Folate Deficiency (Vitamin B9 Deficiency)
What is Folate Deficiency?
Folate Deficiency (Vitamin B9 Deficiency) can result from inadequate dietary intake, poor absorption, or increased demand due to factors such as pregnancy or certain medical conditions.
Folate, also known as vitamin B9, is a vital nutrient essential for various physiological functions within the body. Its primary roles include facilitating DNA synthesis, cell division, and the formation of red blood cells.
Low blood levels of folate and its derivatives are indicative of folate insufficiency, sometimes referred to as vitamin B9 deficiency.
This can lead to a kind of anemia known as folate deficiency anemia, which is a late discovery in folate insufficiency and is characterized by unusually large red blood cells. Folate deficiency frequently manifests subtly.
The following symptoms might be present: fatigue, palpitations, heart palpitations, shortness of breath, dizziness, open sores on the tongue, appetite loss, skin or hair color changes, irritability, and behavioral abnormalities.
There might be a brief, reversible infertility. Premature babies born low-weight and with neural tube abnormalities can result from folate deficiency anemia during pregnancy.
Within a few months, a folate shortage might result from inadequate folate consumption. Other possible explanations include people with shorter red blood cell lifespans and those with greater requirements, similar to those during pregnancy.
Vitamin B12 insufficiency or a homocysteine methyl transferase malfunction that results in an inactive metabolite that cannot be recovered—a “folate trap”—can be secondary causes of folate deficiency.
Serum folate levels and complete blood counts are two common blood tests used to confirm the diagnosis.
Elevated homocysteine levels can indicate a deficient status, but there are other variables at play. It is important to rule out vitamin B12 deficiency since, if addressed, it might result in irreparable brain damage.
Supplemental folic acid and dietary modifications may be part of the treatment. Making dietary adjustments, such as consuming more fruits and leafy green vegetables, which are high in folate, might be beneficial.
For people who are contemplating a pregnancy or who are already pregnant, prevention is advised. In nations where folic acid fortification initiatives are in place, folate deficiency is quite rare. Globally, folic acid deficiency-related anemia is typically relatively rare.
Folate deficiency A low level of folic acid in the blood is called anemia. The B vitamin folic acid aids in the production of red blood cells in your body. Anemia is a condition in which the red blood cell count is low.
Signs and Symptoms Folate Deficiency
The majority of the time, folate deficiency anemia symptoms are mild. In adults, anemia (specifically, macrocytic, megaloblastic anemia) may indicate a severe folate shortage.
Fatigue, weakness, skin or hair color changes, open sores on the mouth, palpitations, lightheadedness, cold hands and feet, headaches, easy bleeding or bruising, low-grade fevers, and loss of appetite.
Weight loss, diarrhea, diminished taste, irritability, and behavioral disorders are some of the symptoms of folate deficiency anemia.
Pregnant women who are deficient in folate are more likely to give birth to preterm babies who have low birth weight, as well as babies who have neural tube problems or even spina bifida.
A lack of folate in babies and kids can cause megaloblastic anemia, diarrhea, mouth ulcers, delayed development, and cerebral impairment. Additional symptoms include an unusually tiny head, irritability, developmental delay, seizures, blindness, and cerebellar ataxia.
Causes of Folate Deficiency
A folate shortage can result from increased folate requirements in the body, insufficient folate intake or absorption through food, or increased folate excretion (or loss) in the body.
The body may require more folate if you take any medications that prevent the body from using it. According to some studies, using tanning beds and other UV radiation exposure might cause a folate shortage.
Adolescents, babies, children, and pregnant women are more likely to have the deficit. It could also be the result of an unhealthy diet or an alcoholism aftereffect.
Furthermore, a “methyl-trap” of tetrahydrofolate (THF) can result from a homocysteine methyltransferase defect or a vitamin B12 deficiency.
In this scenario, THF is converted to a reservoir of methyl-THF, which cannot be metabolized and acts as a sink of THF that subsequently results in a folate deficiency.
Therefore, a huge pool of methyl-THF that is incapable of undergoing reactions can be produced by a B12 shortage, which will simulate folate insufficiency. Pteroylmonoglutamate, or folate, is mostly absorbed in the jejunum but is distributed throughout the small intestine.
Proton-coupled folate transporter (SLC46A1) transports the reduced polyglutamate chain across the brush border membrane after pteroylpoly glutamate hydrolase (gamma-glutamyl hydrolase) reduces it.
These are significant steps in the absorption process. Reduced absorption may occur from diffuse inflammatory or degenerative small intestinal illnesses such as Crohn’s disease, celiac disease, chronic enteritis, or the existence of an entero-enteric fistula.
Situational Folate Deficiency
The following are some circumstances that make folate more necessary:
- bleeding
- kidney dialysis
- liver disease
- malabsorption, including celiac disease and fructose malabsorption
- pregnancy and lactation (breastfeeding)
- tobacco smoking
- alcohol consumption
Medication
The following medications may interfere with the metabolism of folate:
- Anticonvulsant drugs (such primidone, valproate, carbamazepine, or phenytoin)
- Metformin (sometimes recommended for type 2 diabetes blood sugar management)
- Methotrexate is an anti-cancer medication that is also used to manage inflammation brought on by rheumatoid arthritis, ulcerative colitis, and
- Crohn’s disease.
- 5-fluorouracil
- hydroxyurea
- trimethoprim
- Sulfasalazine (used to manage inflammation linked to rheumatoid arthritis, ulcerative colitis, and Crohn’s disease)
- triamterene (a diuretic)
- Birth control tablets may lower blood folate levels without causing a clinically significant folate shortage (this is also related to the length of time that birth control pills are used).
Supplements containing folic acid are occasionally administered together with methotrexate prescriptions.
Methotrexate inhibits dihydrofolate reductase, which lowers the rate of cell division, and de novo purine and pyrimidine production, which is how it has its therapeutic benefits. Methotrexate is a medication that stops cell division.
It is especially harmful to quickly dividing cells, such as cancer cells and immune system progenitor cells. Patients using long-term, low-dose methotrexate for inflammatory diseases such as rheumatoid arthritis benefit from folate supplementation.
(RA) or psoriasis, in order to prevent folate-induced macrocytic anemia. In an effort to preserve healthy tissue, folate supplements are frequently given before some high-dose chemotherapy treatments. Taking a folic acid supplement together with methotrexate during cancer therapy, however, can be detrimental.
Cerebral Folate Deficiency
When 5-methyltetrahydrofolate levels in the cerebral spinal fluid are low in the brain despite being normal in the blood, this condition is known as cerebral folate insufficiency. Usually, the onset of symptoms occurs at five months of age.
Seizures, decreased muscle tone, coordination issues, difficulty speaking, and problems speaking might occur without therapy. Gene mutations affecting folate metabolism and transport are among the causes of cerebral folate insufficiency.
The proton-coupled folate transporter (PCFT), which is encoded by the SLC46A1 gene, is mutated in CFD syndromes, causing both systemic and cerebral folate deficiencies. Folate can repair systemic insufficiency, but folinic acid is still needed to treat cerebral deficiency.
Pregnancy
The growing fetus’s increased cell count, decreased folate intake and absorption, the mother’s hormones that regulate folate metabolism, the fetal and mother’s blood’s vascular circulation, and the dilution caused by.
An increasing volume of blood can contribute to folate deficiency during pregnancy. Pregnant women with sickle cell anemia and those who reside in malarial regions have considerably greater folate requirements.
Supplementing with 450 micrograms of folic acid daily lowers the chance of neural tube defects, which are a kind of birth problem.
addition The best time to treat birth abnormalities is a month before and during the first twelve weeks of pregnancy. Preconception folic acid treatment has been demonstrated to reduce neural tube abnormalities by 70%.
Diagnosis
A blood test measuring the serum amount of methyltetrahydrofolate—a form of folate that is almost unique in the blood—is used to detect folate insufficiency.
In practice, “folate” refers to all derivatives of folic acid. Methylmalonic acid is normal (increased in vitamin B12 insufficiency), however homocysteine is raised (5-MTHF is utilized to convert homocysteine to methionine).
More precisely, in accordance with a UK guideline from 2014:
- When the blood folate level is below 7 nmol/L (3 μg/L), it is considered folate deficient.
- Red blood cell folate testing is not usually done since serum folate is usually sufficient; however, it can be done if there is a strong suspicion of folate shortage even in situations where serum folate levels are normal.
- Measurements of plasma total homocysteine are limited to specific situations. While local reference values should be considered, a reading exceeding 15 μmol/L may indicate a folate deficit.
Prevention and Treatment of Folate Deficiency
Diet
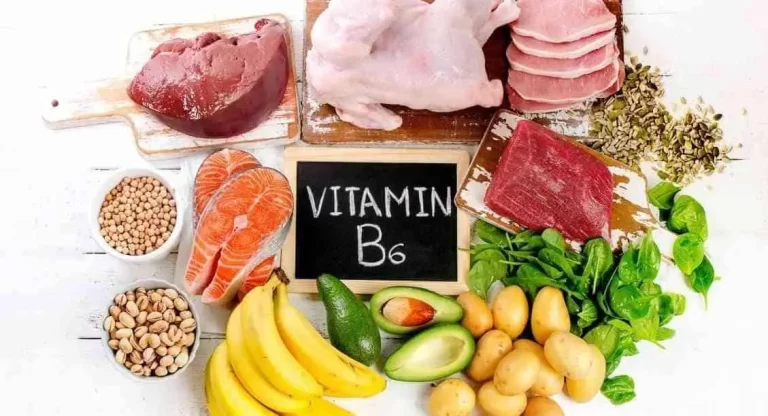
Legumes, organ meats, and leafy green vegetables are good sources of folate for the diet. Using a microwave oven, a food steamer, or steaming during cooking can help preserve more folate in the finished product.
Supplementation
A synthetic form of folate, folic acid is obtained through dietary supplements. Folic acid and other B vitamins can be found in multivitamin dietary supplements. In certain nations, folic acid is accessible without a prescription as a dietary supplement.
In other nations, folic acid fortification of wheat flour, corn meal, or rice is mandated in an effort to improve public health by raising blood folate levels in the populace.
Fortification
Following the identification of the connection between low folic acid and neural tube abnormalities, folic acid supplementation was advised for expectant mothers by governments and health organizations around the globe.
Since the neural tube shuts during the first four weeks of pregnancy, sometimes before most women even realize they are pregnant, several nations have chosen to impose laws requiring nutritional fortification.
According to a meta-analysis of the global birth prevalence of spina bifida, there was a 30% decrease in live births with the condition when mandatory fortification was compared to nations where medical professionals advised women but where there was no mandatory fortification program.
Some nations even reported a greater than 50% decrease. Some foods must be fortified with folic acid in more than 80 countries.
Rice fortification is widespread. Since 1998, the USDA has mandated that flour be fortified. Since then, the largest decrease in neural tube abnormalities has been observed among Hispanics in the United States.
Since 1998, Canada has required the fortification of flour with folic acid, which has led to a 42% reduction in neural tube abnormalities. In Costa Rica, fortification of milk, rice, wheat, and maize flour is mandated, and this has resulted in a 60% decrease in neural tube abnormalities.
Epidemiology
In nations where folic acid fortification initiatives are in place, folate deficiency is quite rare. Overall, folic acid deficiency-related anemia is quite rare worldwide. However, there is a dearth of information about the incidence of deficiencies in particular high-risk categories.
Research
Different developmental problems may arise from folate insufficiency during pregnancy or infancy caused by the fetus or newborn developing autoantibodies against the folate receptor.
Research indicates that major depressive illness may be caused by inadequate folate and vitamin B12 status and that these conditions may benefit from supplementation.
Because transmethylation events are essential for the synthesis of neurotransmitters (e.g., serotonin, epinephrine, nicotinamides, purines, and phospholipids), vitamin B12 and folate have a role in depression.
According to the suggested mechanism, insufficient folate or vitamin B12 levels might interfere with the transmethylation process, which can result in a buildup of homocysteine (hyperhomocysteinemia) and poor metabolism of neurotransmitters.
Phospholipids, myelin, and receptors— particularly the hydroxylation of dopamine and serotonin from tyrosine and tryptophan.
By oxidative processes, elevated blood homocysteine levels can cause vascular damage and perhaps worsen brain impairment. Any of these may contribute to the emergence of different kinds of diseases, depression included.
FAQ
What happens if your folate is low?
Insufficiency in vitamin B12 or B9, also referred to as folate The body produces too many large red blood cells or anemia, when there is insufficient folate or vitamin B12. These cells cannot function correctly. Oxygen is transported throughout the body by red blood cells through a material known as hemoglobin.
Is B12 and folate the same?
Vitamin B12 plays a crucial role in the synthesis of DNA and RNA, the body’s genetic material, and is particularly necessary for the maintenance of healthy nerve cells. Together, vitamin B12 and vitamin B9, sometimes referred to as folate or folic acid, aid in the production of red blood cells and enhance the body’s ability to use iron.
What is the most common cause of folate deficiency?
Individuals who habitually abuse alcohol, have a restrictive diet that excludes ingesting enough amounts of folate, and have an overall imbalanced and unhealthy diet are more likely to suffer from folate insufficiency, which is caused by a lack of dietary folate.
Can folate deficiency be cured?
The cause of vitamin B12 or folate deficient anemia determines the course of therapy. For the majority of patients, vitamin replacement therapy with injections or pills is a simple treatment option.
What foods have folate?
Many different foods, particularly vegetables (especially dark green leafy vegetables), fruits, nuts, beans, peas, shellfish, eggs, dairy products, meat, poultry, and grains naturally contain folate.
What is a normal folate level?
The typical range is 2.7 to 17.0 nanograms per milliliter (ng/mL) or 6.12 to 38.52 nanomoles per liter (nmol/L). The typical ranges of values could vary slightly across laboratories. Discuss the significance of your test findings with your clinician.
Can you have normal B12 but low folate?
While vitamin B12 insufficiency may be verified by raised homocysteine and MMA levels and low B12 levels, folate deficiency can be verified by normal B12, MMA, and homocysteine levels and elevated homocysteine levels. RBC folate levels may be used to determine the duration of a deficit and are a highly helpful indicator of body storage.