Moebius syndrome
What is Moebius syndrome?
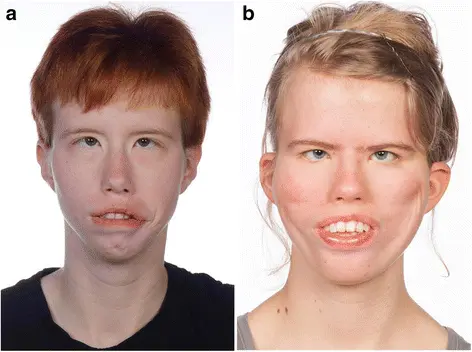
Moebius syndrome is an extremely rare birth neurological defect provoked by the absence or underdevelopment of the 6th and 7th cranial nerves, which control eye movements and facial expression. Congenital facial and abducens palsy was first depicted by Von Graefe (1880) and Moebius (1888), a German neurologist after whom the syndrome was later named.
Many of the other cranial nerves may also be concerned, including the 3rd, 5th, 8th, 9th, 11th, and 12th. The first symptom, present at birth, is an incapacity to suck. The condition may also affect the nerves responsible for speech, chewing, and swallowing. Other symptoms can also include feeding, swallowing, and choking problems; excessive drooling; crossed eyes; lack of facial expression; incapacity to smile; eye sensitivity; motor delays; high or cleft palate; hearing problems, and speech problems.
Kids with Moebius syndrome are unable to move their eyes back and forth. Reduced numbers of muscle fibers have been reported. Deformities of the tongue, jaw, and limbs, such as clubfoot and missing or webbed fingers, may also arise. As children get older, lack of facial expression and ineptitude to smile become the dominant visible symptoms. Approximately 30 to 40 percent of kids with Moebius syndrome have some degree of autism.
Other Names for This Condition
- Congenital facial diplegia
- Congenital ophthalmoplegia and facial paresis
- Mobius syndrome
- Moebius congenital oculofacial paralysis
- Moebius sequence
- Moebius spectrum
- Möbius sequence
Moebius syndrome also involves muscles that control back-and-forth eye movement. Affected people must move their heads from side to side to read or follow the movement of objects. Individuals with this disorder have a problem making eye contact, and their eyes may not look in the same direction (strabismus). Additionally, the eyelids may not shut completely when blinking or sleeping, which can result in dry or irritated eyes. Other characteristics of Moebius syndrome may include bone abnormalities in the hands and feet, weak muscle tone (hypotonia), and hearing loss. Affected kids often experience delayed development of motor skills (such as crawling and walking), although most eventually develop these skills. Moebius syndrome is not progressive, suggesting it does not get worse over time.
These two strict clinical criteria are:
- Congenital (occurring from birth), non-progressive genetic facial weakness
- Incapability to abduct (move the eye away from the nose) one or both eyes
Both measures must be present for a diagnosis of Moebius syndrome. These two symptoms may also be due to impairment in the facial nerve (cranial nerve 7) and the abducens nerve (cranial nerve 6), respectively. Some analysis studies have suggested that children with Moebius syndrome are more likely than unaffected children to have characteristics of autism spectrum disorders, which are a group of conditions described by impaired communication and social interaction. Yet, recent studies have questioned this association. Because individuals with Moebius syndrome have difficulty with eye contact and speech due to their physical differences, autism spectrum disorders can also be difficult to diagnose in these individuals. Moebius syndrome may also be associated with a somewhat improved risk of intellectual disability; yet, most affected people have normal intelligence.
There are four prominent varieties of Moebius syndrome:
- Group I, is characterized by small or absent brain stem nuclei that control the cranial nerves;
- Group II, characterized by loss and deterioration of neurons in the facial peripheral nerve;
- Group III, characterized by loss and deterioration of neurons and other brain cells, microscopic areas of impairment, hardened tissue in the brainstem nuclei, and,
- Group IV, is characterized by muscular symptoms despite a lack of lesions in the cranial nerve.
Pathogenesis of moebius syndrome
Moebius syndrome develops from the underdevelopment of the VI and VII cranial nerves. The VI cranial nerve regulates lateral eye movement, and the VII cranial nerve controls facial expression. The causes of Moebius syndrome are poorly understood. It is thought to result from a vascular disruption (temporary loss of blood flow) in the brain during prenatal development.
There can also be many reasons for vascular disruption leading to Moebius syndrome. Most cases do not emerge to be genetic. Nevertheless, genetic links have been found in a few families. A few maternal trauma may result in impaired or interrupted blood flow (ischemia) or lack of oxygen (hypoxia) to a developing fetus. Some issues are associated with a reciprocal translocation between chromosomes or maternal illness. In the majority of cases of Möbius syndrome in which autosomal dominant inheritance is suspected, sixth and seventh cranial nerve paralysis (palsy) appears without associated limb abnormalities.
The usage of drugs and a traumatic pregnancy may also be linked to the development of Moebius syndrome. The utilization of the drugs misoprostol or thalidomide by women during pregnancy has been linked to the development of Möbius syndrome in some cases. Misoprostol is employed to induce abortions in Brazil and Argentina as well as in the United States.
Misoprostol abortions are successful 90% of the time, indicating that 10% of the time the pregnancy continues. Studies show that the use of misoprostol during pregnancy increases the risk of developing Moebius syndrome by a factor of 30. While this is a dramatic increase in risk, the incidence of Möbius syndrome without misoprostol use is estimated at one in 50000 to 100000 births (making the incidence of Moebius syndrome with misoprostol usage, less than one in 1000 births). The usage of cocaine (which also has vascular effects) has been implicated in Moebius syndrome.
A few researchers have suggested that the underlying problem of this disorder could also be congenital hypoplasia or agenesis of the cranial nerve nuclei. Certain symptoms associated with Möbius syndrome may be caused by insufficient development of facial nerves, other cranial nerves, and other aspects of the central nervous system.
Oral or dental concerns
Neonatal
When a child is born with Möbius syndrome, there can also be a problem in closing the mouth or swallowing. The tongue could also fasciculate (quaver) or be hypotonic (low muscle tone). The tongue might be more extensive or more diminutive than average. There may be a low tone of the muscles of the smooth palate, pharynx, and masticatory system. The palate may be arched excessively (a high palate) because the tongue does not create a suction that would normally shape the palate down further. The palate may also have a groove (this may be partly due to intubation earlier on if it is for an extended period) or maybe a cleft (incompletely formed). The opening to the mouth might be small. Feeding considerations may evolve into a critical problem early on if adequate nutrition is difficult.
Primary dentition
The primary (baby) teeth commonly start arriving in by 6 months of age, and all 20 teeth may also be in by two and a half years of age. The eruption timing varies greatly. There may be an insufficient formation of the enamel on the teeth (enamel hypoplasia) that makes the teeth more powerless to caries (cavities). There may be missing teeth eruptions. If the infant is not closing down completely, the lower jaws become more noticeably deficient (micrognathia or retrognathia). The front teeth may not touch when the child closes down because the back teeth have over-erupted or because of incomplete formation of the maxilla. This condition is reached an anterior open bite and has facial or skeletal implications. The saliva may be thick, or the baby may have a dry mouth.
Transitional dentition
Between the age of 5 and 7, most kids start losing their primary teeth. Periodically, few primary teeth are slow to exfoliate (fall out), and the dentist may want to withdraw a primary tooth early to prevent orthodontic problems. Correspondingly, premature loss of immediate teeth may create orthodontic problems later on. When a tooth is lost prematurely, removable or fixed spacers may be required to prevent the shifting of teeth. Interceptive orthodontic therapy may also be initiated at this stage of development to assist with crowding or to help relate the upper and lower jaws. Consistent with an increased palate is a narrow arch shape of the upper teeth as they line up in the mouth. This may cause the upper front teeth to flare out and evolve more prone to fracture if accidentally hit. Interceptive orthodontics has an important role in these circumstances. Instruments that expand the upper arch tend to obtain the front teeth back into a more normal position. A few appliances could also even assist allow the front teeth to close to normal in an open-bite situation. The mouth and lips might tend to get dry with the Möbius patient. Lack of a sufficient oral seal (lips together) permits the gingiva (gums) to get dry and may get inflamed and irritated.
Permanent dentition
After the last primary tooth is failed, usually around the age of twelve, final orthodontic treatment can also be initiated. A patient that has not been capable to close or swallow well probably will have an open bite, deficient lower-jaw growth, a narrow arch form with crowded teeth, and upper anterior flaring of teeth. Orthognathic (jaw) surgery might be indicated. This should be completed in most circumstances before the smile surgery where the gracilis muscle is grafted to the face.
Causes of Moebius syndrome
Most patients of Moebius syndrome emerge randomly for unrevealed reasons (sporadically) in the absence of a family history of the disorder. The syndrome is detailed as Online Mendelian Inheritance in Man (OMIM). Sporadic mutations in PLXND1 and REV3L genes have also been identified in several patients and confirmed to cause a constellation of findings consistent with Moebius syndrome when introduced in animal models.
In rare cases, familial patterns have been reported. Most likely, Moebius syndrome is multifactorial, which means that both genetic and environmental factors recreate a few causative processes. It is conceivable that in additional cases there are different underlying causes (heterogeneity). In domestic cases, there is proof that Moebius syndrome is inherited as an autosomal dominant trait. Predominant genetic disorders occur when only a single copy of an abnormal gene is essential for the appearance of the disease. The abnormal gene can also be inherited from either parent or maybe the result of a new mutation (gene change) in the affected individual. The menace of passing the abnormal gene from the affected parent to offspring is 50% for every pregnancy regardless of the sex of the resulting youth.
The spectrum of findings in Moebius syndrome indicates a developmental defect of the hindbrain. Several different theories have been proposed to describe the cause of Moebius syndrome. One theory is the disorder is the result of diminished or interrupted blood flow (ischemia) to the developing fetus during pregnancy (in utero). Current research proposes that the deficiency of blood affects certain areas of the lower brainstem that contain the cranial nerve nuclei. This deficiency of blood flow could result from an environmental, mechanical, or genetic cause. Nevertheless, the cause of the syndrome stays inconclusive, and more basic and clinical research is necessary. Scientists are still investigating the causes of Moebius syndrome. Occasionally it is linked to mutations in distinctive genes, but it usually happens sporadically (no known reason or family link).
What you need to know
- Moebius syndrome is a kind of congenital facial paralysis or palsy.
- The condition usually involves both sides of the face.
- While researchers have not specified the cause(s) of Moebius syndrome, investigations suggest a combination of genetic and environmental risk factors.
- Treating Moebius syndrome may also need a team of doctors to address symptoms, including cleft palate, crossed eyes, and difficulties eating, speaking, hearing, or controlling facial expressions and functioning.
Signs and Symptoms of Moebius syndrome
The aberrations and severity of Moebius syndrome vary greatly from one person to another. The classically accepted diagnostic criteria include:
- facial paralysis or weakness involving at least one but usually both sides of the face (7th cranial nerve)
- Immobility of sideways (lateral) movement of the eyes (6th cranial nerve)
- preservation of vertical movements of the eyes. Less frequently, other cranial nerves, including the 5th, 8th, 9th, 10th, 11th, and 12th may be affected.
Clinical Presentation
Cranial Nerve VII Involvement
- Bilateral facial immobility or paralysis is the multiple noticeable symptoms and is often noticed very soon after birth, with the parents reporting incomplete eyelid closure during sleep and difficulty sucking (due to lack of lip seal).
- However, occasionally facial paralysis is not noticed for a few weeks or months until the baby’s inability to smile or the lack of facial movement with crying arouses the parents’ concern. In extremely rare cases facial paralysis is unilateral.
- As the juvenile grows, speech problems emerge due to the incapability to seal the lips for the labial consonants. Speech concerns are reported in 76 to 90% of patients with Möbius syndrome.
Cranial Nerve VI Involvement
- Abducens nerve palsies are noted in approximately 75% of patients and are some of the most distinctive features of the syndrome.
Cranial Nerve XII Involvement
- The hypoglossal nerve is the third most typically involved cranial nerve (CN) and is involved in approximately 25% of reported cases. Involvement of the hypoglossal nerves repeatedly leads to atrophy of the tongue.
- Patients may be unable to protrude their tongues beyond their lips because of this weakness. This involvement might result in paralysis and hypoplasia of the tongue, or fasciculations may be seen as a result of hypoglossal denervation. The ocular muscles are consistently involved when the tongue is affected.
Brachial Malformation
The brachial malformation is expected and can involve the following:
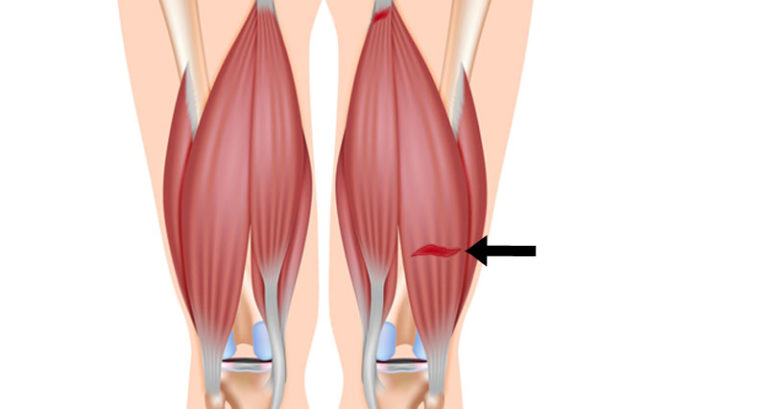
- CTEV – Talipes Equinovarus AKA Clubfoot, frequently bilateral, appears in almost one-third of patients
- Reports include hand malformations or congenital amputation of the hand
- In some cases, the involved hand is smaller than the other hand
- Syndactyly is not uncommon, and brachydactyly is commonly reported
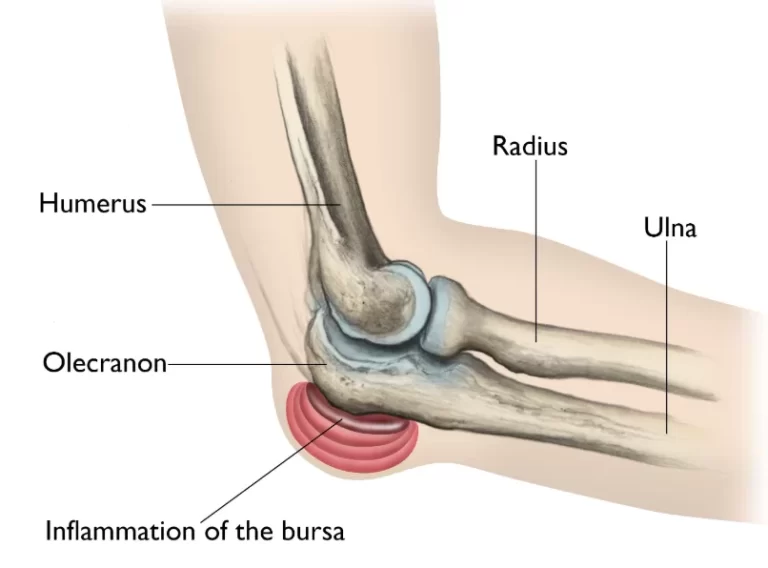
Other aberrations in the upper extremities include finger webbing and scarcity or hypoplasia of the radius, ulna, metacarpal, or phalanx
Motor Delay
- Many youngsters with this syndrome have some motor delay during infancy, although this is usually resolved after the first few years of life. One large Italian analysis published in 2016, found that these children often “exhibit development described by global delay at 1 year of age, motor, emotional and speech problems at 2 years of age, a trend toward normalization at 3 years of age but with weakness in hand-eye coordination, and finally accomplishing average results at 5 years of age.”
Poland Sequence
- A congenital condition called the Poland sequence, characterized by ipsilateral hand malformations and by the partial or complete absence of the pectoralis muscles and breast occurs with Möbius syndrome in approximately 15% of patients.
Other problems
- Several individuals with Moebius Syndrome have been found to have missing (or incompletely developed) trunk muscles; most often the trapezius and pectoral muscles, but other muscles which can be involved are the serratus anterior, latissimus dorsi, abdominal & intercostal muscles.
- Möbius syndrome has been associated with autistic behavior. Studies suggest that autistic symptoms are present in 30 to 40% of children and young adults with Möbius syndrome. The patient’s intelligence is usually normal, but mild mental retardation is thought to occur in approximately 10 to 15% of patients.
- Newborns with Moebius syndrome may also drool excessively and exhibit crossed eyes (strabismus). Because the eyes do not move from side to side (laterally), the kid is forced to turn the head to track objects. Babies who lack facial expression frequently are described as including a “mask-like” face that is especially obvious when laughing or crying. Affected infants can also have difficulties feeding, including problems swallowing and/or poor sucking. Corneal ulceration can also happen because the eyelids remain open during sleep.
- There are a wide variety of additional abnormalities. A few youngsters with Moebius syndrome have a short, malformed tongue and/or an abnormally small jaw (micrognathia). A Cleft palate may also be present. These irregularities contribute to feeding and breathing difficulties. Kids with cleft palate are predisposed to ear infections (otitis media). There may also be external ear anomalies including underdevelopment of the outer piece of the ear (microtia) or total absence of the outer portion of the ear (anotia). If the 8th cranial nerve is involved, there is likely hearing loss. Dental abnormalities are not uncommon. There is an improved risk of childhood cavities. Some affected children have problems with speech and delays in speech development.
- Skeletal malformations of the limbs appear in over half of children with Moebius syndrome. Lower limb malformations contain clubbed feet and underdevelopment of the lower legs; upper extremities may also have webbing of the fingers (syndactyly), underdevelopment or absence of the fingers, and underdevelopment of the hand. In a few children there can also be abnormal side-to-side curvature of the spine (scoliosis), and in approximately 15% of patients underdevelopment of the chest (pectoral) muscles and the breast on one side of the body also occur (see Poland-Moebius syndrome in the Related Disorder section below).
A few affected youngsters demonstrate a delay in attaining certain milestones such as crawling or walking, most likely due to upper body weakness; however, most children eventually catch up. Moebius syndrome infrequently is associated with a minor intellectual disability. Some juniors have been classified as existing on the “autistic spectrum”.
The identical relationship between Moebius syndrome and autism is unknown. A few studies have suggested that autism spectrum disorders occur with greater frequency in children with Moebius syndrome; other studies have not verified this and suggest that any such relationship is overstated. Moebius syndrome is frequently associated with a combination of social and psychological consequences. other symptoms such as chest wall abnormalities and crossed eyes.
The lack of facial expressions and the incapability to smile can also cause observers to misinterpret what an affected individual is thinking or feeling or intends. Although clinical anxiety and depression are not more typical in children and adolescents with Moebius syndrome, affected individuals may also evade social situations due to apprehension and frustration.
Moebius Syndrome Symptoms
People with Moebius syndrome experience:
- Weakness or whole paralysis of the facial muscles
- Difficulties with speech and routine drooling
- Incapacity to form facial expressions, including smiling, frowning, raising eyebrows, puckering lips, or closing eyes
- Cleft palate
- Dental problems
- Hand and foot concerns including club foot and missing or fused fingers (syndactyly)
- Hearing problems
- High palate
- Irritated and dry eyes
- Motor delays
- Poland’s syndrome (chest wall and upper limb abnormalities)
- Strabismus (crossed eyes)
How is Moebius syndrome diagnosed?
A healthcare provider analyzes Moebius syndrome based on clinical criteria. That means there are no detailed tests for the disorder. Diagnosis is based on a healthcare provider regarding specific symptoms during an examination.
To analyze Mobius syndrome, a child must have:
- Facial weakness or paralysis that has been attending since birth but does not get worse over time.
- Incapability to move one or both eyes outward or side to side (but can move the eyes up and down).
A healthcare provider can also perform tests to rule out other causes of facial weakness or paralysis. A diagnosis of Moebius syndrome is based on the characteristic signs or symptoms, a detailed patient history, and a thorough clinical evaluation. There are no diagnostic tests that establish a diagnosis of Moebius syndrome. A few specialized tests may be performed to rule out other causes of facial palsy.
Electromyography can be used to help determine whether a patient’s symptoms stem from birth trauma and are therefore NOT associated with Moebius syndrome. CT scanning or MRI of the brain may demonstrate bilateral calcifications in the regions of the CN VI nuclei, but this is not true for all cases of Moebius syndrome
What is the perspective of individuals with Moebius syndrome?
With proper medical care, people with Moebius syndrome usually have a normal life longing. This is particularly true if they do not have life-threatening complications in the foremost year of life. Although symptoms may also make life more demanding, many people with the condition live productive and meaningful lives.
What could I ask my child’s doctor about Moebius syndrome?
Contemplate asking your healthcare team the following questions:
- Which cranial nerves are affected?
- What specialists can assist with the signs and symptoms?
- Should I consider surgery for my child?
- Is there any reason I should seek prompt medical attention for my kid?
- Should my family get genetic testing or counseling?
How can my child best learn to cope with Moebius’s mouth?
Individuals with Moebius syndrome frequently live their whole lives, especially after treatment to correct or lessen the signs and symptoms. Yet, they may have various problems with self-esteem or the emotional aspects of the condition. It may assist to:
- Treat support groups to connect with other people with Moebius syndrome.
- Get engaged in the Moebius syndrome community through advocacy, fundraising, etc.
- Speak to a therapist (such as a counselor or psychologist).
Differential Diagnosis
- Abducens (CN VI) nerve palsy
- Congenital facial (CN VII) nerve palsy
- Brainstem syndromes
- Metabolic neuropathy
- Myotonic diseases
- Neuromuscular diseases
- Congenital neuropathies
- Congenital muscular dystrophy
- Duane syndrome
- Kallmann syndrome
- Poland anomaly
- Klippel-Feil anomaly
Treatment of Moebius syndrome
There is no distinct course of therapy for Moebius syndrome. Treatment is supportive and in conformity with symptoms. Your kid’s medical care will require a variety of specialists, including neurologists, ophthalmologists, plastic surgeons, otolaryngologists, and speech pathologists. Infants may also need feeding tubes or special bottles to maintain sufficient nutrition.
Surgery may correct crossed eyes and enhance limb and jaw deformities. Physical and speech therapy frequently improves motor skills and coordination and leads to better control of speaking and eating abilities. Plastic reconstructive surgery can also be beneficial in some individuals. Nerve and muscle transfers to the intersections of the mouth have been performed to furnish the unreasonable ability to smile.
The remedy of Moebius syndrome is directed toward the distinctive exceptions in each individual. Usually, these children are managed by a multidisciplinary team, frequently in a craniofacial center. Involved specialists consist of pediatricians; neurologists; plastic surgeons; ear, nose, and throat specialists (otolaryngologists); orthopedists; dental specialists; speech pathologists; specialists who assess and treat hearing problems (audiologists), specialists who treat eye abnormalities (ophthalmologists) and another healthcare professionals.
Corrective procedures for facial paralysis involve the transfer of muscle and graft nerves from another area of the face or the body. An old procedure, known as temporalis tendon transfer, involves taking the temporalis muscle, one of the muscles normally utilize for chewing (mastication), and transferring it to the corners of the mouth.
This same type of operation can be also used to enhance the closure of the eyelids. If the paralysis is on exclusively one side (unilateral), a “cross-facial nerve graft” is an option. The procedure involves taking a sensory nerve from the calf, affixing it to a branch of the functioning facial nerve on the normal side of the face, and then waiting till the renewing nerve fibers cross over the face to reach the paralyzed side where it is joined to a motor nerve of a thin muscle transferred to the face by microvascular anastomosis.
The most current procedure, called “the smile operation”, involves the microvascular transfer of a muscle from the thigh (gracious) to the face and touching the nerves that normally supply the masseter muscle (one of the muscles utilized for chewing). This operation has demonstrated remarkable results in terms of speech, facial mobility, and self-esteem. Recurring lubrication for dry eyes is often necessary.
Physiotherapy
The main areas needing physiotherapy intervention are bilateral facial palsy, and also techniques to address bilateral talipes equines in youths with this condition. Early in infancy, children with Moebius Syndrome may have a mild motor delay, so pediatric physiotherapists may be able to provide management advice.
- Motor Delay – general pediatric physiotherapy interventions can be utilized to educate the parents on how to help the child with motor delay. It is recognized that in Moebius Syndrome motor delay, if present at all, is likely to be very mild, so often no specific intervention is suggested.
- Facial Palsy – physiotherapy techniques desired at improving facial movements are indicated for the majority of people with Moebius Syndrome. More components are on the Facial Palsy page. Techniques include neuromuscular reeducation, Trophic Electrical Stimulation, and EMG biofeedback. Many of these youngsters go on to have surgical interventions as the degree of facial palsy is often severe, and the reaction to conservative or physiotherapy interventions is often limited.
- Talipes Equinas, AKA Clubfoot – physiotherapy interventions are indicated for all kids with this condition. In some cases, the reaction to conservative measures may be insufficient, so surgical intervention may be required. Please see the following pages for management of clubfoot: Assessing children with clubfoot, Management of clubfoot, and Multidisciplinary team in managing clubfoot.
Physical therapy may be needed for people with various orthopedic abnormalities. Occupational therapy could also be beneficial, specifically in patients with abnormalities of the hands, fingers, and toes. Speech therapy may be necessary for some involved children. Strabismus is usually surgically curable, although some physicians recommend delaying these procedures as the condition sometimes improves with age. Operations may also be necessary for the different skeletal malformations affecting the limbs and jaws. Specialized procedures to repair abnormalities and/or underdevelopment of the chest wall and breast are available.
Splints, braces, and prostheses may be necessary for individuals with congenital limb abnormalities (clubbed feet, missing fingers). Genetic counseling may also be of benefit to concerned individuals and their families. Surgery may be required to help correct strabismus (crossed eyes) or to transfer nerves and muscles to the face, improving the ability to smile. Reconstructive surgery can also help address facial, limb, and jaw differences.
Prognosis of Moebius syndrome
There is no cure for Moebius syndrome. Despite the impairments that represent the disorder, proper care and treatment give many individuals a normal life longing.
Summary
Moebius syndrome is a rare neurological disorder distinguished by weakness or paralysis (palsy) of multiple cranial nerves, most frequently the 6th (abducens) and 7th (facial) nerves. Other cranial nerves are sometimes affected. The disorder is present at birth (congenital). If the 7th nerve is affected, the individual with Moebius syndrome is unable to smile, frown, pucker the lips, raise the eyebrows, or close the eyelids. If the 6th nerve is concerned, the eye cannot turn outward past the midline. Other abnormalities consist of underdevelopment of the pectoral muscles and defects of the limbs. Moebius syndrome is not progressive. The exact cause is unknown. It appears to happen randomly (sporadically) in most cases; yet, some cases occur in families suggesting that there may be a genetic component.
FAQ
How Frequent Moebius syndrome occurs?
The precise incidence of Moebius syndrome is unknown. Researchers calculate that the condition affects 1 in 50,000 to 1 in 500,000 newborns. Moebius syndrome can also be associated with a somewhat improved risk of intellectual disability; yet, most affected individuals have normal intelligence. The precise incidence of Moebius syndrome is unknown.
What is Inheritance of the moebius syndrome?
Most cases of Moebius syndrome are irregular, which means they appear in people with no history of the disorder in their family. A small percentage of all cases have been reported to run in families; nevertheless, the condition does not have a single obvious inheritance pattern.
Who might get Moebius syndrome?
Scientists have not recognized any specific factors that increase a person’s chances of having Moebius syndrome. It appears in both girls and boys of all ethnicities.
How common is Moebius syndrome?
Moebius syndrome is very rare. The precise incidence is unknown, but some estimates are 2 to 20 cases per million births.
Can people with Moebius syndrome speak?
These abnormalities contribute to tribulations with speech, which occur in many children with Moebius syndrome. Dental abnormalities, including missing and misaligned teeth, are also expected. Moebius syndrome also involves muscles that control back-and-forth eye movement.
Is Moebius syndrome a disability?
Although Moebius syndrome is sometimes associated with intellectual disabilities such as autism, and developmental delays, it mainly affects children of normal intelligence and cognitive development. The disorder is named after the German physician Paul Julius Moebius who described the condition in 1888.
Can Moebius syndrome be cured?
Nerve and muscle transfers to the intersections of the mouth have been performed to furnish the limited ability to smile. There is no cure for Moebius syndrome. Despite the impairments that describe the disorder, proper care and treatment give many people a normal life expectancy.
Can Moebius syndrome be detected before birth?
Particular ultrasonography should be performed to detect any malformations possibly related to misoprostol exposure (e.g. limb defects), although it is almost incomprehensible to detect cranial nerve palsies of Moebius syndrome before birth.
Does Moebius syndrome affect the brain?
Moebius syndrome can impact cranial nerves responsible for the control of muscles in the tongue, jaw, larynx, and throat, as well as ones that produce speech.
Is Moebius syndrome bilateral?
Moebius syndrome (MBS) is a rare disease distinguished by unilateral or bilateral nonprogressive congenital facial palsy (VII cranial nerve) with impairments of ocular abduction (VI cranial nerve); it may also be associated with other cranial nerves (CN) palsies, orofacial anomalies, and limb defects.


2 Comments