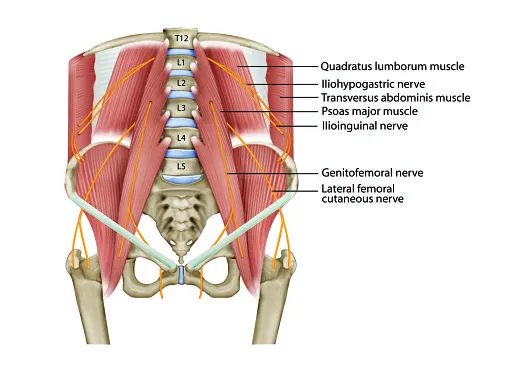
Genitofemoral Neuralgia
What is Genitofemoral neuralgia?
Genitofemoral neuralgia (nerve pain) is a compression neuropathy that involves both males and females. It induces pain in the lower abdomen, groin region, and inner thigh due to a compressed or pinched nerve. Genitofemoral neuralgia is one of the most familiar causes of lower abdominal and pelvic aches.
Persons suffering from genitofemoral neuralgia will usually be forced into a bent-over position to help some of the pain. If genitofemoral neuralgia stays untreated, the abnormal position can lead to bulging of the anterior abdominal wall muscles. advanced motor deficit consisting of bulging of the anterior abdominal wall muscles may happen.
What are the Causes of Genitofemoral neuralgia?
The major cause of this disease is nerve damage. This infrequently happens by itself and may be secondary to
Inguinal hernia surgery- Continuing pain after inguinal hernia surgery is not unusual and genitofemoral nerve issue is one of the known causes. It can occur after both laparoscopic surgery and open hernia surgery and numerous mechanisms may be liable like an injury during surgical hernia repair, laparoscopic port insertion, mesh placement and tying of the cremasteric artery, securing, entrapment of the nerve in the scar tissue and the adhesions near the mesh.
There is the info on genitofemoral nerve damage after many other surgeries like:
Pelvic lymph nodes dissection as in uterine, ovarian, bladder, or prostate cancer surgery or when a big pelvic mass is extracted
Kidney removal (Nephrectomy)
Appendix removal (appendectomy)
Uterus removal (Hysterectomy)
Cesarean section
Other surgeries include retraction of the psoas muscle like spinal surgery- lateral interbody fusion by retroperitoneal trans psoas methods.
Other non-surgical causes include:
Abdominal/pelvic trauma or pelvic fractures or retroperitoneal hematoma (blood accumulation in the posterior part of the abdomen)
Psoas muscle-related problems like compression due to abscess or Potts disorder (TB of the spine)
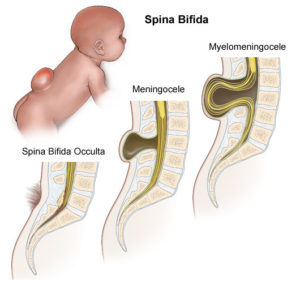
Spinal issues like cancer spread to bones, compression fractures, narrowing of the spine (spinal stenosis) at upper lumbar levels
Peripheral neuropathy- nerve injury due to diseases like alcohol abuse, diabetes, cancer treatments, vitamin deficiencies, etc
Symptoms of Genitofemoral neuralgia
Symptoms associated with this disease contain:
A familiar presenting complaint is a groin, lower abdominal, or genital ache which can be a heavy sensation or severe, dull, burning, electric shock-like, throbbing, sharp pain. In men, it affects the scrotum whereas in women the labia majora and mons pubis are affected.
Ache may be accompanied by changed sensations like tingling, numbness in the involved location
Pain may be irregular or frequently present. Normally, it involves one side, infrequently both sides can be affected
Frequently there is tenderness near the side of the pubis (pubic tubercle) on the involved side
Physical exercise like running, walking, jumping, and sexual intercourse can cause aggravating aches. Elongation of the lower back while flexing backward can also raise pain. Frequently persons with this disease walk in a bent-over position
How Is Genitofemoral Neuralgia Diagnosed?
The first actions in determining the presence of genitofemoral neuralgia are a conversation with your doctor or physician about your symptoms and medical record and a physical examination. These further tests may be required:
Blood tests
Bone scan
CT scan
MRI
Ultrasound
The tests are easily handled and assist your doctor or physician decide which treatments are suitable for your complaint.
Treatment of Genitofemoral neuralgia
A multimodal method with a combination of several modalities is used to provide ease. such as:
Lifestyle modifications
Drugs acting on the nerves (neuropathic agents), anti-inflammatory drugs
Nerve blocks
Pulsed radiofrequency therapy
Cryoablation
Spinal injections
Surgical interventions
Injections play a key part in the diagnosis the management of this disease. These are non-surgical choices that can provide prolonged ease. The choices are discussed in additional detail down
Ultrasound Guided Nerve blocks
Genitofemoral nerve identification under ultrasound needs a reasonable quantity of skill. The nerve block injections include injecting a variety of numbing agents (local anesthetics) and a little number of steroids. The local anesthetic feeds quick ease but is short lasting, whereas the steroid brings time to begin working but can provide longer lasting ease. These injections can assist to decrease the inflammation, may allow freeing the nerve of the stress from encircling structures, and also decrease the sensitivity of the nerves thereby decreasing the ache signals being sent via these nerves. The use of ultrasound improves the accuracy of injections and decreases the potential for side impacts.
Ultrasound Guided Pulsed Radiofrequency Treatment
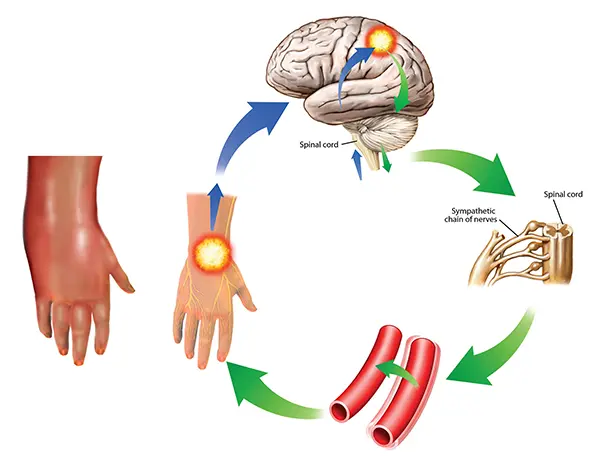
This is a secure, useful treatment modality that can assist in decreasing pain. The treatment includes modulating the route pain signals are sent and processed, with the possibility of delivering lasting ache ease.
This therapy is completed as a day case under local anesthesia, using special syringes and a radiofrequency generator. A syringe is put close to the nerve under ultrasound advice observed by testing to guide proper syringe placement. Radiofrequency therapy is then performed on a tiny region of the nerve by using the radiofrequency device. This decreases the ache signals being sent by the nerves to the brain resulting in ache ease.
Ultrasound Guided Cryoablation
Cryoablation offers advantages over radiofrequency like fast pain ease, no risk of neuroma construction, and higher probabilities of successful pain ease as the probe marks a larger site. The pain ease from the method may last from months to a year. As the method exits the outer layer of the nerve intact the nerve does rise back but the original ache for which the process was conducted may not return or be less painful if it returns.
Spinal injections
The genitofemoral nerve arises from the upper part of the lumbar spine as described previously. Any issues in the spine from where the nerve originates, like stress on the nerve roots, exemplify equal symptoms and may not answer to injections done distally along the course of the nerve. This location is also targeted if the nerve in the front is not available due to scarring etc. Occasionally a mixed method is conducted where the nerve is targeted both in the front and where it arrives out of the spine, to raise the chances of ache ease.
These injections are conducted under x-ray recommendation as a day case process. The options contain epidurals, nerve root blocks, and pulsed radiofrequency therapy.
Surgery
This is supposed for intractable aches not reacting to other therapies. Surgery aims to either free the nerve of all external force/entrapment or to excise a portion of the nerve (neurectomy). If patients with scarring due to previous surgery, visualization, and release of the nerve can be difficult. The cut nerve ends are connected and sowed into the muscle fibers to control neuroma (swelling of the nerve) construction. A neuroma formed can lead to more harmful aches later. Cutting the nerve created numbness or decreased sensation in the regions provided by the nerve which contains the aspects of the genitalia noted previously and the upper thigh.
Physiotherapy treatment
Ice packs
Acupuncture
Genitofemoral nerve block
Cryo-nerve ablation
Trigger point injections
Relaxation techniques
Low-intensity laser therapy
TENS- transcutaneous electric nerve stimulation
Femoral nerve neural mobilization in unilateral active PKB (prone knee bending)
Lie on your front in a prone position on a raised surface with one leg on the bed and the further leg straight in contact with the bottom. Flex your knee joint of the horizontal leg (heel to buttock) and hold the position when you sense a stretching sensation. Recount.
Prone femoral nerve glide
Lie on your stomach in a prone position with flex elbow joints (so you are relaxing on your forearms). Begin by flexing the knee joint of the occupied side as much as possible, maintaining the thigh on the table. Subsequently, decline the leg back on the table at the exact time as you raise the trunk by forcing with your forearms. Alternate between these activities, flexing the knee joint and extending the trunk.
FAQ
How do you stop genitofemoral nerve pain?
Initial therapy of genitofemoral neuralgia will generally consist of anti-neuropathic, nonsteroidal anti-inflammatory, and vulnerable opioid drugs. Qutenza patches can also be regarded as a conservative process of localized therapy.
How does the genitofemoral nerve get injured?
This can occur with penetrating trauma, a knife wound, or surgical exploration of the groin. In some patients, during surgery on the saphenous vein for varicose vein ligation, retractors can cause abrasive damage. It can also be injured in the inguinal canal, mostly during inguinal hernia repair.
How do you stretch the genitofemoral nerve?
Kneeling on one knee joint, with your foot relaxing on a chair behind you. Fold your base under and lunge barely forward into hip extension. Once you sense a mild stretch gradually bend your head and upper back down to boost the stretch for a few seconds then recount.
Is genitofemoral nerve sensory or motor?
The genitofemoral nerve is mainly a sensory nerve that supplies the upper thigh part in both genders. It especially provides the mons pubis and labia majora in women, and the skin of the anterior scrotum in men.
How do you release a nerve in your groin?
Stand erect and placed the leg on the side that senses pinched behind your further leg. Move your hip outward and lean to the opposing side. Extend the arm on the side of the involved region of the groin above your head and lengthen it toward that side of your body. Maintain this position for up to 20 seconds.