Osteomyelitis
What is Osteomyelitis?
A bone infection, also known as osteomyelitis, can result when bacteria or fungi plague a bone from the bloodstream or surrounding tissue. Trauma to the skin, maybe from surgery, may be affected. In kids, bone infections most generally appear in the long bones of the arms and legs. In grown-ups, they generally occur in the hips, spine, and feet.
Bone infections can occur unexpectedly or expand over a long time. If they’re not correctly treated, bone infections can exit a bone permanently harmed.
What are the types of osteomyelitis?
Types of osteomyelitis contain:
Acute: This infection arrives unexpectedly. You may keep a fever and then invent pain in the infected region days after.
Chronic: Chronic osteomyelitis is a bone disease that doesn’t go out with treatments. It causes bone discomfort and systematic drainage (pus). Infrequently, chronic osteomyelitis doesn’t keep symptoms. The infection may go hidden for months or even years.
Vertebral: This kind involves the spine. It causes chronic backache that gets more harmful when you move. Management like heating, resting, and pain relievers don’t support. It infrequently causes a fever. A patient who lives in nursing houses, abuse intravenous medications, or is on dialysis are more inclined to spinal bone infections.
What are the symptoms of osteomyelitis?
People presenting with osteomyelitis may have the following symptoms:
- Pain and/or tenderness in the infected region (pain may not ever be an aspect early in the infectious cycle due to the shortage of pain fibers in cancellous bone).
- Inflammation, redness, and warmth in the involved region
- Fever, chills, and extreme sweating
- Nausea and a generalized feeling of existing sick
- Lower back ache (if the vertebrae are affected and the range of movement of the lumbar spine may be reduced and painful)
- Swelling of the ankles, legs, and feet
- Joint or junction pain – if the infection spreads into the periosteum of the bone, people may feel joint or junction pain, reduced function, and systemic signs, like swelling, fever, and malaise
- Antalgic gait – if the infected lower extremity bone causes ache
- Sausage toes – a clinical indication that has been demonstrated to have adequate sensitivity and particularity, may be present if osteomyelitis involves the phalanges of the feet in diabetic people.
- The primary indications of osteomyelitis may differ between grown-ups and kids.
In kids, osteomyelitis supervises to be acute, and it generally occurs within 2 weeks of a pre-existing blood infection. This is called hematogenous osteomyelitis, and it is generally due to methicillin-resistant Staphylococcus aureus (S. aureus) (MRSA).
They have hurtful complaints, like high fever and extreme pain, but in a few subjects, the predominating symptoms are erythema, edema, and tenderness in the involved region.
In grown-ups, sub-acute or chronic osteomyelitis is more familiar, particularly after surgery or trauma, an injury, like a fractured bone. This is called contiguous osteomyelitis. It generally involves grown-ups over the age of 50 years
Which are the Causes of Osteomyelitis?
Bone infection is most frequently caused by bacteria. But it can also be generated by fungi or different germs. When a patient has osteomyelitis:
Bacteria or different germs may extend to a bone from muscles, infected skin, or tendons next to the bone. This may happen under a skin sore.
The disease can begin in another body aspect and extend to the bone via the blood.
The disease can also begin after bone surgery. This is more possible if the surgery is done after damage or if metal bars or plates are put in the bone.
In kids, the long bones of the arms or legs are most frequently affected. In grown-ups, spine bones (vertebrae), the feet, and hips (pelvis) are most generally involved.
Risk factors
- Diabetes
- Hemodialysis
- Poor blood supply
- Recent injury
- Use of injected illicit medicines
- Surgery including bones
- Weakened immune system
Epidemiology
- Osteomyelitis can happen at any age, it is familiar between the ages of 2-12 and is more familiar in men
- Circulation diseases, like peripheral arterial disorder
- Situations needing intravenous tubes or catheters
- Sickle cell condition
- Systemic Lupus Erythematosus (SLE) can also be associated with producing osteomyelitis.
- Malnutrition
- Chronic hypoxia
- Extremes of age
How is osteomyelitis diagnosed?
Physical examination
To verify a diagnosis of presumed osteomyelitis, your doctor or physician will first bring out a physical inspection of your involved body region to check for swelling, redness, and tenderness.
They will want to understand your recent medical records, like whether you have just had surgery, an injury, or a prior infection.
If your doctor or physician is uncertain regarding a diagnosis or doubts about osteomyelitis, they may guide you to an orthopedic surgeon (an expert in bones and joints or junctions).
Laboratory Test
After evaluating your symptoms and conducting a physical examination, your healthcare provider or doctor may contain one or more of these tests:
- Blood tests: A complete blood count (CBC) examination for signs of inflammation and infection. A blood culture examines for bacteria in your bloodstream. C-reactive protein: More elevated concentrations can show inflammation. White blood cell count: More elevated levels may suggest an infection.
- Erythrocyte sedimentation rate: This guides to the space that red blood cells transit in 1 hour before settling, and the speed may be promoted in a person with osteomyelitis.
- Imaging tests: X-rays, CT scans, MRIs, and ultrasounds supply images of your muscles, bones, and tissues.
- Bone scan: A bone scan utilizes a small quantity of safe, radioactive material to resolve infections or fractures during an imaging scan.
- Biopsy: Your healthcare provider or doctor conducts a syringe biopsy to take samples of fluid, tissue, or bone to study for signs of infection.
Treatment of Osteomyelitis
Medical treatment
An antibiotic is generally begun as shortly as possible. The initial antibiotic selected is one that is possible to destroy the germs (bacteria) which generally cause osteomyelitis. Nevertheless, the antibiotic is sometimes switched to a further one when the outcomes of the tests verify which bacterium is causing the infection. (Some bacteria are invulnerable to a few antibiotics.)
Osteomyelitis symptoms may drop quite fast after you begin taking an antibiotic. You may have to bring the drug for 4-6 weeks but, if you have an extreme infection, the dose may stay up to twelve weeks. This is to make it foolproof all illness has moved from the bone.
To manage the pain you may be offered painkillers and if you have a sickness in a long bone (like an arm or leg) you may be provided with a splint to limit motion.
Quick treatment is suggested for osteomyelitis, particularly in the acute phase. Treatment is generally started with an antibiotic, specified by the outcomes of the bone biopsy or cultures carried, provided intravenously at a high amount. Factors like the people’s age, fitness status, place of infection, and initial antimicrobial treatment are brought into consideration when choosing the antibiotic used for treatment. The antibiotics are generally specified for 4-6 weeks observed by >8 weeks of oral therapy.
Osteomyelitis may also require minister surgically. Possibilities involve:
Draining the involved region
Subtraction of necrotic bone and soft tissue
Fixing normal blood flow to the bone
Withdrawing any foreign objects
Amputation of the involved limb.
Substitute of infected prostheses, like total hip arthroplasty parts
Physiotherapy treatment in Osteomyelitis
Knee-to-chest stretch
Lie on your back in a supine position with your knees flexed and your feet flat on the bottom. Utilizing both hands, drag up one knee joint and push it to your chest. Tense your abdominals muscles and push your spine to the base. Maintain for 5 seconds. Return to the beginning position and replicate with the opposing leg. Return to the beginning position and then replicate with both legs at the exact time. Reprise per stretch 2 to 3 times preferably earlier in the morning and earlier at night.

Lower back rotational stretch
Lie on your back in a supine position with your knees flexed and your feet flat on the bottom. Maintaining your shoulders firmly on the bottom, move your flexed knees to one side. Maintain for 5 to 10 seconds. Return to the beginning position. Repeat on the contrasting side. Replay per stretch 2 to 3 times preferably one time in the morning and one time at night.

Lower back flexibility exercise
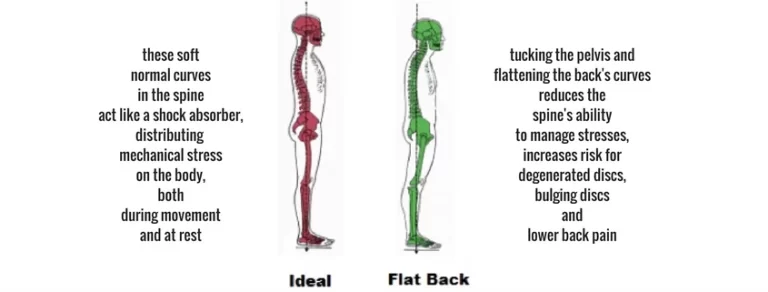
Lie on your back in a supine position with your knees flexed and your feet flat on the bottom. Tense your abdominal muscles so your stomach stretches out from your waistband. Maintain for five seconds and then rest. Flatten your back, dragging your belly button toward the bottom. Maintain for five seconds and then rest. Reprise. Begin with five repetitions per day and slowly perform up to 30.
Bridge exercise
Lie on your back in a supine position with your knees flexed and your feet flat on the bottom. Maintaining your shoulders and head rested on the ground, tenses your abdominal muscles and gluteal muscles. After then lift your hips to form a straight line from your knee joints to your shoulders. Attempt to maintain the position long sufficiently to finish three deep breaths. Return to the beginning position and replay. Begin with five repetitions per day and slowly perform up to 30.

Cat stretch
Take a position like a dog or yourself on your hands and knees. Gradually bend your back, as if you’re dragging your abdomen up toward the roof. Then gradually allow your back and abdomen to hang toward the ground. Return to the beginning position. Reprise 3 to 5 times double a day.

Seated lower back rotational stretch
Sit in a sitting position on an armless chair or a stool. Cross your right leg over your opposite leg. Bracing your left elbow opposite the exterior of your right knee joint, wrench and stretch to the side. Maintain for 10 seconds. Reprise on the further side. Reprise this stretch 3 to 5 times per side double a day.

Shoulder blade squeeze
Sit in a sitting position on an armless chair or a stool (A). While keeping a good posture, drag your shoulder blades jointly. Maintain for five seconds and then rest. Replicate 3 to 5 times double a day.
Frankenstein walk
This activity operates your quads, hips, and hamstrings. It also improves the range of movement. Keep good posture, avoid twisting at the waist, and improve your gait as you progress.
Stand in a standing position with your arms outstretched in front of you, palms meeting down.
As you move ahead, hang your right leg up to stretch it straight out, making a 90-degree curve with your body.
Drop your right leg to the ground, then sway your left leg up in an exact manner.
Persist for 1 minute, switching direction if your area is fixed.
Once you sense comfort, do the movement by getting your arm out to touch your opposing foot, and expanding your other arm after you.
Hip circles
This exercise improves flexibility and strength. For more help, use a steady thing for help.
Stand in a standing position on your right leg with your left leg raised.
Thrust your left leg in rings.
Accomplish 20 rings per direction.
Then accomplish the opposite leg.
To complete this activity, rise the size of the rings and do 23 sets.
Sidestep exercise
Maintain your hips and toes encountering straight forward. Raise the power by lowering the band so it’s exceeding your ankles and reducing your squat position.
Stand in a half-squat position with an opposition band near your lower thighs.
Entertain your hip muscles as you gradually bring small steps to the side.
keep 15 steps in one order.
Accomplish the further side.

This activity makes strength in your thighs, hips, and glutes. It keeps your pelvic muscles and can reduce tightness in your lower back, which allows control over overuse and injury. Once you’ve learned the primary pose, fit out a few interpretations.
Lie on your side in a side-lying position with flexed knees and a resistance band near your inferior thighs.
Turn your top leg up as elevated as you can, then wait for a point.
More down to the beginning position.
Accomplish 13 sets of 815 repetitions.

Hip marching
This movement creates power and flexibility in your hips and thighs.
Sit in a sitting position toward the front border of a chair.
Lift your left leg as elevated as you can, maintaining your knee flexed.
Gradually and with management, lower your foot.
Then accomplish the opposite side.
This is 1 recurrence.
Accomplish 23 sets of 512 repetitions.
Butterfly pose
This movement stretches your hips while enhancing blood circulation.
Relax your sitting bones on the border of a pillow or folded blanket to keep the pelvic tilt. If you sense tight, put blocks or pillows under your thighs for help.
Sit in a sitting position with your knees flexed and the soles of your feet jointly.
Twist your fingers beneath your feet. Utilize your elbows to gently push your knees down to the ground.
Experience an opening in your hips as you remove stress.
After 30 seconds, expand your arms in front of you and reach into an ahead fold.
Keep this position for at least 1 minute.
You can worsen the stretch by getting your heels in near your body.

Donkey kicks
Do this movement to tone and maintain your hips and glutes.
From the tabletop position, raise your right knee joint, maintaining it flexed as you kick upward.
Obtain the base of your foot toward the roof.
Return to the beginning position.
Accomplish 23 sets of 1220 repeats per side.

Knee Extension
Sit in a sitting position on a table or desk with your legs slumping willingly, and put a thin pillow under your knee joint, so that the knee is just higher than the hip. Unfold the knee joint gradually with the foot curved, until the leg is expanded; maintain for 3-5 seconds, and then decline gradually under supervision. Accomplish 10 repetitions and reprise with the further leg. You can do 2-3 sets as required.
As you get more powerful, you can add light ankle poundages to raise the resistance. Your hamstring muscles will also bring an amazing stretch in the procedure, as you maintain your quads.
Knee Flexion (Standing)
Stand in a standing position on a 2-inch panel or small step. Maintaining your thigh in a straight line with the upper body, flex your knee to a 90-degree arc and gradually lower down. Maintain your foot bent throughout the motion. You can maintain your thigh pushed opposite a table, to confirm that it stays in line with your trunk.
Accomplish 10 repetitions, and replicate with the other leg. You can accomplish 2-3 sets as required.
As you get more powerful, you can add light ankle poundages to raise the resistance. In this activity, your hamstring muscles get more powerful, while you push out your quads.
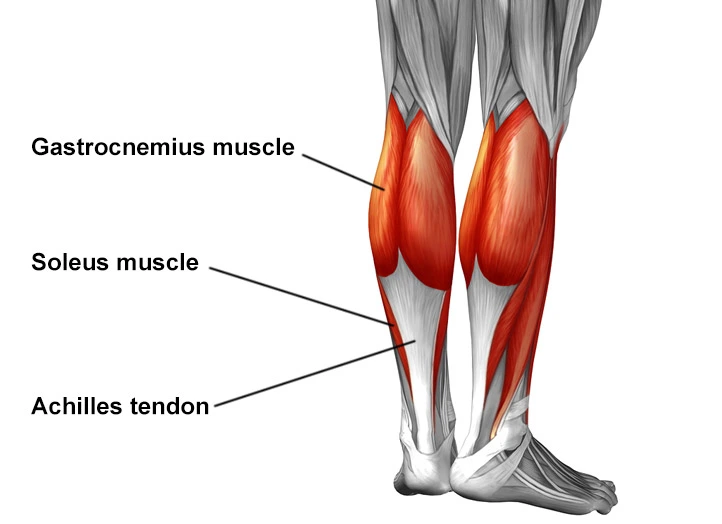
Heel and Calf Raises
The calf muscle is intricately linked to the hamstring muscle and the back of your knee joint or junction. Boosting the calf muscle will significantly help your hamstrings, and supply your knee joint with more excellent help and stability.
Stand barefoot (or wear stockings) on a 2-inch board or aerobic action. Put the toes and balls of your feet on the panel, with your heels on the ground. Create sure your body is level; you can grasp onto assistance like the wall or another stabilizing exterior. Lift vertically up as elevated as possible onto your toes and gradually lower down. Accomplish 10 recurrences and 2-3 sets, as required.
A significant deviation of this activity is to curve your toes inward (heels out from each other) and lift up vertically. This separates and boosts the internal part of your calf muscles. Then attempt shifting your toes out and obtain your heels close jointly, and extend up vertically. This will separate the outer part of the calves.
This is a fantastic workout that will help both your knees joints and ankles at the exact time.

Wall Squats
Stand in a standing position with your head, back, and hips against a wall, your feet around hip-width separated. Gradually twist your knee joint, and slide down the wall until only before you get a sitting position. Maintain the position for five to ten seconds and then gradually reached up. Reprise 5-10 times as required.
You should maintain your abdominal muscles committed and not permit your pelvis to glide down lower than your knee joints. Avoid getting the knees joints forward over the toes.
This quadriceps activity will strengthen your knee joint or junction and make energy along the whole leg.

Swimming
Fortunately, swimming is one of the finest exercises you can do to enhance bad knee joints. Walking water, backstroke, front crawling or only kicking laps with a flutter board will not solely firm your knee joint junctions but will provide you with a fantastic cardio exercise as well. Racing in water or water aerobics is another alternative you can test in a pool as well.
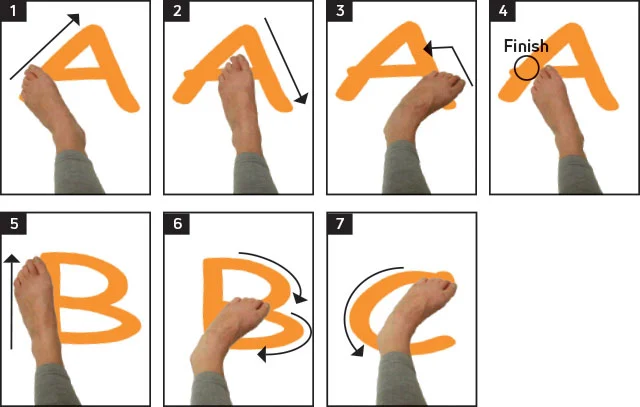
Ankle alphabet
This activity enhances the range of movement in your ankle. To do the activity, sit in a chair in a sitting position or sit on the floor with your knees flexed. Raise one leg barely off the floor, and make the letters of the alphabet with your foot. Run via all 26 letters, and then replicate with the further foot.
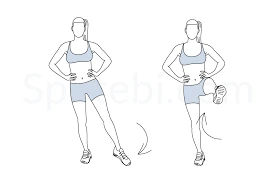
Single-leg balance
Balancing on one leg boosts your ankle joint or junction. Begin by standing on one leg solely while doing ordinary daily movements, like brushing your teeth or cleaning dishes. Over the period, add balance difficulties by standing on a foam pillow or BOSU balance instrument. Stand on one leg in a standing position for 30 to 60 seconds at a time.
Four-square drills
Make a square on the ground using tape, and separate it into a grid of four similar squares. Jump on one foot in the subsequent directions: front-to-back, side-to-side, clockwise, and anticlockwise. Accomplish almost 20 jumps per direction. Replicate with the other leg.
Resistance band work
Resistance from a latex band enhances your range of movement in numerous directions. Sit in a sitting position on the ground with your legs spread and cover the resistance band near the ball of one foot. Begin with your toes indicating straight up, and indicate them out from you for nearly 20 reps. Then, drag the toes toward your shin for 20 repetitions.
Evert your foot turns your toes to the side for about 20 repetitions, and then invert and turn your toes toward the midline of your body for 20 repetitions. Replicate on the opposite leg.
Heel-Toe walks
Heel-toe walks result in the muscles that cover the joint or junction to assist with stabilization and power. To accomplish the activity, find a long hallway or another matte stretch. Step on your heels just as you move ahead for four measures, then change to your tip-toes. Resume rotating this walking way for a minute or two.
Ankle circles
Ankle circles enhance mobility and range of movement in your ankle joint or junction. Sit in a sitting position on the ground with your knees flexed, or complete the activity while seated in a chair. Raise one leg and do 20-30 rings with your ankle in a clockwise order. Move gradually, actually working via the entire range of movement. Pause, then change orders for a similar number of repetitions. Reprise with the opposite leg.
Surgery
You will generally require an operation if:
- A ball of pus (abscess) forms. The pus in an abscess requires to be emptied.
- The infection presses on other essential structures. For instance, an infection in the spine may push on the spinal cord.
- The infection has evolved persistent (chronic) and some bone has been killed. The lifeless and infected bone may require to be released to permit the infection to remove. Occasionally plastic surgery is required at the exact time to protect any wound by providing the best option for cure.
- Infrequently, surgical reduction (amputation) of a foot or leg is required if the infection continues in a leg bone and does not obvious with any other therapy.
What are the complications of osteomyelitis?
Complications of osteomyelitis involve:
- Abscesses: Infection may extend to muscles and soft tissue, inducing abscesses. These bags of pus can seep through your skin. Patients with chronic osteomyelitis are more possible to have frequent abscesses. Treatment to empty these abscesses may just raise the risk of skin cancer.
- Bone death: Also known as osteonecrosis, bone dying can happen if swelling from the infection clips off blood flow to your bone. Very infrequently, this may conduct in the failure of a limb or amputation.
- Stunted growth: Osteomyelitis in a growing kid may hinder bone development.
- Early therapy, involving antibiotic therapy, is required to control the consequence of complications. Some difficulties which may occur with untreated or poorly treated osteomyelitis are:
- Septic arthritis
- Pathological fractures
- Squamous cell carcinoma
- Sinus tract formation
- Amyloidosis (rare)
- Abscess
- Bone deformity
- Systemic infection
- Contiguous soft tissue infection
Differential Diagnosis
The differential diagnosis for osteomyelitis is wide, and it is important to maintain these in mind during the evaluation of a person with a supposed bone infection. These differentials involve:
- Charcot arthropathy particularly in patients with diabetes
- Arthritis involving rheumatoid arthritis
- Metastatic bone disorder
- Fractures, involving pathological and stress fractures.
- Gout
- Avascular necrosis of the bone
- Bursitis
- Sickle cell vaso-occlusive pain crises
Outlook (Prognosis)
With management, the result for acute osteomyelitis is frequently good.
The outlook is more harmful to those with long-term (chronic) osteomyelitis. Symptoms may arrive and run for years, consistent with surgery. Amputation may be required, particularly in patients with diabetes or insufficient blood circulation.
The outlook for patients with an infection of a prosthesis trusts partly on:
The patient’s health
The kind of infection
Whether the infected prosthesis can be safely dismissed
What is the long-term outlook?
Most patients with osteomyelitis are treatable. Chronic infections of the bone, yet, may carry longer to manage and heal, particularly if they need surgery. Management should be forceful because an amputation can become essential sometimes. The outlook for this situation is suitable if the infection is managed early.
Prevention
If you’ve been informed that you have a raised risk of infection, talk to your doctor or physician about methods to control infections from happening. Decreasing your risk of infection will also allow your risk of creating osteomyelitis.
In general, accept precautions to avoid scrapes, cuts, and animal scrapes or bites, which provide germs comfortable entry to your body. If you or your kid has a little injury, clean the region instantly and use a clean bandage. Check injuries repeatedly for signs of disease.
Dos and Donts in Managing Osteomyelitis:
- Do carry the entire course of antibiotics.
- Do shift position in bed frequently to control pressure sores. Inspect the skin for redness at stress points.
- Do isometric activities frequently to control muscle weakness and support joint or junction flexibility.
- Do raise normal activities gradually after symptoms go out.
- Do help sterile bandages if you have an open injury. Wash hands before and after altering dressings.
- Do call your health care provider or doctor if the fever rises during therapy.
- Do call your health care provider or doctor if pain evolves unbearable.
- Do call your health care provider or doctor if a new abscess formation or drainage rises from an old abscess.
- Do see your health care provider or doctor if you have symptoms of infection anywhere in your body. This is very essential if you had a recent wound, are having dialysis, have diabetes, or inject medications.
- Don’t stop assuming antibiotics or alter your dosage because you feel more okay. If you quit too soon, the infection can return.
- Don’t dangle the involved limb. Maintain it barely increased.
- Don’t set weight on an involved leg. Crutches may allow for journeys to the bathroom.
FAQ
Who treats Osteomyelitis?
Osteomyelitis is managed by an orthopedic surgeon or doctor, but it should be handled by a multidisciplinary team involving infectious disorder experts, surgeons, and reconstructive surgeons or doctors along with microbiologists.
How does osteomyelitis of the jaws occur?
Osteomyelitis of the jaws is different; it appears in healthy grown-ups, is localized, is associated with the periodontal condition, and is frequently caused by anaerobic bacteria. But jaw fractures, periodontal disease, and penetrating wounds can be causative factors also. Chronic osteomyelitis of the jaw can happen with actinomycosis, tuberculosis, and syphilis. Special to the jaw is also osteomyelitis associated with sclerosis.
Can Osteomyelitis be prevented?
Yes, it can be controlled in some people by rehearsing rigorous infection management techniques, particularly before surgery. Understanding the areas of infection and the nearest eradication of the infection can benefit; for instance in diabetics; persistent infections which do not cause pain are originally ignored for a considerable quantity of time. Covering the feet and unraveling the right footwear to beneficial especially in controlling infections of the feet in diabetic people.
What wounds would be suspicious for osteomyelitis?
Suspicious injuries involve those that fell to the bone, joint, or junction or deep fascial cases. Typically, any damage close to the bone and over six months period should be doubted for osteomyelitis. When a record of damage that heals and then opens is likewise preceded by an episode of excessive warmth and abscess building, osteomyelitis should be presumed.
What is the major intervention for osteomyelitis?
Acute osteomyelitis must be managed surgically to empty pus and control bone necrosis. Antibiotics fitted to the people’s age and the organism is provided to prevent the hematogenous spread and to treat the local illness. In other terms, antibiotics protect life, and surgery assists to save bone.





3 Comments