GLUTEAL TENDINOPATHY: Physiotherapy Treatment
What is gluteal tendinopathy?
The gluteal tendinopathy is characterized by a dull, aching, constant pain that is exacerbated by activity, especially when the hip is flexed. The pain is thought to be associated with the presence of a hematoma in the tendon. The pain may radiate proximally (into the thigh or lateral epicondyle) and distally (into the buttocks).
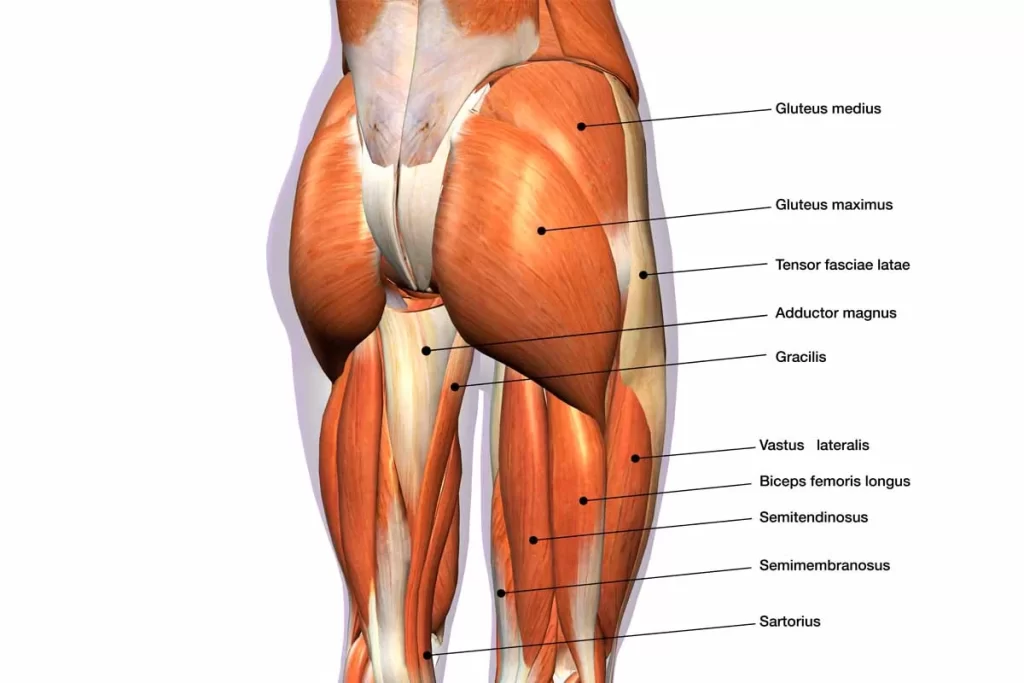
The gluteal muscles are a group of three muscles which make up the buttocks, the gluteus maximus, gluteus medius, and gluteus minimus. The three muscles originate from the ilium and sacrum and inserted on the femur. The functions of the muscles include extension, abduction, external rotation, and internal rotation of the hip joint’
Gluteal Tendinopathy (GT) is defined as moderate to severely disabling pain over the Greater Trochanter (lateral hip pain) with marked palpation tenderness over the greater trochanter. This condition generally affects inactive people but can also be a problem in athletes, especially runners, with one in four females over 50 years likely to be affected.
The pain can at times prefer into the lateral thigh,It is often referred to as Greater Trochanter Pain Syndrome (GTPS) and was traditionally diagnosed as Trochanteric Bursitis, however, recent research defines non-inflammatory tendinopathy of the gluteus medius(GMed) and/or gluteus minimus (GMin) muscles to be the main source of lateral hip pain.
GT has significant impacts on the quality of life, with similar symptoms to those of hip OA and interferes with sleep (side lying) and common weight bearing tasks. Sadly, there is no optimal treatment approach for this condition.
Pathoanatomy/Pathomechanics
-Tendon structure and loading capacity are influenced by mechanical loading which triggers physiological responses within the tendon. Under normal conditions, the tendon undergoes a cycle of balanced catabolic and anabolic processes. Changes in loading type, intensity or frequency disrupt this harmony. Eccentric contractions in outer ranges (when the muscle is active and the tendon is lengthening simultaneously) and where potential compression can occur, represent the greatest form of loading. Failure to adapt to loading, due to rapid increase in intensity and/or frequency with insufficient recovery time, results in a series of catabolic effects which in turn result in altering tenocyte behaviour, reducing load-bearing capacity and predisposing tendons to injury at relatively low tensile loads. A combination of both tensile loading and compression are found to be the most damaging.
What are the causes of gluteal tendinopathy?
Gluteal Tendinopathy causes vary from person to person, one or more causes may involve in Gluteal tendinopathy.
Following common causes are involved :
- Hypermobile Individual can lead to overload gluteal muscles- tendinopathy.
- Limb-length discrepancy.
- Other Joint pain such as ankle pain, knee pain, hip Pain or pelvic problems following injuries or operations or some kind of instability in these joints can lead to abnormal or excessive loading in the gluteal tendons leading to pain and tendinopathy.
- Biomechanical changes in the lower-limb which can alter the gait cycle, runner’s and even daily movements in individuals, along with certain muscle imbalances secondary to those biomechanical changes can lead to excessive loading in the glutes muscles which can lead to tendinopathy.
- Finally, purely muscle imbalances arising from less use of certain muscles in the lower extremities or excessive loading to other muscles due to high demand (especially in sports person) can once again lead to imbalances putting the gluteal muscles strain which are unable to withstand, leads to tendinopathy.
Symptoms of Gluteal Tendinopathy:
Lateral hip pain with an insidious onset, that gradually worsens overtime with different loads and tasks is the main feature of GT. Other symptoms include

-Tender lateral hip when palpated, especially near the greater trochanter.
-Pain with side-lying on the problematic side.
-Pain with weight-bearing activities such as walking, climbing stairs, standing and running.
-Pain may refer to the lateral thigh and knee.
-Pain with prolonged sitting.
-Sitting with crossed legs increases pain.
-Pain can also occur when lying on the non-painful side if the painful hip falls into adduction.
-Weak hip abductors.
Diagnosis criteria
-A thorough hip examination is needed basically by obtaining the patient’s history to understand the nature of the symptoms, And some clinical test are there to confirm hip abnormality.
Gluteal tendinopathy test :
The following test is useful in the Diagnosis of Gluteal tendinopathy.
1. FABER test:
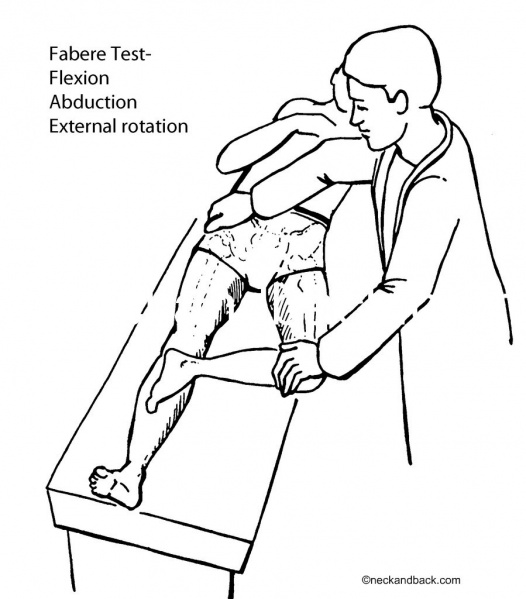
Flexion/Abduction/External Rotation. Tension in this test is specific to the anterior portions of the GMed and GMin. The test is positive when pain is experienced over the lateral hip. It assists with differentiating between hip OA and GTPS.
2.(30 second) single leg stance test:

The person being tested must stand, unassisted, on one leg with their eyes open and one finger on a wall. As soon as the person’s foot is lifted of the floor, the 30 seconds start. This test has been shown to have a specificity of 100%, sensitivity of 38% and positive predictive value of 100%, indicating that if the test was positive there was an extremely high likelihood that GT was present on MRI. Grimaldi and Fearon (2015) suggest holding the position for 30 seconds or until reproduction of symptoms.
3. Resisted external de-rotation test and modified external de-rotation test
The patient lies in supine and the examiner then passively flexes the hip to 90° with external rotation. The hip should be in neutral abduction/adduction. Slightly reduce the external rotation to decrease the compression of the tendon. The patient then actively rotates their leg to neutral against the therapist’s resistance.
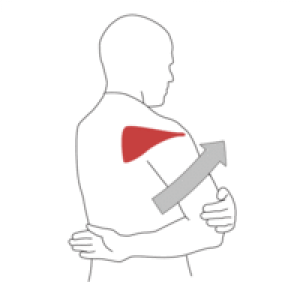
4.Hip FADER: (FADER=Flexion/Adduction/External Rotation).
The therapist passively takes the limb into 90° hip flexion, adduction and external rotation to end of range. This test aims to position the ITB over the greater trochanter and positions the GMed and GMin tendons under tension with the ITB fascia against the greater trochanter. Test is positive if the patient experienced pain (=2/10) on the Numeric Rating Scale (NRS) over the lateral hip. The reported specificity and positive predictive value (PPV) of this test are 86.67% and 88.24% respectively when compared with an MRI imaging.
5. Passive end-of-range hip adduction in side lying (ADD) test.
In the side lying position, the lowermost hip and knee flexed 80-90°, and the uppermost leg supported by the examiner with the knee extended, in neutral rotation, and the femur in line with the trunk. The anterior superior iliac spines are aligned vertically in the frontal plane. The examiner passively moves the hip into end range hip adduction with overpressure, while maintaining the pelvis stable with the other hand. This test compresses the lateral insertions of the gluteal tendons, and a positive response is felt over the lateral hip.
6. Palpation:
Palpation has been shown to be most sensitive, but least specific for clinically diagnosing GT. Palpation should be done over the anterior, lateral or posterosuperior facets of the greater trochanter (GMed and GMin tendon insertions) bilaterally. The patient should assume a side-lying position with the asymptomatic side at the bottom, hips flexed 60°and knees together. A positive test indicates pain and tenderness.
Treatment for gluteal tendinopathy :
Pain-relieving Analgesics like NSAIDs eg. Aceclofenac, Diclofenac are used to relieve pain.
Rest, Hot Pack / Ice Pack are also used to relieve pain.
Physiotherapy Treatment :
Pain-relieving electrotherapy modalities like TENS, IFT (Interferential Therapy ), Ultrasound therapy are used according to symptoms.
Ergonomics :
-Load management: Loading management for GT should include education on positions and activities that can increase compressive load on the gluteal tendons. Patients with GT should:
[Avoid sitting with their legs crossed]
[Avoid sitting with knees together]
[Avoid standing while hanging on one hip]
[Avoid lying on the affected side]
[Place a pillow between their knees and shins when lying on the unaffected side to limit adduction of the affected hip]
[Stop adduction stretching (for glutes and ITB) to limit compression of the gluteal tendons]
Exercises for gluteal tendinopathy :
Isometric exercise training:
-Isometric contractions activate segmental and extrasegmental descending pain inhibitory pathways. Sustained low-intensity contractions (25% maximum voluntary isometric contraction) are more effective in raising pain pressure thresholds.
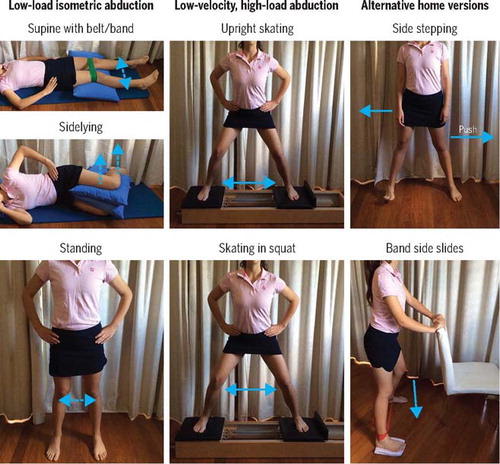
1.Low-load isometric abduction.
2.Low-velocity, high-load abduction.
3.Alternative home version.
Isotonic Loading training
-This phase is to commence once pain is under control and should include slow, progressive isotonic loading and strength endurance.
- The internal rotation hip strengthening exercise-
-The patient needs to be in a sitting position. An elastic resistance strap is used to do this exercise. The patient is sitting on the table. The elastic resistance strap is attached to the table leg 10 cm above the ground. The other side of the resistance strap is attached around the foot of the patient’s affected hip. The patient performs an internal rotation. The patient should perform three sets of 20 repetitions on both the affected and unaffected side.
2. The external rotation hip strengthening exercise-Same position as internal rotation but now the patient performs an external rotation. The strap is used to stabilize the thigh to prevent sagittal and frontal plane hip motion.
3. The side-lying abduction/external rotation exercise-
The patient lies on the table on his/her side with the hip in approximately 45 degrees of flexion (the elastic resistance strap surrounds the knees).The patient performs an abduction with his upper leg. He slowly lowers his leg: at this point the hip abductors contract eccentrically. [3] The patient should perform this exercise three sets of 20 repetitions on the affected side and two sets of 20 repetitions on the unaffected side. The side-lying abduction exercise should be performed daily for 2 weeks.
4. Weight-bearing hip strengthening exercise-
The patient is standing against the wall on one leg. The patient bears his weight on the affected side en he/she performs a series of mini-squats. The patient should maintain the external rotation of the affected hip so that the hip remains over the lateral portion of the foot/leg which is bearing the weight. This exercise should be performed two or three times a week with three sets of 20 repetitions on the affected side and two sets of 20 repetitions on the unaffected side.
5. Stretching program-
The patients need to stretch daily. The main stretches are: stretching of the hip flexor, the quadriceps, the lateral hip/piriformis and the hamstring muscles. The patients should perform more stretches on the affected side than on the unaffected side. They have to repeat them as often as they can throughout the day. They should keep stretching their muscles as long as they’re in pain.
Do’s and Don’ts:
Do:
- Always stand with your weight evenly distributed between both feet.
- Walk with a slightly wider base so your feet don’t come towards the mid-line.
- A walking stick can sometimes be useful in more severe cases in the early stages.
Do Not:
- Sleep on your side: it is best to sleep on your back with a pillow under your knees, but if you really find this impossible, sleep on the non-affected side with a pillow between your legs to keep them parallel ( don’t let the affected leg fall towards the other ).
- Cross your legs when you are sitting ( either one ).
- “Hang on one hip” – standing leaning most of your weight through one leg




3 Comments