsed, when in healthy condition.
In some situations, the bursa is enlarged and contains fluid.
When enlarged, it may cause a variety of symptoms such as pain, and immobility.
Epidemiology /Etiology
Iliopsoas bursitis is mainly caused by certain types of arthritis such as rheumatoid arthritis and psoriatic arthritis, acute trauma, and overuse injury. When an acute or chronic occupational trauma incurred during sports activities, bursitis is likely the result of multiple mini-traumas caused by vigorous hip flexion and extension.
Iliopsoas bursitis is commonly seen in individuals participating in strength training, rowing, uphill running, and competitive track and field.
There are a few theories concerning the origin of symptoms of iliopsoas bursitis.
One of them points out that when the hip is in flexion, both the iliopsoas muscle and the anterior part of the bursa move away from the hip joint.
If the hip is to be hyperextended suddenly, there is a great tension that stretches the muscle and the bursa.
This stretching traumatizes the bursa.
Another theory hypothesizes that when a flexed, abducted, and externally rotated hip, with iliopsoas bursitis, is brought in an extension, it causes an interruption of the lateral to medial movement of the iliopsoas tendon.
This results in a painful snapping of the tendon over the femoral head, and over the anterior hip capsule.
Inevitably, iliopsoas bursitis and tendinitis are interrelated, where inflammation of the one will result in inflammation of the other because of their close proximity. In their presentation, etiology, and treatment, the two conditions are almost identical. Together it is called the iliopsoas syndrome.
Patients with rheumatoid arthritis can also suffer from iliopsoas bursitis. Joint synovium is the main target of rheumatoid arthritis, but sometimes, synovial tissues of tenosynovium and bursae, are also involved. This results from the inflammatory process in the hip joint, extending into the iliopsoas bursitis. This kind of bursitis mainly affects young adults. It occurs slightly more often in women than in men.
Causes:
- A direct blow to the iliopsoas bursa from falling on the outside of the hip or on the buttocks can produce inflammation and irritation.
- A fall onto the hip or iliopsoas bursa.
- Constant pressure on the iliopsoas bursa from lying on that side.
- Repeated stress or friction injury as the tendon rubs over the iliopsoas bursa during activity.
- Weakness of the muscles over the iliopsoas bursa.
- Complications from rheumatoid arthritis, osteoarthritis, or gout.
- Infection of the iliopsoas bursa.
- Tightness of the structures of the hip like the psoas hip flexor, iliotibial band, and hamstrings.
- Iliopsoas bursa can become swollen as a response to other hip conditions.
Characteristics/Clinical Presentation
- Pain is felt in the anteromedial aspect of the thigh
- Pain radiated into the knee, leg, and lower back.
- Tenderness in the upper quads (M. Quadriceps).
- A snapping sensation at the front of the hip.
- Pain develops during walking or specific movements like crossing the legs.
- Pain on hip flexion resisted as well as passive.
- Pain on internal rotation or passive hyperextension.
- Stiffness or pain after a rest or in the mornings.
- Pain is worse while performing activities.
- Rest can relieve the pain.
Differential Diagnosis
Several joint diseases can cause distension: Osteoarthritis, Rheumatoid arthritis, Avascular necrosis, Pigmente villonodular synovitis, Synovial chondromatosis, Gout, Chondrocalcinosis, Trauma, Lupus erythematodes, Pyogenic infection, Snapping hip.
Differential diagnosis of anterior hip pain by anatomical structure:
- Joint
- Osteoarthritis
- Inflammatory synovitis
- Loose bodies (chondral, osteochondral, ossified, non-ossified, fibrous, foreign)
- Infection (septic joint)
- Crystal-induced synovitis (gout)
- Labral tears
- Bone
- Femur
- Stress fracture
- Avascular necrosis of femoral head
- Bone tumour
- Infection
- Femoroacetabular impingement (two types: cam impingement occurs from an abnormal head junction of the femur, pincer impingement is because of over-coverage of the acetabulum)
- Pelvis
- Hip fracture
- Stress fracture
- Osteitis pubis
- Muscle, tendon, bursa
- Iliopsoas bursitis and tendinitis
- Iliopsoas strain
- Rectus femoris strain
- Tight iliotibial band
- Gluteus medius and minimus problems
- Capsular laxity causing instability (due to traumatic dislocation or overuse)
- Vasculature
- Aneurysm
- Arteriovenous malformation
- Pelvic mass
- Gastrointestinal causes (e.g. hernia)
- Genitourinary causes (e.g. ureteral stone)
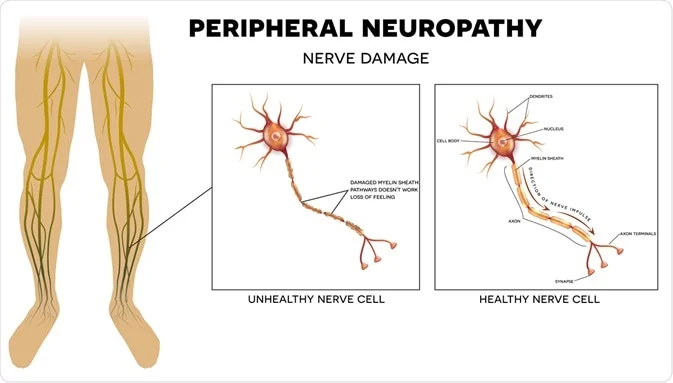
- Nerve
- Obturator nerve entrapment
- Myalgia paraesthetica
- Referred from the lumbar spine (L1, L2)
Diagnostic Procedures
Iliopsoas bursitis is often underdiagnosed due to its unspecific symptomatology. Careful and deep palpation in the femoral triangle medial or lateral to the femoral artery, with pressure applied on the bursa, will result in pain. To elicit a patient’s hip pain, a clinical maneuver is commonly used. It involves the extension of their flexed, abducted, and externally rotated hip where a tangible or audible ‘snap’ in the hip is almost always noted. It is also possible that the inguinal region is painful when palpating it. A known or suspected osteoarthritis, snapping hip syndrome, and a palpable inguinal or pelvic mass could raise the suspicion of an inflamed iliopsoas bursa and lead to further imaging examinations.
To exclude other possible hip problems, and to get a more realistic idea about the size of the bursa, a 3D image is recommended preferably an MRI scan. The MRI scan can distinguish the iliopsoas bursitis from other possible problems such as a tumor, a hernia, a hematoma, and an aneurysm. However, musculoskeletal ultrasound is the most cost-efficient way. Other frequently used options to exclude problems of the bone are an X-ray and a bone scan. Computed tomography or CT-scan is also a commonly used instrument.
An arthrography can determine instability and intra-articular pathology. A radiograph can also indicate an underlying problem of the hip, such as osteoarthritis and rheumatoid arthritis.
Examination
- Movement: The patient feels pain in the anteromedial aspect of the thigh when doing a hip flexion and internal rotation. There is a limitation in the range of motion (ROM) according to a non-capsular pattern. Flexion is lightly painful at the end of ROM. Sometimes pain can be felt at the end of ROM when extension or adduction is performed. The most painful movement is adduction with the hip in flexion.
- Palpation: bursitis can be palpated as an oedematous mass in the groin region. A palpable and/or audible snap can be present. Tenderness in the femoral triangle.
- Positive Thomas test
- Active resisted testing of the iliopsoas.
- (Dynamic) Ultrasound.
Medical Interventions:
- Avoiding the activities that produce pain or stress the iliopsoas bursa is the first line of treatment.
- RICE: (Rest, Ice, Compression, Elevation) should be used to reduce the stress on the iliopsoas bursa.
- NSAIDS (non-steroidal anti-inflammatory drugs) to reduce pain and inflammation.
- Needle drainage to remove excessive fluid from the iliopsoas bursa.
- Injection of steroids to reduce inflammation in iliopsoas bursa.
- In the case of infection, antibiotics may be prescribed,
- In severe recurrent conditions surgery to remove the iliopsoas bursa may be indicated.
Physiotherapy treatment for iliopsoas bursitis:
Physiotherapy is important in the treatment of iliopsoas bursitis. Your physiotherapist will be able to make a diagnosis and can use a number of treatment techniques to reduce your pain. Your physiotherapist will also be able to determine what structures are causing the inflammation within your iliopsoas bursa and address this as your pain settles to prevent a reoccurrence. Other treatment includes:
- Manipulation / Mobilisation
- Hydrotherapy
- Balance Exercises
- Electrotherapy
- Soft Tissue Treatment
- Joint mobilization of the lumber spine and hip to relieve stiffness and pain
- A progressive exercise program to improve strength, flexibility, and core stability
- Sport-specific exercises.
- This may include a graduated return to running program in the final stages of rehabilitation to recondition the hip flexor muscles for running in a safe and effective manner.
- Dry needling.
- Using crutches.
- Correction of abnormal biomechanics such as using orthotics.
- Exercises of the muscles and tendons surrounding the area to improve strength and flexibility.
- Manual Therapeutic Technique (MTT): hands-on care including soft tissue massage, stretching, and joint mobilization by a physical therapist to regain mobility and range of motion of the knee. The use of mobilization techniques also helps to modulate pain.
- Therapeutic Exercises (TE) include stretching and strengthening exercises to regain range of motion and strengthen muscles of the knee to support, stabilize, and decrease the stresses placed on the iliopsoas bursa and tendons of the hip joint.
- Neuromuscular Reeducation (NMR) to restore stability, retrain the lower extremity and improve movement techniques and mechanics (for example, running, kneeling, squatting, and jumping) of the involved lower extremity to reduce stress on iliopsoas bursa and tendons in daily activities.
- Modalities include the use of ultrasound, electrical stimulation, ice, cold laser, and others to decrease pain and inflammation of the iliopsoas bursa.
- A home program that includes strengthening, stretching, and stabilization exercises and instructions to help the person perform daily tasks and advance to the next functional level. Advice on how to modify the activity
Exercises for iliopsoas bursitis:
Hip Flexor Stretch Exercise for Iliopsoas Bursitis
This exercise is performed by placing the knee of the affected leg on the floor in such a way that the entire lower leg must lie directly on the floor. Now by bending the other knee lean forward slightly until a pain free stretch is felt in the front side of the thigh. Hold the position for about 30 seconds and release. Perform three times. Hip flexor stretch not only helps in stretching the iliopsoas muscle, but also improves stiffness of the joint of the hip.
Straight Leg Raises Exercise for Iliopsoas Bursitis
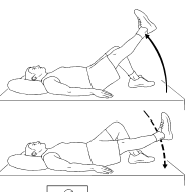
This exercise is performed by lying down on the back and straightening out the injured leg. Now place the foot flat of the healthy leg on the floor by bending at the knee. By tightening the thigh muscles gradually lift the injured leg in the upward direction until it reaches the level of the thigh on the opposite side. Hold the position for about one second and release. Repeat 10 times. Repeat the same exercise on the opposite leg. Straight leg raises help in strengthening the quadriceps muscle and iliopsoas present in the thigh.
Sitting Hip Flexion Exercise for Iliopsoas Bursitis
This exercise is performed by sitting on a chair or a table. Now by bending the right knee gradually lift the right knee in the upward direction as high as possible until a pain-free stretch is felt. Hold the position for about one second and release. Repeat 10 times. Repeat the same exercise on the left side.
Standing Resisted Hip Flexion Exercise for Iliopsoas Bursitis

This exercise is performed with the help of rubber resistance band. Tie the two ends of the band in order to make a loop. By placing the band around the leg of a table keep the foot into the loop and stand by keeping the body away from the band in such a way that the band loops around the front side of the ankle. Now by tightening the muscles of the hip gradually pull the foot in the forward direction. Perform 3 sets of 10. Standing resisted hip flexion also improves the strength of iliopsoas.
Gluteal Stretch Exercise for Iliopsoas Bursitis
This exercise is performed by lying down on the back. With the help of your hands, bring the knee towards the opposite shoulder until a mild to moderate pain-free stretch is felt along the buttocks or at the front side of the hip. Hold the position for about 15 seconds and release. Repeat four times ensuring there is no exacerbation of pain.
Prognosis:
In general, patients respond well to conservative treatment of hip bursitis (iliopsoas bursa). It is important that once the pain and inflammation are reduced, and motion and strength are restored, the patient gradually returns to full activities. Instruction in daily activities or sports performance is helpful to reduce the chance of a reoccurrence of bursitis. In most cases, a full return to activity will take from 2-6 weeks depending on the severity of the condition. As a preventive measure, individuals should:
Make modifications in work or daily activities to avoid prolonged pressure or unexpected blows on the iliopsoas bursa.
Maintain strength and flexibility to reduce stress on the iliopsoas bursa and tendons of the hip.
Avoid highly repetitive activities whenever possible