GLOSSOPHARYNGEAL NERVE
INTRODUCTION :
The glossopharyngeal nerve, known as the ninth cranial nerve (CN IX), is a mixed nerve that carries afferent sensory and efferent motor information.
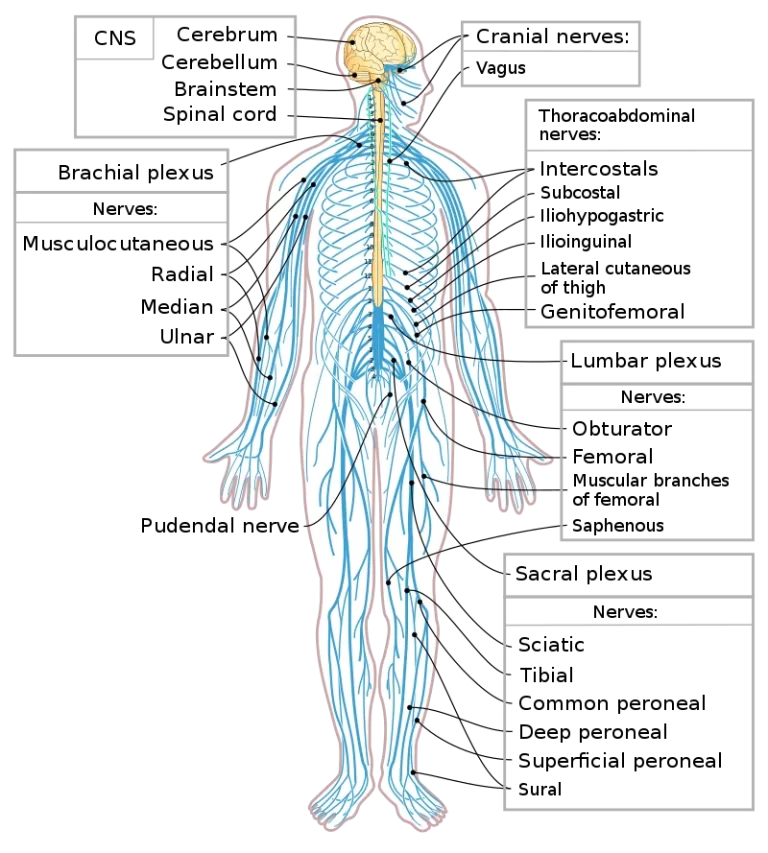
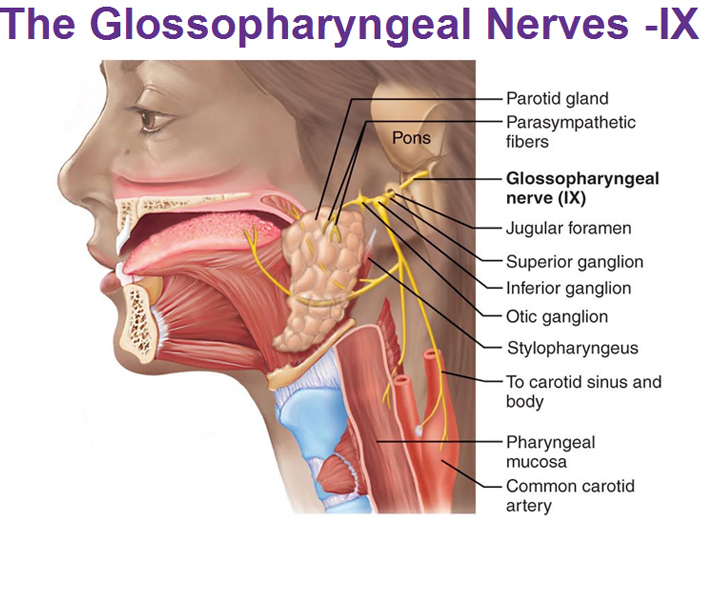
It exits the brainstem out from the sides of the upper medulla, just anterior (closer to the nose) to the vagus nerve.
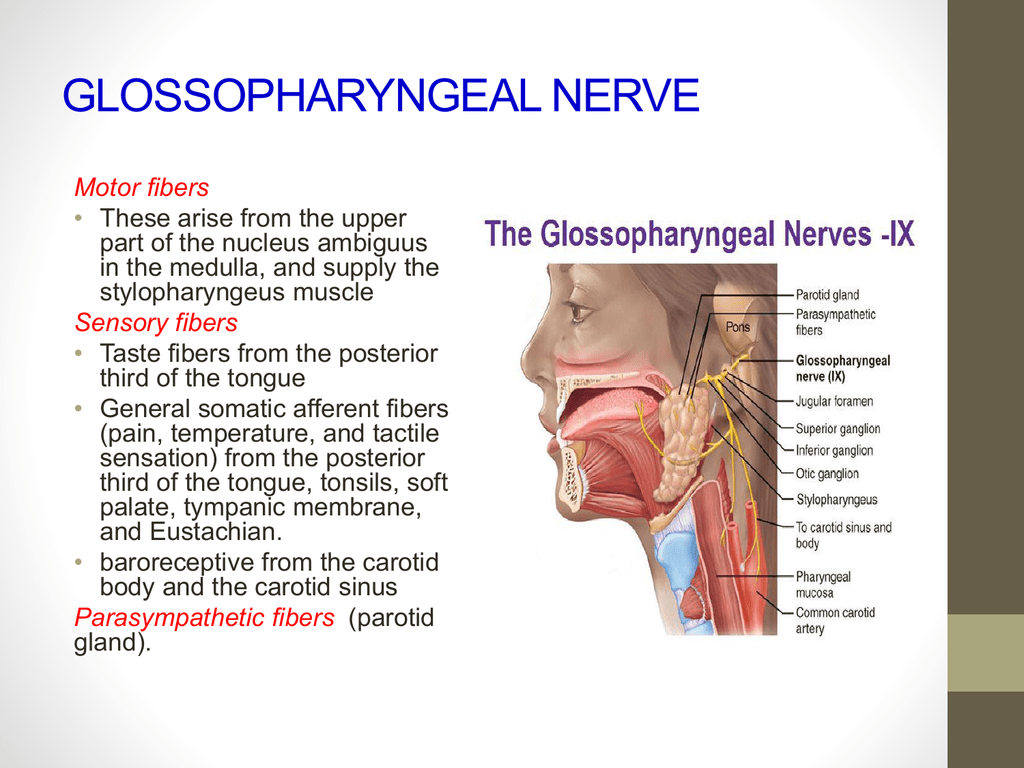
Sensory: Innervates the oropharynx, carotid body and sinus, posterior 1/3 of the tongue, middle ear cavity and Eustachian tube.
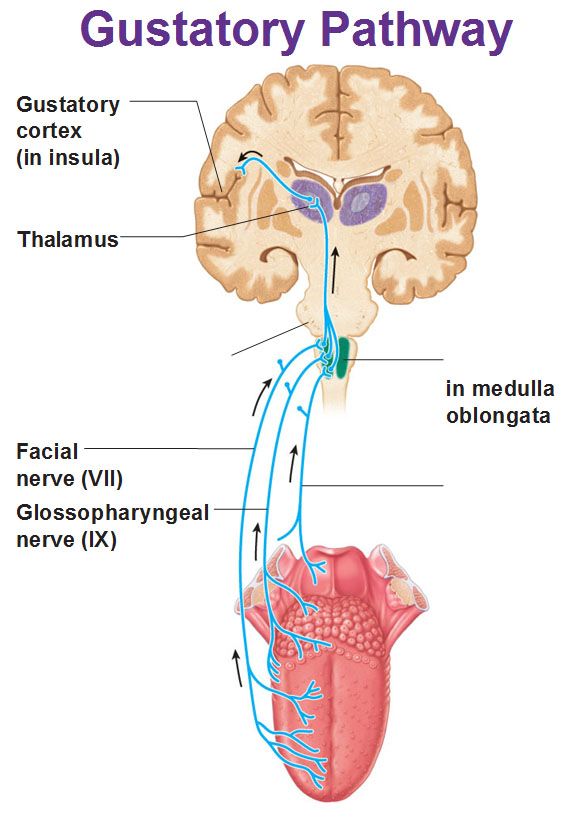
Special sensory: Provides taste sensation to the posterior 1/3 of the tongue.
Parasympathetic: Provides parasympathetic innervation to the parotid gland.
Motor: Innervates the stylopharyngeus muscle of the pharyna :
GLOSSOPHARYNGEAL NERVE ANATOMY :
ANATOMY OF GLOSSOPHARYNGEAL NERVE
The glossopharyngeal nerve originates in the medulla oblongata of the brain.
It emerges from the anterior aspect of the medulla, moving laterally in the posterior cranial fossa.
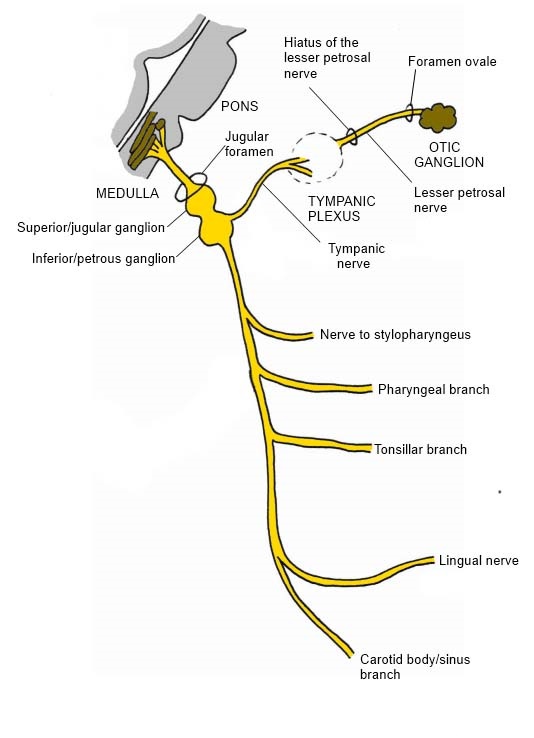
The nerve leaves the cranium via the jugular foramen. At this point, the tympanic nerve arises. It has a mixed sensory and parasympathetic composition.
Immediately outside the jugular foramen lie two ganglia (collections of nerve cell bodies).
They are known as the superior and inferior (or petrous) ganglia – they contain the cell bodies of the sensory fibres in the glossopharyngeal nerve.
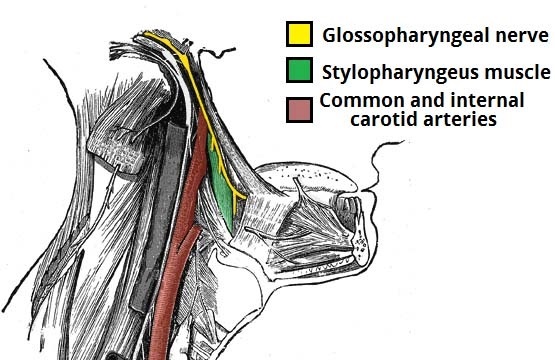
Now extracranial, the glossopharyngeal nerve descends down the neck, anterolateral to the internal carotid artery.
At the inferior margin of the stylopharyngeus, several branches arise to provide motor innervation to the muscle.
It also gives rise to the carotid sinus nerve, which provides sensation to the carotid sinus and body.
The nerve enters the pharynx by passing between the superior and middle pharyngeal constrictors.
Within the pharynx, it terminates by dividing into several branches – lingual, tonsil and pharyngeal.
GLOSSOPHARYNGEAL NERVE FUNCTIONS :
The glossopharyngeal nerve is a mixed nerve that contains both motor and sensory fibers.
It originates from the medulla oblongata, where the four of its nuclei are located.
Those nuclei give rise to the functionally diverse neuronal fibers that are involved in the motor and sensory functions of this nerve. These fibers are:
Somatic sensory : Which provide the sensory input from the posterior one-third of the tongue, palatine tonsils, oropharynx, mucosa of the middle ear, pharyngotympanic tube and the mastoid air cells.
Visceral sensory : That carry the sensory information from the carotid body.
Special sensory for the sense of taste from the posterior one-third of the tongue.
Parasympathetic :That innervate the salivary parotid gland.
Motor : Which innervate the muscles derived from the third pharyngeal arch, which are:
The stylopharyngeus muscle
The superior pharyngeal constrictor muscle
Special Sensory Function :
GLOSSOPHARYNGEAL NERVE FUNCTIONS
The glossopharyngeal nerve provides taste sensation to the posterior 1/3 of the tongue, via its lingual branch (Note: not to be confused with the lingual nerve).
Motor Functions :
The stylopharyngeus muscle of the pharynx is innervated by the glossopharyngeal nerve.
This muscle acts to shorten and widen the pharynx, and elevate the larynx during swallowing.
Parasympathetic Functions :
The glossopharyngeal nerve provides parasympathetic innervation to the parotid gland. These fibres originate in the inferior salivatory nucleus of CN IX.
These fibres travel with the tympanic nerve to the middle ear. From the ear, the fibres continue as the lesser petrosal nerve, before synapsing at the otic ganglion.
The fibres then hitchhike on the auriculotemporal nerve to the parotid gland, where they have a secretomotor effect.
COURSE AND RELATION :
COURSE AND RELATION CN IX
The glossopharyngeal nerve leaves the brainstem in a form of the several rootlets from the posterior lateral sulcus of the medulla oblongata, superiorly to the place of the exit of the vagus nerve.
The rootlets merge to form the body of the glossopharyngeal nerve, which courses forward and laterally, together with the vagus nerve and the accessory nerve.
It crosses over the jugular tuberculum and finally leaves the cranium through the anterior, narrow part of the jugular foramen.
Immediately outside the jugular foramen are placed two sensory ganglia that belong to the glossopharyngeal nerve, the superior and the inferior ganglia.
After passing through the jugular foramen, the glossopharyngeal nerve descends forward and inferiorly, aiming to the root of the tongue.
In that phase of its course, the nerve forms an arch that is placed superiorly and parallel to the arch of the hypoglossal nerve.
After this, the nerve passes between the stylopharyngeus muscle and the styloglossus muscle, enters the prestyloid space and then divides under the mucosa of the posterior one-third of the tongue, to its many branches.
Lateral branches :
The glossopharyngeal nerve, besides the anastomotic branches with the facial nerve, vagus nerve, and the sympathetic fibers, also gives off 5 lateral branches :
- The tympanic nerve – Jacobson
- The carotid sinus nerve
- The pharyngeal nerves
- Stylopharyngeus muscle nerve
- Tonsillar nerves
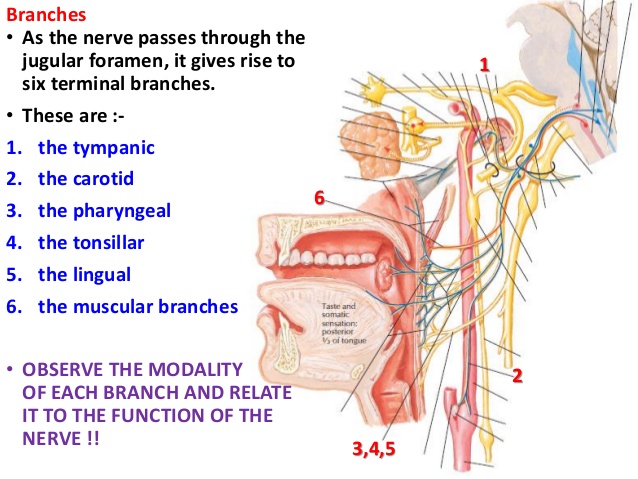
BRANCHES OF GLOSSOPHARYNGEAL NERVE
Tympanic nerve :
- This is the parasympathetic branch of the glossopharyngeal nerve that innervates the parotid gland.
- It separates from the glossopharyngeal nerve directly under the jugular foramen, and then it courses forward and laterally across the inferior side of the temporal pyramid, where it enters the tympanic canal.
- The nerve ascends upwards through this canal and enters the tympanic cavity.
- Inside the cavity, the tympanic nerve extends upwards by crossing through the promontory sulcus where it forms the neural tympanic plexus.
- Sympathetic caroticotympanic nerves that extend from the internal carotid plexus also participate in the making of the tympanic plexus, along with the branch of the facial nerve that is called the communicant branch with the tympanic plexus.
- The tympanic plexus sends branches that innervate the mucosa of the middle ear.
- From the superior part of the plexus, the lesser petrosal nerve rises.
- The lesser petrosal nerve then extends across this side of the temporal pyramid coursing forward and medially, all along the way being placed inside its groove called the sulcus of the lesser petrosal nerve.
- It passes through the sphenopetrosal fissure, and it finally ends in the otic ganglion.
- This is important because the lesser petrosal nerve carries the secretory parasympathetic fibers that synapse with the cells of the otic ganglion.
- In that way, the postganglionic fibers in a form of the auriculotemporal nerve reach the parotid gland and supply it with the parasympathetic innervation that is necessary for the proper stimulation of the gland.
Carotid sinus nerve :
- This nerve consists of the general visceral afferent fibers that serve for the reflex lowering of the blood pressure when it is increased.
- The carotid sinus nerve emerges from the glossopharyngeal nerve from about 0.4 inches (1 cm) beneath the basis of the cranium.
- It then descends along the body of the internal carotid artery aiming towards the bifurcation of the common carotid artery.
- This nerve ends by sending terminal branches to the carotid sinus and the carotid body.
Pharyngeal nerves :
- There are usually three of these nerves. They course medially, towards the pharynx.
- These branches create the anastomosis with the branches of the vagus nerve and as well as with the laryngopharyngeal nerves that originate from the cervical sympathetic plexus.
- With these anastomoses, these nerves build a neural network that is called pharyngeal plexus.
- The nerves of this plexus innervate many of the pharyngeal muscles, soft palate muscles and the mucosa of the pharynx.
Stylopharyngeus muscle nerve :
- This is the motor branch that provides the motor innervation for the stylopharyngeus muscle.
- It reaches the muscle from its lateral surface, in the part of the glossopharyngeal nerve course between the stylopharyngeus and the styloglossus muscle.
Tonsillar nerves :
- These nerves provide sensory innervation to the palatine tonsils and to the mucosa of the isthmus of the fauces.
CLINICAL RELEVANCE :
Damage :
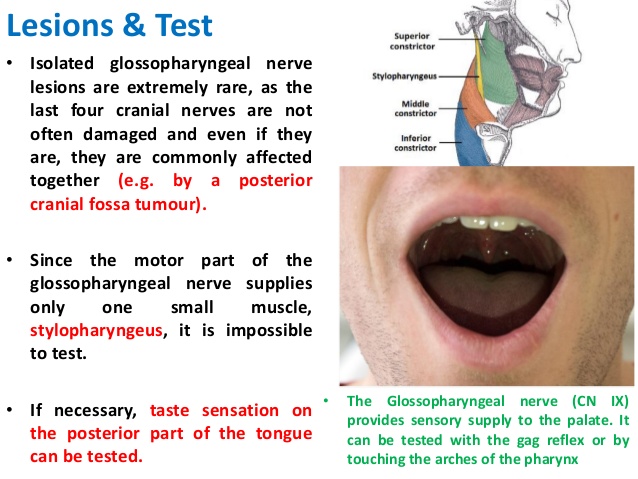
Damage to the glossopharyngeal nerve can result in loss of taste sensation to the posterior one third of the tongue, and impaired swallowing.
Examination :
The clinical tests used to determine if the glossopharyngeal nerve has been damaged include testing the gag reflex of the mouth, asking the patient to swallow or cough, and evaluating for speech impediments.
The clinician may also test the posterior one-third of the tongue with bitter and sour substances to evaluate for impairment of taste.
The integrity of the glossopharyngeal nerve may be evaluated by testing the patient’s general sensation and that of taste on the posterior third of the tongue.
The gag reflex can also be used to evaluate the glossphyaryngeal nerve.
Gag Reflex :
The glossopharyngeal nerve supplies sensory innervation to the oropharynx, and thus carries the afferent information for the gag reflex.
When a foreign object touches the back of the mouth, this stimulates CNIX, beginning the reflex.
The efferent nerve in this process is the vagus nerve, CNX.
An absent gag reflex signifies damage to the glossopharyngeal nerve.