Chondromalacia Patella and Physiotherapy Management
What is a Chondromalacia Patella?
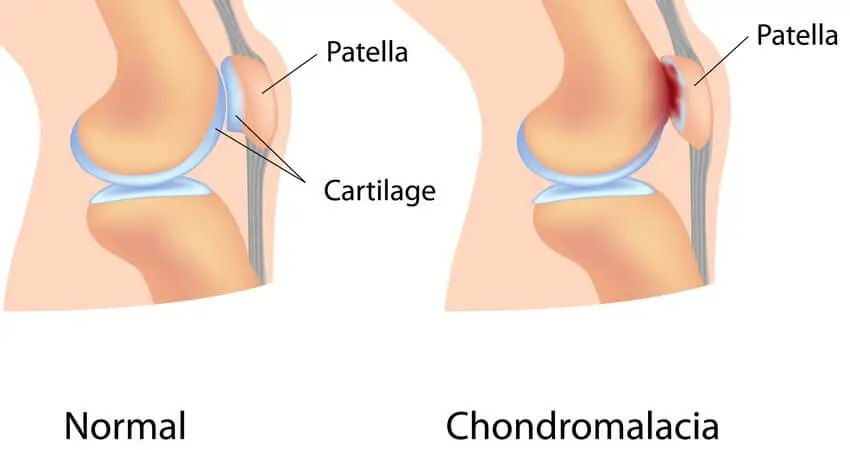
- Chondromalacia patellae, also known as “runner’s knee,” is a condition where the cartilage on the under-surface of the patella (kneecap) deteriorates and softens.
- This condition is common among young, athletic individuals, but may also occur in older adults who have arthritis of the knee.
- The articular cartilage of the posterior surface of the patella is going through degenerative changes which manifest as a softening, swelling, fraying, and erosion of the hyaline cartilage underlying the patella and sclerosis of the underlying bone.
Anatomy related to Chondromalacia Patella
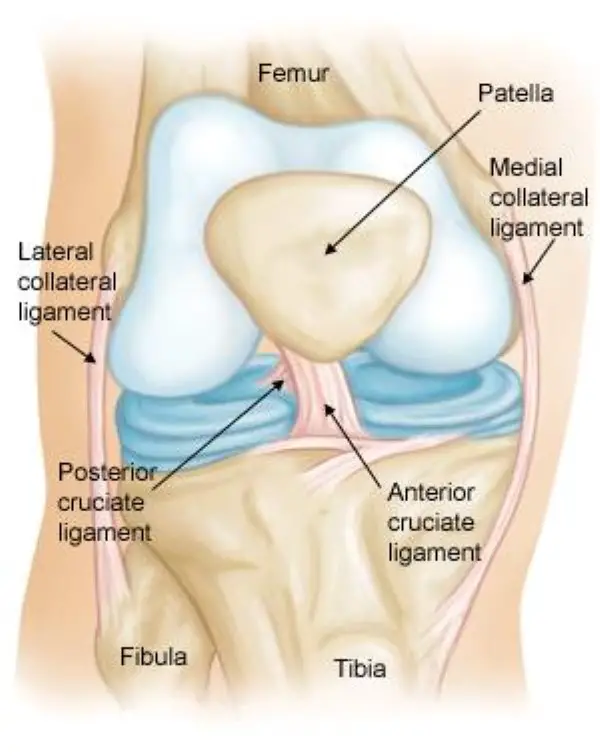
- The knee joint comprises 4 major bones: the femur, tibia, fibula, and patella. The patella articulates with the femur at the trochlear groove.
- Articular cartilage on the underside of the patella allows the patella to glide over the femoral groove, necessary for efficient motion at the knee joint.
- Excess and persistent turning forces on the lateral side of the knee can have a negative effect on the nutrition of the articular cartilage and more specifically in the medial and central area of the patella, where degenerative change will occur more readily.
- The quadriceps insert into the patella via the quadriceps tendon and are divided into four separate muscles: rectus femoris (RF), vastus lateralis (VL), vastus intermedius (VI), and vastus medialis (VM). The VM has oblique fibers which are referred to as the vastus medialis obliques (VMO).
- These muscles are active stabilizers during knee extension, especially the VL (on the lateral side) and the VMO (on the medial side). The VMO is active during knee extension but does not extend the knee. Its function is to keep the patella centered in the trochlea.
- This muscle is the only active stabilizer on the medial aspect, so its functional timing and amount of activity is critical to patellofemoral movement, the smallest change having significant effects on the position of the patella.
- Not only do the quadriceps influence the patella position, but also the passive structures of the knee. These passive structures are more extensive and stronger on the lateral side than they are on the medial side, with most of the lateral retinaculum arising from the iliotibial band (ITB).
- If the ITB is under excessive tension, excessive lateral tracking, and/or lateral patellar tilt can occur. This is can be a result of the tensor fasciae lata being tight, as the ITB itself is a non-contractile structure.
- Other significant anatomical structures:
- The femoral anteversion or medial torsion of the femur is a condition that changes the alignment of the bones at the knee. This may lead to overuse injuries of the knee due to malalignment of the femur in relation to the patella and tibia.
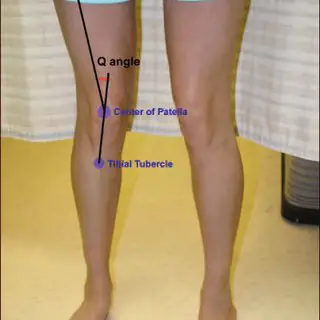
- The Q-angle: or quadriceps angle is the geometric relationship between the pelvis, the tibia, the patella, and the femur and is defined as the angle between the first line from the anterior superior iliac spine to the center of the patella and the second line from the center of the patella to the tibial tuberosity.
- If there is increased adduction and/or internal rotation of the hip, the Q-angle will increase, which increases the relative valgus of the lower extremity as well. This higher Q-angle and valgus will increase the contact pressure on the lateral side of the patellofemoral joint (which is also increased by external rotation of the tibia.
Causes of Chondromalacia patella
- The etiology of ChonromalaciaPatella is poorly understood, although it is believed that the causes of chondromalacia are injury, generalized constitutional disturbance, and patellofemoral contact, or as a result of trauma to the chondrocytes in the articular cartilage (leading to proteolytic enzymatic digestion of the superficial matrix).
- It may also be caused by instability or maltracking of the patella which softens the articular cartilage. Chondromalacia patella is usually described as an overload injury, caused by malalignment of the femur to the patella and the tibia.
Main reasons for patellar malalignment:
- Q-angle: An abnormality of the Q-angle is one of the most significant factors of patellar malalignment. A normal Q-angle is 14° for men and 17° for women. An increase can result in an increased lateral pull on the patella.
- Muscular tightness of:
- Rectus femoris: affects the patellar movement during flexion of the knee.
- Tensa Fascia late; affects the influence of the ITB
- Hamstrings: during running, tight hamstrings increase knee flexion which results in increased ankle dorsiflexion. This causes compensatory pronation in the talocrural joint.
- Gastrocnemius: tightness will result in compensatory pronation in the subtalar joint.
- Excessive pronation: prolonged pronation of the subtalar joint is caused by internal rotation of the leg. This internal rotation will result in malalignment of the patella.
- Patella Alta: this is a condition where the patella is positioned in an abnormally superior position. It is present when the length of the patellar tendon is 20% greater than the height of the patella.
- Vastus medialis insufficiency: the function of the vastus medialis is to realign the patella during knee extension. If the strength of VM is insufficient this will cause a lateral drift of the patella.
- A muscular balance between the VL and VM is important. Where VM is weaker the patella is pulled too far laterally which can cause increased contact with the condylus lateralis, leading to degenerative disease.
- Degenerative changes in the articular cartilage can be caused by
- Trauma: instability caused by previous trauma or overuse during recovery
- Repetitive microtrauma and inflammatory conditions
- Postural distortion: causes malposition or dislocation of the patella in the trochlear groove
- Hip positioning and strength are linked to the prevalence of patellofemoral pain syndrome. Therefore, hip strengthening and stability exercises may be useful in the treatment program of patellofemoral pain syndrome.
Stages of Chondromalacia patella
- In the early stages, chondromalacia shows areas of high sensitivity to fluid sequences. This can be associated with the increased thickness of the cartilage and may also cause oedema. In the latter stages, there will be a more irregular surface with focal thinning that can expand to and expose the subchondral bone.
- Stage 1: softening and swelling of the articular cartilage due to broken vertical collagenous fibers. The cartilage is spongy on arthroscopy.
- Stage 2: blister formation in the articular cartilage due to the separation of the superficial from the deep cartilaginous layers. Cartilaginous fissures affecting less than 1,3 cm² in an area with no extension to the subchondral bone.
- Stage 3: fissures ulceration, fragmentation, and fibrillation of cartilage extending to the subchondral bone but affecting less than 50% of the patellar articular surface.
- Stage 4: crater formation and eburnation of the exposed subchondral bone more than 50% of the patellar articular surface exposed, with sclerosis and erosions of the subchondral bone. Osteophyte formation also occurs at this stage.
- Articular cartilage does not have any nerve endings, so CMP should not be considered as a true source of anterior knee pain, rather, it is a pathological or surgical finding that represents areas of articular cartilage trauma or divergent loading.
Clinical features of Chondromalacia patella
- The main symptom of chondromalacia patellae is anterior knee pain, which is exacerbated by common daily activities that load the patellofemoral joint, such as running, stair climbing, squatting, kneeling, or changing from a sitting to a standing position.
- pain arising from the posterior aspect of the patella. Compression of the patella against the femoral condyle causes the pain The pain often causes disability affecting short-term participation in daily and physical activities.
- tenderness on palpating under the medial or lateral border of the patella, crepitation (felt with motion), minor swelling, a weak vastus medialis muscle, and a high Q-angle. A significant number of individuals are asymptomatic, but crepitation in flexion or extension is often present.
Differential Diagnosis
- Chondromalacia patellae
- Osteochondritis dessicans
- Patellofemoral osteoarthritis
- Patellofemoral pain syndrome
- Lateral patellar compression syndrome
- Plica syndrome
- Quadriceps tendonitis/tendinopathy
- Patellar tendonitis/ tendinopathy
- Saphenous neuroma
- Postoperative neuroma
- Patellar fat pad inflammation
- Hoffa disease
- Patella Alta
- Patella Baja
- Patella instability
- Bi-partite patella
Diagnosis of Chondromalacia patella
- The primary diagnostic approach for chondromalacia patellae is radiography with added arthrography. Pinhole scintigraphy, part of arthrography, is also used to diagnose the condition. MRI is an effective, non-invasive method with the ability to increase the sensitivity and specificity of the diagnosis.
Examination
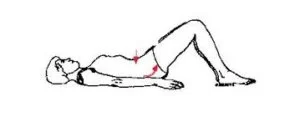
- Examination of the knee is 4 fold: observation, mobility, feel, X-ray.
Observation
- joint appearance is usually normal, but there may be a slight effusion.
Effusion test:Patellar tap test
- The patient is lying in supine with the leg extended. The physiotherapist puts pressure on the proximal side of the knee in an effort to squeeze the fluid out of the suprapatellar pouch.
- The fluid can be moved under the patella while maintaining the pressure on the suprapatellar pouch; the therapist uses his/her other hand to press upon the medial and lateral recesses forcing the fluid under the patella.
- Tapping down the patella with the index creates an upward and downward movement and a palpable ‘click’ as the patella hits the underlying femur.
- If the test is negative the femur and the patella are already in contact.
- A positive test is when the patella can be felt to move down through the fluid and rebounds on the patella. The test can be falsely positive, therefore we must always test both sides to compare
- Mobility: passive movements are usually full and painless, but a repeated extension of the knee from flexion will produce pain and a grating feeling underneath the patella, especially if the articular surfaces are compressed together.
- Feel: Pain and crepitus will be felt if the patella is compressed against the femur, either vertically or horizontally, with the knee in full extension. By displacing the patella medially or laterally, the patellar margins and their articular surfaces may be felt.
- Tenderness of one or other margin may be elicited and more frequently the felt medial. Resisting a static quadriceps contraction will generally produce a sharp pain under the patella. This may be apparent in both knees, but more severe on the affected side.
- X-ray: an AP view of the patellofemoral joint is needed to detect any radiological change. In all but the most advanced cases, there is no convincing radiological change. In the latter stages, patellofemoral joint space narrows, and osteoarthritic changes begin to appear.
Medical Management of Chondromalacia patella
- Exercise and education are two important aspects of a treatment program. Education helps the patient to understand the condition and how they should deal with it for optimal recovery.
- If conservative measures fail, there are a number of possible surgical procedures.
- Chondrectomy: also known as shaving. This treatment includes shaving down the damaged cartilage to the nondamaged cartilage underneath. The success of this treatment depends on the severity of the cartilage damage.
- Drilling is also a method that is frequently used to heal damaged cartilage. However, this procedure has not so far been proven to be effective. More localized degeneration might respond better to drilling small holes through the damaged cartilage. This facilitates the growth of healthy tissue through the holes from the layers underneath.
- Full patellectomy: This is the most severe surgical treatment. This method is only used when no other procedures are helpful, but a significant consequence is that the quadriceps will become weak.
- Two other treatments may be successful.
- Replacement of the damaged cartilage: The damaged cartilage is replaced by a polyethylene cap prosthesis. Early results have been good, but the eventual wearing of the opposing articular surface is inevitable.
- Autologous chondrocyte transplantation under a tibial periosteal patch.
- Simply removing the cartilage is not a cure for chondromalacia patellae. The biomechanical deficits need addressing and there are various procedures to aid in managing this.
- Tightening of the medial capsule (MC): If the MC is lax, it can be tightened by pulling the patella back into its correct alignment.
- Lateral release: A very tight lateral capsule will pull the patella laterally. The release of the lateral patellar retinaculum allows the patella to track correctly into the femoral groove.
- The medial shift of the tibial tubercle: Moving the insertion of the quadriceps tendon medially at the tibial tubercle, allows the quadriceps to pull the patella more directly. It also decreases the amount of wear on the underside of the patellar.
- Partial removal of the patella
- Although there is no overall agreement for the treatment of chondromalacia, the general consensus is that the best treatment is a non-surgical one.
Physiotherapy management of Chondromalacia patella
Pain-relieving modality
- TENS: transcutaneous electrical nerve stimulation is an electrical modality that provides pain relief by providing pain modulation.TENS closes the gate mechanism at the anterior grey horn in the spinal cord. also stimulates the endogenous opioid system which prevents the release of substance p at the anterior grey horn.
- SWD: short wave diathermy is a deep heating modality that uses heat to provide pain relief, it improves the blood supply to targeted muscles, and removal waste products.
- IFT: Interferential current therapy produces a low-frequency effect at targeted tissue, it inhibits transmission of pain impulses, stimulates the endogenous opioid system, increases blood supply, relieves edema, and removes the waste products.
- Cold therapy: used to relieve inflammation and reduce pain, Ice Massage- Ice on the area of inflammation for anti-inflammatory effects. Use ice in a paper or Styrofoam cup (peeled away) for 5-7 minutes, make sure to avoid frostbite.
initial if the knee is too painful, the knee is immobilized in a pop cylinder cast.
- the exercise program includes gentle isometric quadriceps contraction assisted single-leg to raise strong hip ankle-foot movements and relaxed passive or active knee swinging to maintain a full range of motion.
- stretching exercise for rectus femoris, hamstring muscle, gastrocnemius, and tensor fascia lata.
- strengthening exercise of the vastus medialis oblique muscle.

- Patellar taping: Taping the patella to influence its movement may provide some short-term relief, but the evidence is varied. A commonly used technique is ‘McConnell taping or Kinesio taping.
- knee braces: Supporting the patella and knee joint by bracing is a further way to reduce pain and symptoms, but it will also alter patella tracking and reduce the active function of the quadriceps.
- Bracing may be useful in the short term to offer patients some support and pain relief to help them avoid antalgic movements and normalize gait as much as possible.
- Bracing can also be used for patients pre- and postoperatively, but a brace should allow variation in a medial pull on the patellar and pressure.
- Wearing a patellar realignment brace and following physical therapy has a synergistic effect on patients with chondromalacia patellae
- Foot Orthoses
- Foot orthoses are another option for pain relief, but only in cases where lower limb mechanics are deemed to be contributing to the knee pain, which may be due to:
- Poor pronation control,
- Excessive lower limb internal rotation during weight-bearing
- An increased Q-angle
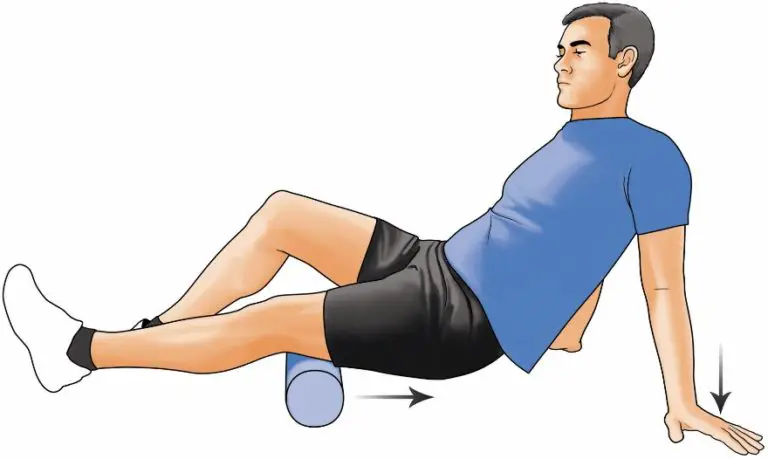
- Foam Roller
- Using a foam roller can be useful for relieving tight musculature and reducing pressure over the patella
- Foam roller exercise for hamstring muscle
- foam roller exercise for gastrocnemius muscle
- foam roller exercise for iliotibial band and tensor fascia lata.
Epidemiology
The higher Q angles in women are thought to be the reason why more women than males are impacted. The variance does not seem to have a hormonal explanation.
A greater incidence of chondromalacia is seen in active young adults who play running sports or in workers who put more stress on their patellofemoral joint by often stair climbing and/or kneeling.
Prognosis
Patellofemoral osteoarthritis may develop from chondromalacia patellae, or it may be reversible. Individuals who suffer from chondromalacia patella-related pain in the knee frequently heal completely.
Recovery might take years or as little as a month, depending on the circumstances. Because their bones are still developing and their symptoms usually get better as they become older, teenagers frequently make long-term recoveries.
Complications
Patients with chondromalacia patella may experience secondary complications from the use of NSAIDs (e.g., gastrointestinal symptoms) or from bracing, wherein the skin reacts to the brace material sometimes, leading to dermatological responses.
Rarely do therapeutic exercises exacerbate symptoms.
The patient, the doctor, and the therapist should collaborate to change the activity if it is associated with worsening symptoms. This may involve changing the activity’s frequency, length, or intensity, or temporarily stopping it if needed.
Best Doctors for CMP
- Orthopedist
- Physical therapist
- Radiologist
- Rheumatologist
Patient Education
Patient education focuses on following prescribed dosages, doing therapeutic exercises, recovering from surgery, and avoiding any activities or movements that cause pain when at all possible.
Conclusion
Chondromalacia patella, or “runner’s knee,” is a condition involving the deterioration of the cartilage beneath the kneecap. The severity and reaction to therapy determine the prognosis. Conservative measures like rest, physical therapy, and activity modification are often effective.
Surgical options may be explored in some circumstances. Long-term management may involve ongoing exercises and lifestyle adjustments. Consulting with a healthcare professional for an individualized plan is crucial.
FAQ
What is the best treatment for chondromalacia patella?
Initially, chondromalacia patella is treated with straightforward conservative measures. It’s possible that you’ll be told to rest your knee and prevent doing anything that might put a strain on it. To treat pain and minimize swelling, your doctor could recommend anti-inflammatory medications and opioids with combination of Physical therapy.
Is chondromalacia patella serious?
Rarely is chondromalacia patella a serious condition. In actuality, with rest, elevation, ice, and stretching, the majority of individuals can handle it. Nevertheless, in certain individuals, the condition may deteriorate to the extent where nonprescription analgesics and alternative home remedies are inadequate to alleviate discomfort.
Can chondromalacia be cured without surgery?
Nonsteroidal anti-inflammatory medicines (NSAIDs) and rest are the most common over-the-counter pain relievers for chondromalacia. Occasionally, physical treatment is advised; surgery is advised less frequently.
What age is chondromalacia patella common?
Patients with chondromalacia patella are often young, between the ages of 15 and 35, and many of them lead busy lives. The condition’s symptoms, which include recurring knee effusion, knee instability, and crepitus, can be quite debilitating.
What is the fastest way to heal chondromalacia?
The standard therapy for this issue is non-operative. To treat your chondromalacia patella, you might need to see a physical therapist for four to six weeks, followed by many additional months of at-home stretching and strengthening exercises. The first stage is managing the discomfort and inflammation.
Is walking good for chondromalacia patella?
The ideal exercises are those with little impact, like swimming or walking on level ground.
Can you fully recover from chondromalacia?
As articular cartilage repairs slowly, chondromalacia is typically a lifelong condition. However, knee discomfort may frequently be relieved in a few months with nonsurgical therapy. In the event that nonsurgical therapy is unsuccessful, your physician may operate to remove the affected cartilage.
References
- Habusta, S. F. (2023, April 22). Chondromalacia Patella. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK459195/




4 Comments